Antegrade nailing
1. Principles
General considerations
Acute and pathological fractures can be nailed. The best indications for humeral shaft nailing are fractures located between the surgical neck and approximally 5 cm above the olecranon fossa.
There are many different nails on the market; the main difference between them relates to their nail design (straight vs bent nails) and their locking configurations. Some nails allow compression at the fracture site.
To demonstrate the principles, the illustrations below show the use of a straight nail. Some details may not be applicable with other nailing systems.
For antegrade nailing with a bent nail click here.
See also the discussion of bent vs straight nails.
Note on illustrations
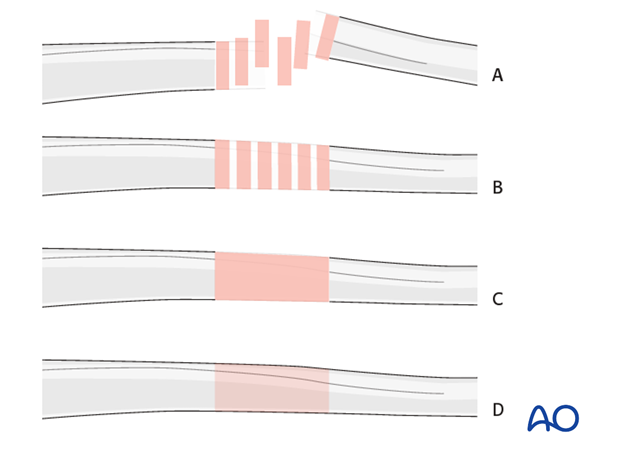
In some illustrations generic fracture patterns are shown, as four different types:
A) Unreduced fractureB) Reduced fracture
C) Fracture reduced and fixed provisionally
D) Fracture fixed definitively
Open fractures in the humeral shaft
Adequate surgical debridement is the crucial first step in the care of any open fracture.
Read more about the treatment of open fractures in the humeral shaft.
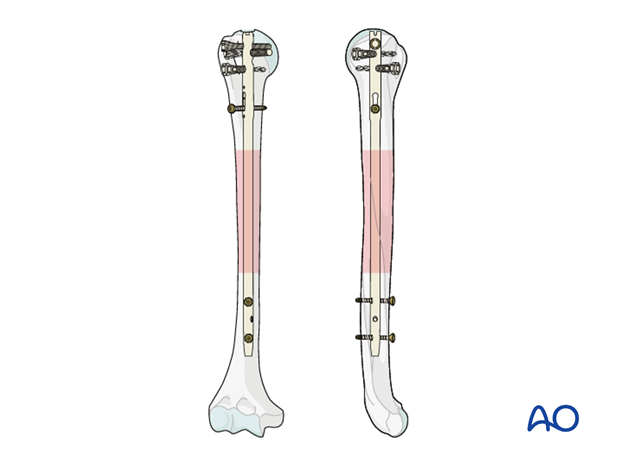
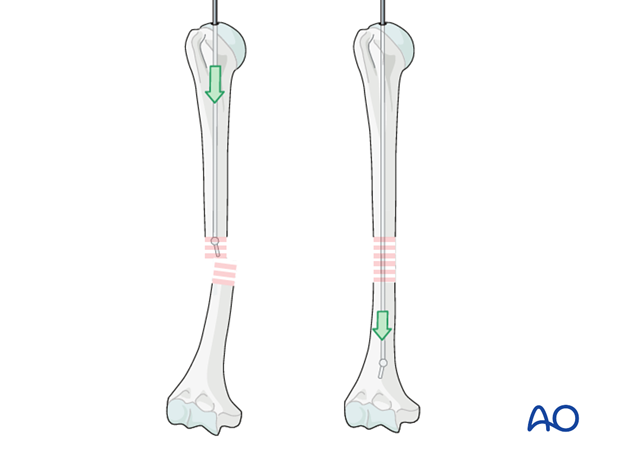
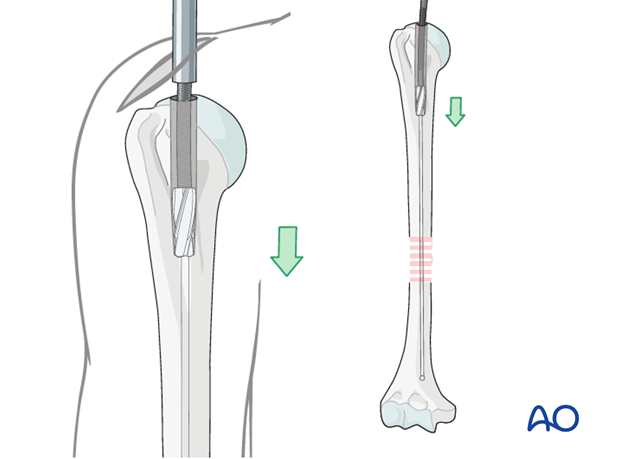
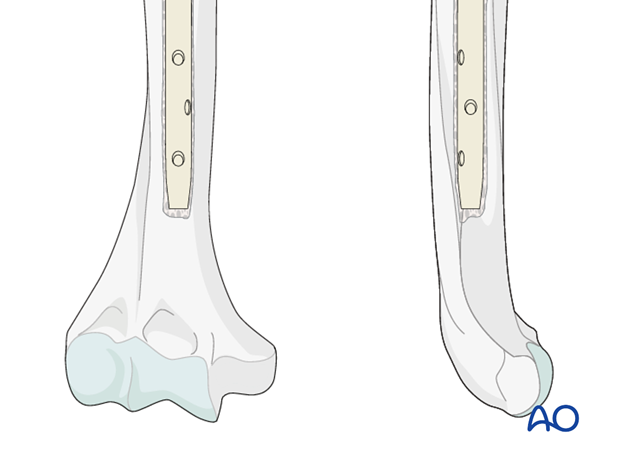
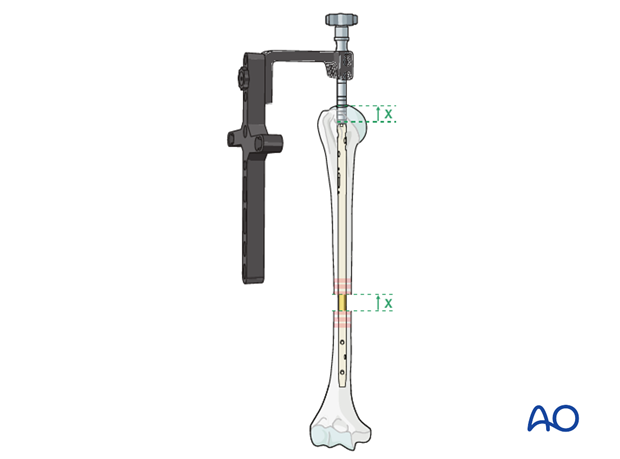
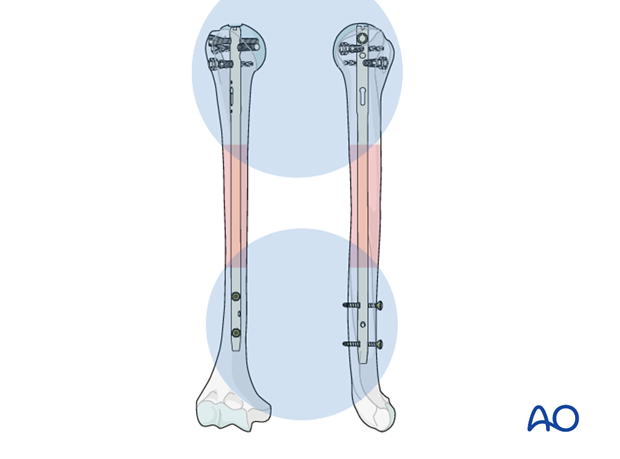
Interlocking
In general, static interlocking with at least two screws on each side of the fracture is recommended. Depending on the fracture morphology/extension and the bone quality, additional locking screws may be used.
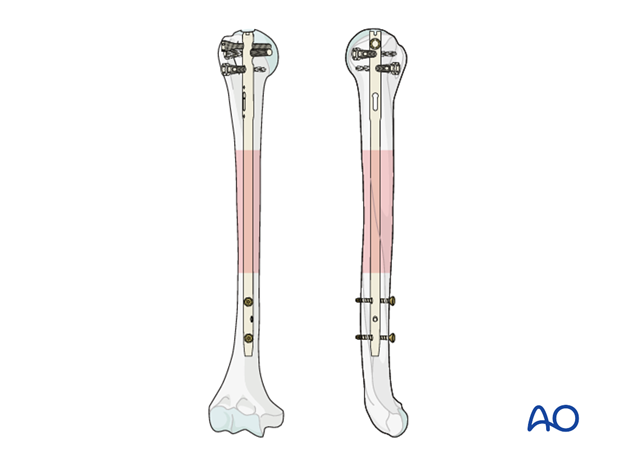
If an anatomic reduction is obtained it is easiest to start with the proximal interlocking of the nail (left).
If retrograde closure/compression of the fracture site is intended, start with the distal interlocking to allow for later retrograde movement of the nail (right). In this case the top of the nail should be inserted into the humeral head far enough for it to remain below the articular surface after fracture reduction.

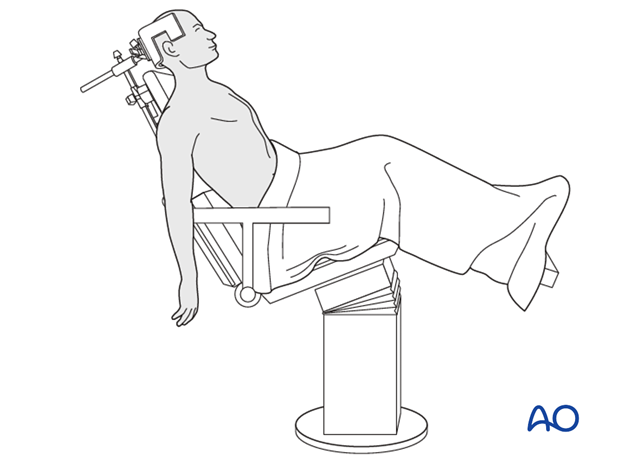
2. Patient preparation and approach
Patient positioning
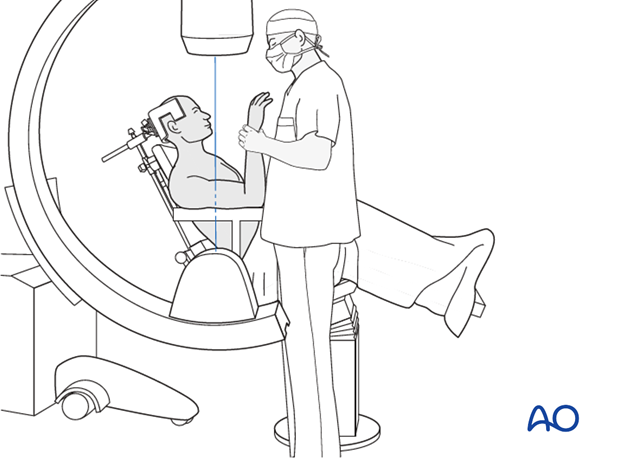
For antegrade nailing, the beach chair is the preferred position.
If no beach chair is available, a supine position may be used.
Approach to entry point
The entry point is accessed through an antegrade nailing approach.
3. Determining nail diameter and length
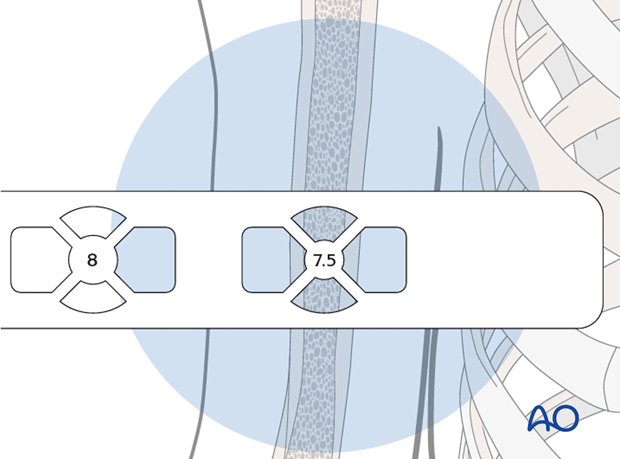
Nail diameter
Place a radiographic ruler anteriorly on the upper arm over the medullary canal.
Visualize the medullary canal under image intensification in AP view and compare with the diameters of the marks on the ruler.
The correct diameter of the humeral nail corresponds to the diameter of the mark that fits completely into the medullary canal. Look carefully at the distal humeral canal. It may be narrower than the rest. If the isthmus is very narrow, consider reaming to allow the insertion of a larger diameter nail.
In our example, a nail of 7.5 mm diameter is chosen.
The diameter of the medullary cavity can also be measured on digital x-rays of the humerus. Take care to estimate the diameter on the narrowest site.
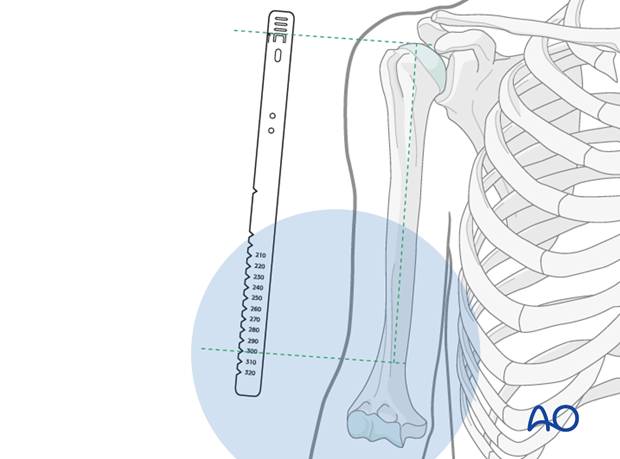
Nail length
Provisionally reduce the humeral fracture.
Place the ruler parallel to the arm, with the top-of-nail mark at the level of the anticipated insertion site in the humeral head.
Take an AP image intensifier view of the distal humerus together with the ruler.
The humeral nail should be as long as possible in the distal canal, consistent with its diameter. Determine this length with the aid of the ruler.
Keep in mind that the top of the nail should lie just below the surface of the bone.
The length of the nail can also be estimated by measurements of digital preop x-rays. Care should be taken that the whole humerus is pictured.
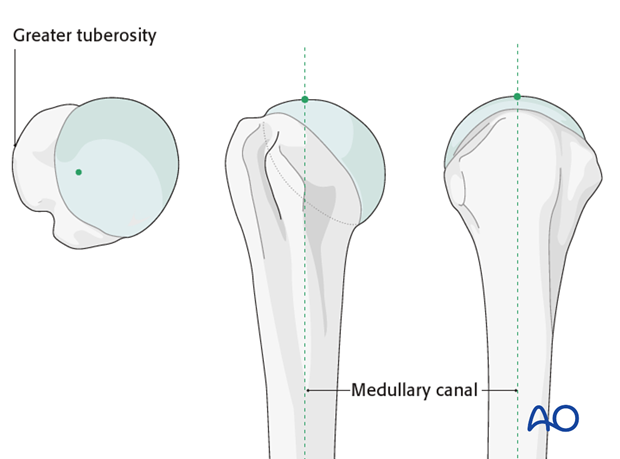
4. Entry point
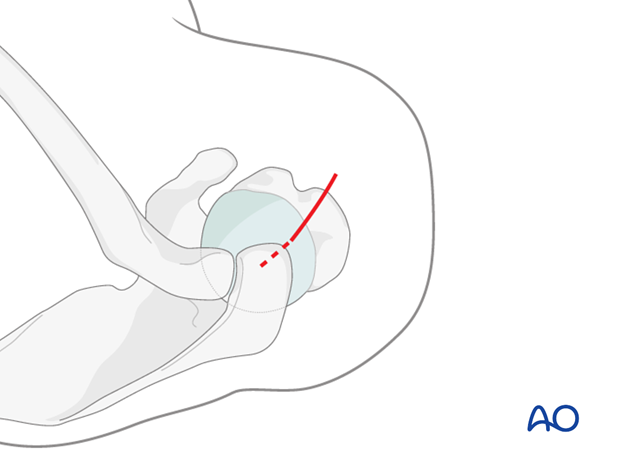
Location of entry point
Different nailing systems have nails of different shapes, and so may require different entry points. Refer to the manufacturers' operative technique guides for further details.
The insertion point for the straight nail is in line with the medullary cavity. Typically, it ends up at the highest point of the humeral head. In contrast to bent nails it is located intraarticularly completely, well away from the insertion of the supraspinatus tendon.
Insertion of guide wire
Insert a guide wire through the correct entry point and confirm proper placement by image intensification.
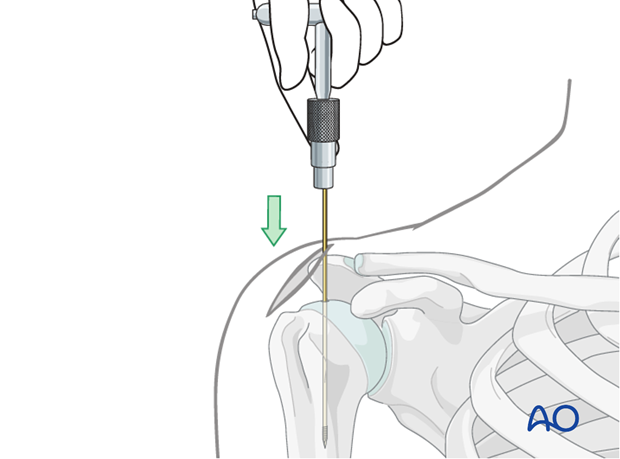
Opening the canal
A cannulated drill bit is recommended for opening the proximal humerus.
Insert this drill bit over the guide wire and advance into the proximal medullary canal.
Alternatively, use an awl to open the humerus.
5. Reaming
Indication
If the canal is very narrow rather than inserting a narrow nail, reaming will allow for the insertion of a larger diameter (ie stronger) nail. This may be particularly useful when nailing a nonunion.
Procedure
Pass an olive tipped guide wire across the fracture site. With experience it is usually possible to feel the tip of the wire is in the cancellous bone, but this should be confirmed with image intensifier.
Ream up sequentially to an appropriate size for the desired nail. In segmental or multifragmentary fractures take care to avoid soft-tissue damage, particularly to the nerves and vessels, as the reamer is passed through the fracture zone.
Exchange the olive tipped wire to a straight guide wire, and then insert the nail over the guide wire. Alternatively, some nails may be introduced without a guide wire.
6. Nail insertion
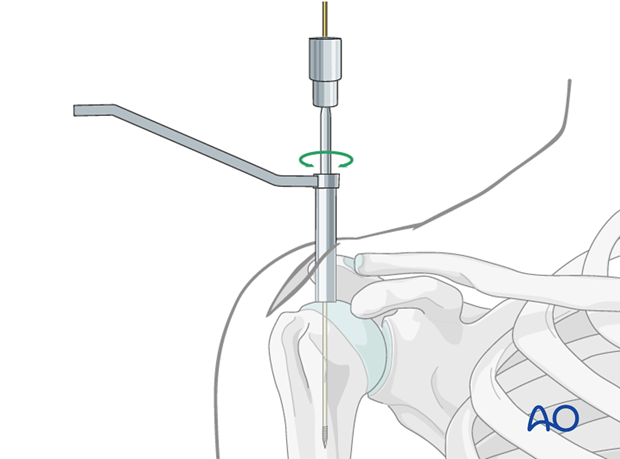
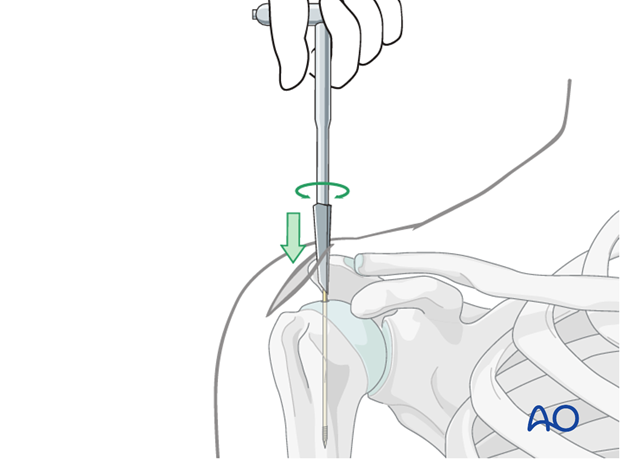
Insertion handle
Mount the humeral nail on the insertion handle. The nail must be rotated correctly relative to the insertion handle.

Insert the nail with slightly rotating movements down to the fracture line.
Do not use a hammer, as this may increase the risk of fissure or fracture at the insertion site.
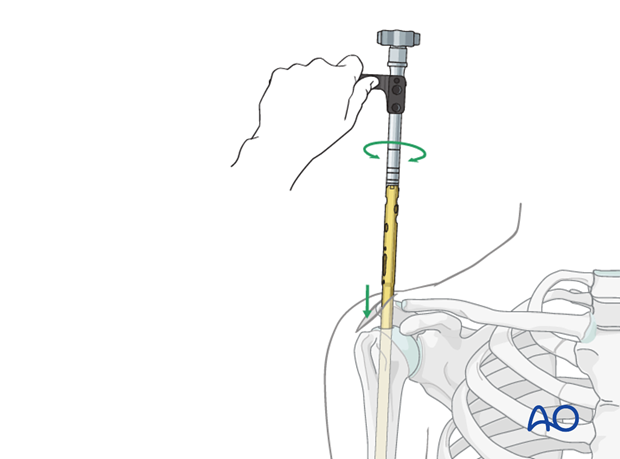
Advance the nail under image intensification just beyond the fracture site.
If inserting an unreamed nail a guide wire may be helpful but may not be necessary.
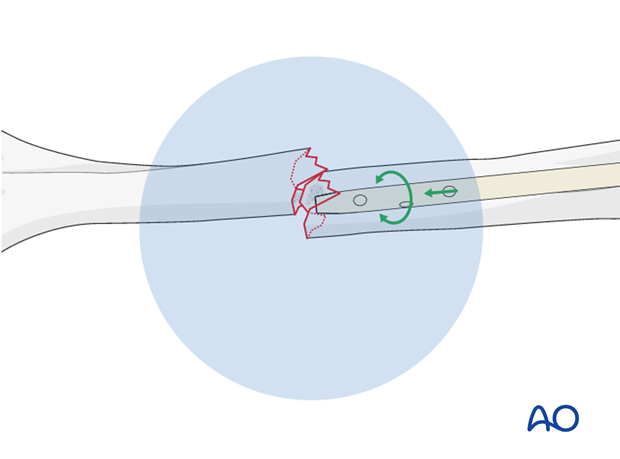
Reduction
Pass the fracture zone under image intensification and make sure that the nail enters the distal fragment properly.
Use the nail tip as a reduction aid. Alternatively, it may be easier to pass a guide wire with a bent tip across the fracture zone, and then pass the nail over the guide wire.
After passing the fracture zone, adjust humeral shaft alignment, rotation, and length.
Confirm under image intensification in two different planes.
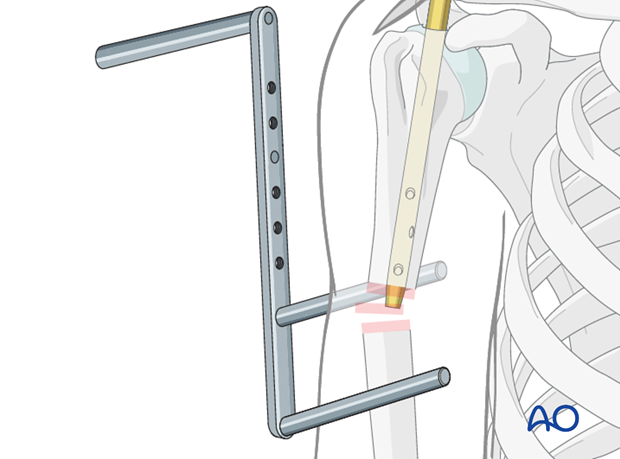
Pearl: F-tool for reduction
To lower the radiographic exposure to the surgeon’s hands use a radiolucent reduction tool (ie “F-tool”).
Open reduction
In some cases, there may be soft tissues interposed between the fragments. This prevents reduction and necessitates open reduction to remove any soft tissue.
If several attempts at introducing the nail into the distal fragment are unsuccessful the fracture site should be opened. Use a finger, bone hook or reduction clamp to reduce the fracture and pass the nail across the fracture site. This also reduces the radiographic exposure.
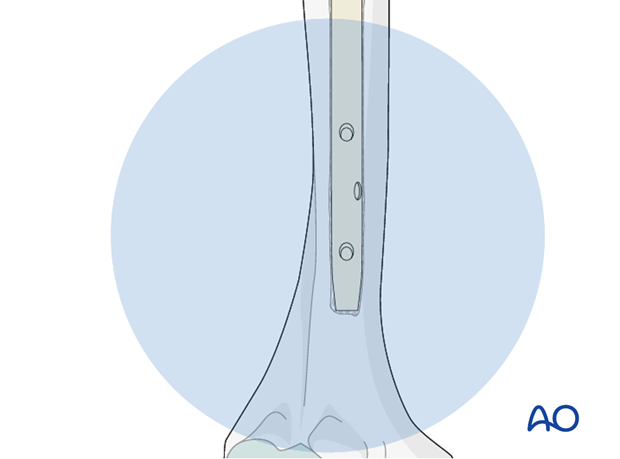
Definitive nail position
Gently advance the nail until it has reached the desired position just above the olecranon fossa. Avoid fracture distraction.
If a guide wire was used, remove it once the nail is in place.
Make sure the proximal end of the nail is placed beneath the bony surface of the humeral head.
No protrusion of the nail may be tolerated. Confirm with appropriately oriented C-arm images that the nail is below the bone.
If retrograde compression is planned insert the top of the nail into the humeral head far enough for it to remain below the articular surface after fracture reduction. See below for more details.
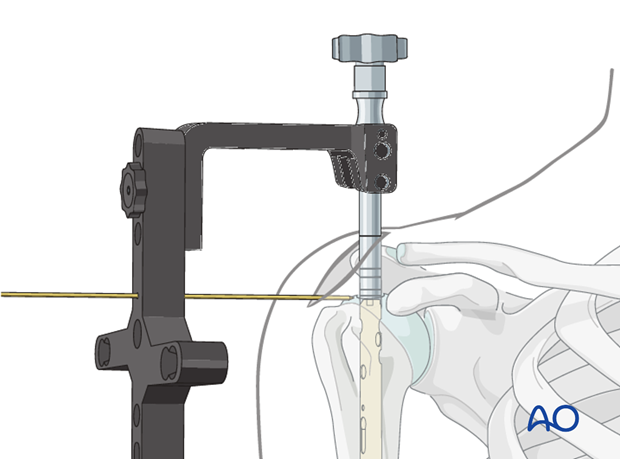
A K-wire placed through an aiming device may help to adjust the appropriate insertion depth.
Rotational reduction
Confirm the fracture reduction under image intensification. Ideally the fracture line should be closed anatomically.
In cases of comminution indirect signs can be helpful such as the width of the cortices proximal and distal to the fracture site. Both should have the same width. Any difference suggests rotational malalignment.
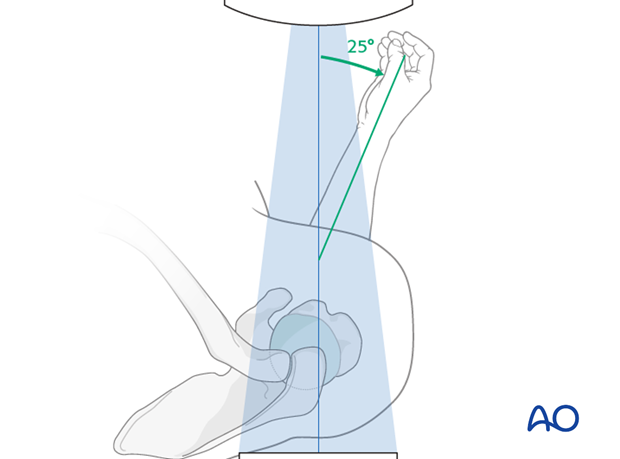
Alternatively, if the proximal fragment is in the correct anatomic position, confirmed with image intensification, the forearm should lie in 25° external rotation.
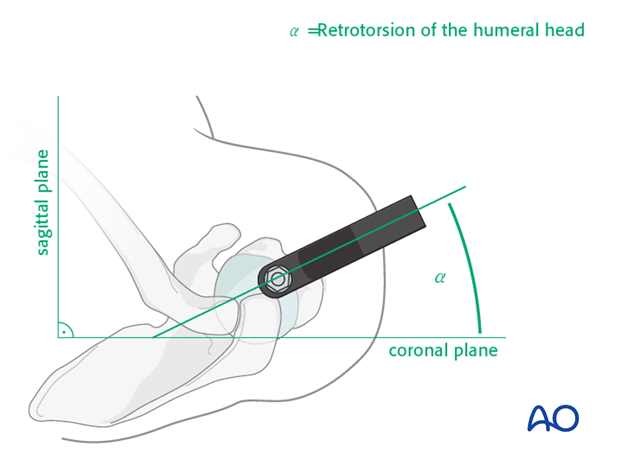
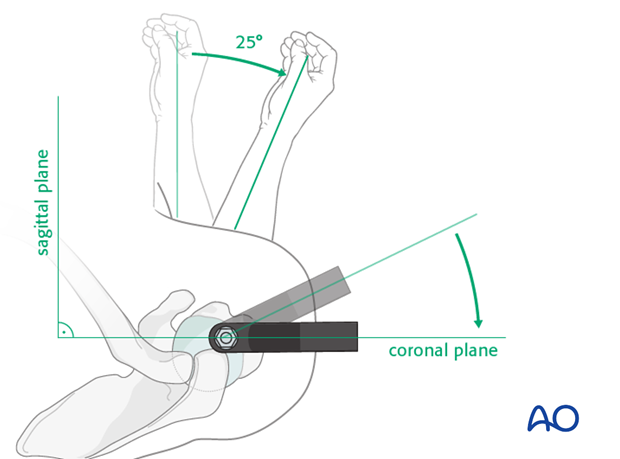
Rotational implant position
To lock the nail in the correct rotation, swivel the aiming arm approximately 25° anteriorly. Due to the physiological retrotorsion of the humeral head, the axis of the humeral head is directed approximately 25° posteriorly to the condylar plane of the distal humerus.
To obtain a true AP view of the proximal humerus, rotate the forearm approximately 25° externally relative to the sagittal plane.
Pitfalls
To achieve correct locking of the nail and avoid complications it is crucial to obtain the correct rotation of the nail in the humerus.
Typical problems arising after incorrect rotation of the nail are:
- Proximally: interference of the long head of the biceps
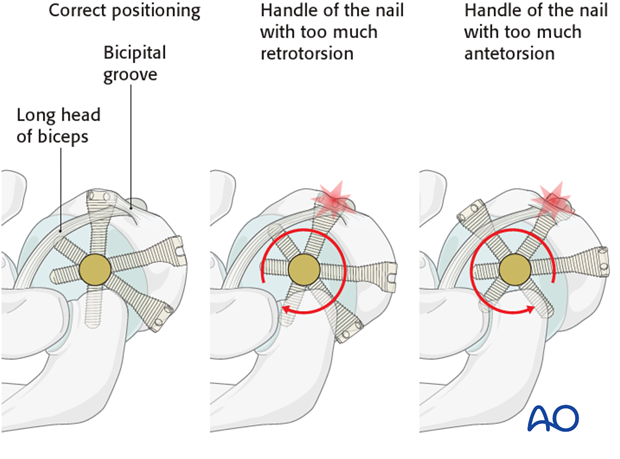
- Distally: interference of the screw insertion with neurovascular structures
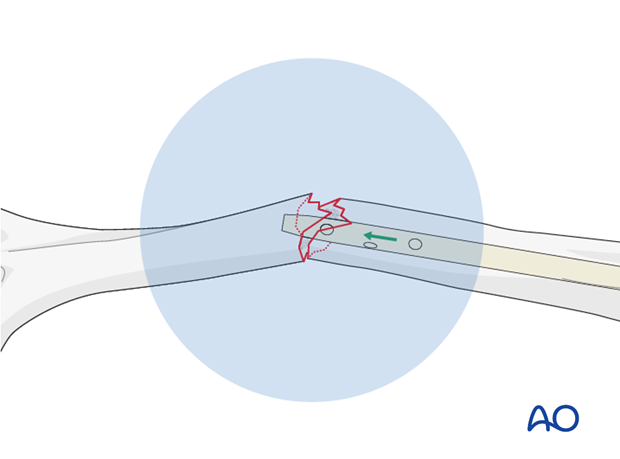
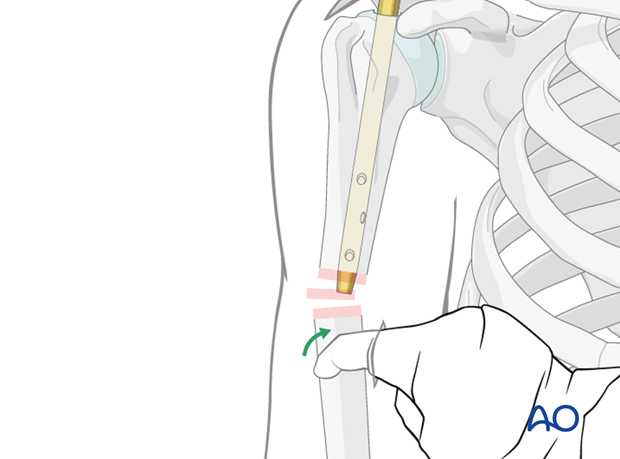
Longitudinal reduction
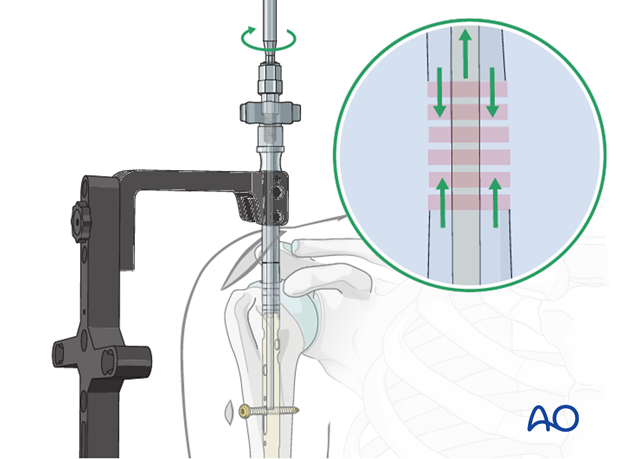
Confirm reduction of the fracture under image intensification. Take care that there is no fracture gap as this has a high risk of nonunion.
If there is a gap, it may be possible to close it with manual compression along the axis of the humerus, telescoping the distal fragment over the nail.
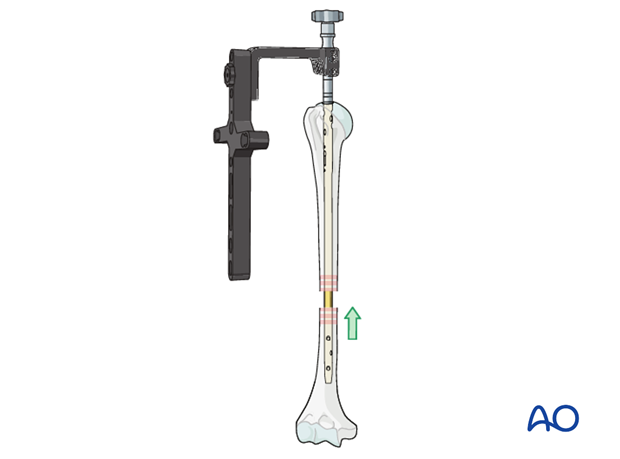
Alternatively, the gap can be closed with retrograde pulling of the nail after initial distal locking or by use of a compression mechanism implemented in the nailing system.
Both these techniques require the nail to be inserted deeper into the proximal fragment, so that as the fracture gap is closed the top of the nail comes to lie in the correct position. Otherwise an intraarticular, proximal protrusion of the nail will cause injury to the rotator cuff and impingement.
7. Proximal interlocking
Trocar insertion
Place the trocar for the planned screw fixation through the aiming device, if necessary through a separate skin incision. Perform blunt dissection down to the bone so that the trocar may be placed without interposition of soft tissue.
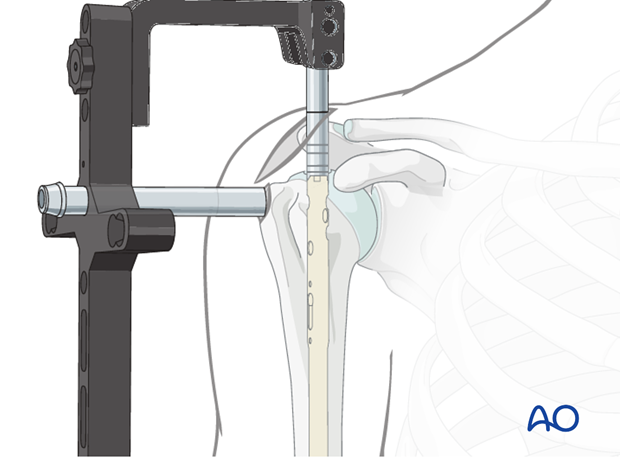
Predrilling
Check once more the correct retrotorsion.
Drill with the calibrated drill bit carefully just to the level of the subchondral bone. The final position of the drill bit can be checked with the image intensifier. The screw length can be determined from the measurements of the drill bit.
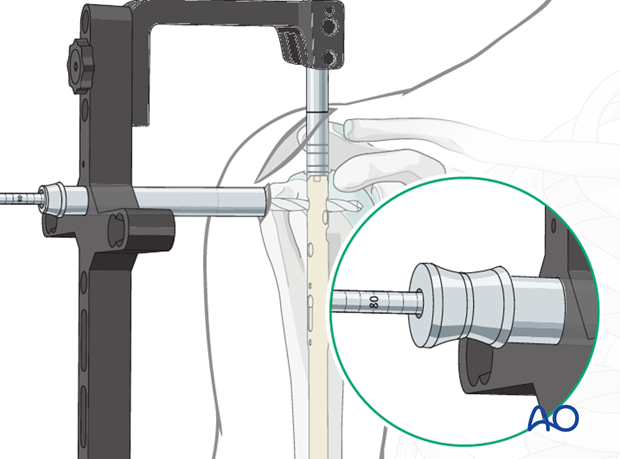
Screw hole widening in the lateral cortex
If the proximal locking bolts have enlarged heads the lateral hole must be overdrilled with the appropriate drill to avoid fracturing the lateral cortex.

Screw insertion
Attach the screw to the screw driver and insert the screw.
In some systems, as the one shown in this illustration, a screw-in-screw fixation is possible (see below) and may help in fractures involving the humeral head. If so and if also intended, the plane of the handle of the screw driver should be horizontal and the arrow should point posteriorly once the final position of the screw is reached.
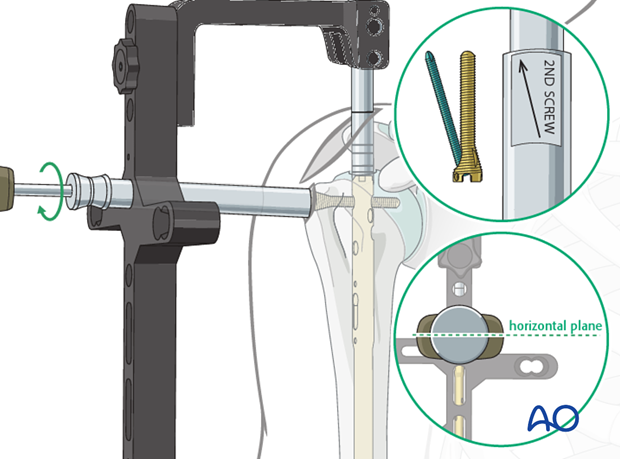
Insertion of further screws
Insert further screws using the aiming device according to the fracture pattern.
Remove the aiming device.
8. Distal interlocking
Position of the arm
Distal interlocking is typically performed using a freehand technique. Therefore, the arm has to be placed in a stable position for distal locking under image intensification.
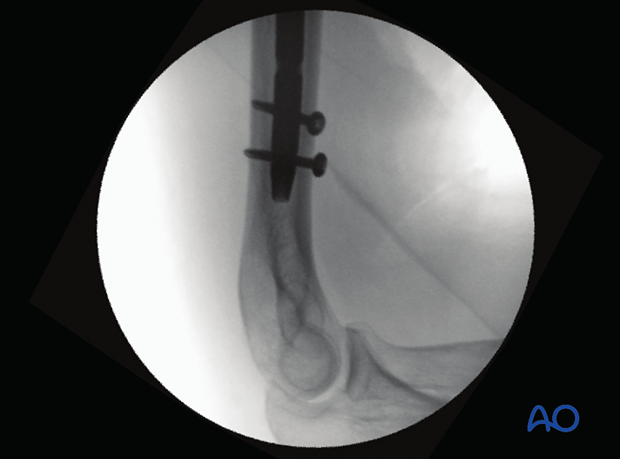
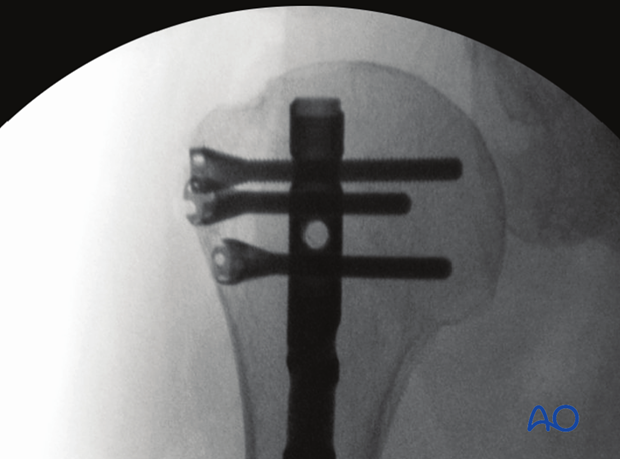
Defining the correct position of the arm/C-arm
It is crucial for a proper freehand interlocking to define the correct position of the arm/C-arm. This is defined under image intensification showing a perfectly round circle of the nail’s locking holes within the center of the image.
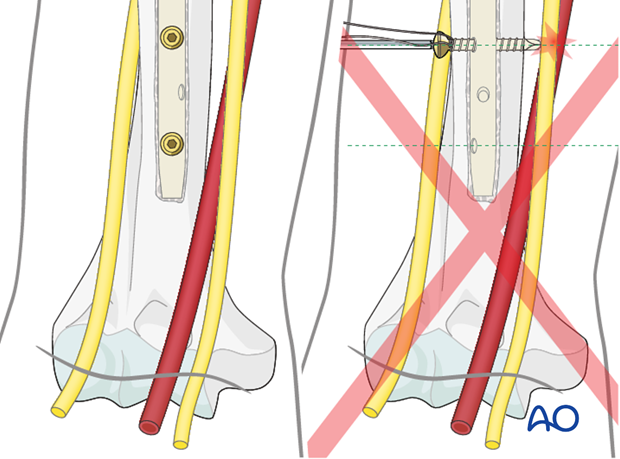
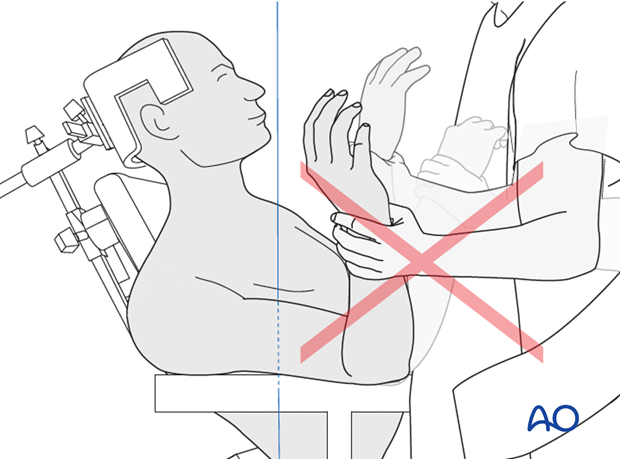
Pitfall: unrecognized malrotation
While positioning the arm and determining the proper position of the C-arm pay special attention not to produce an unrecognized malrotation by just rotating the forearm.
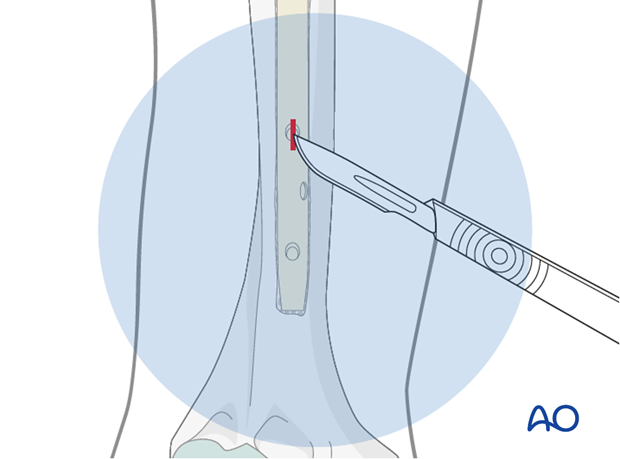
Skin incision
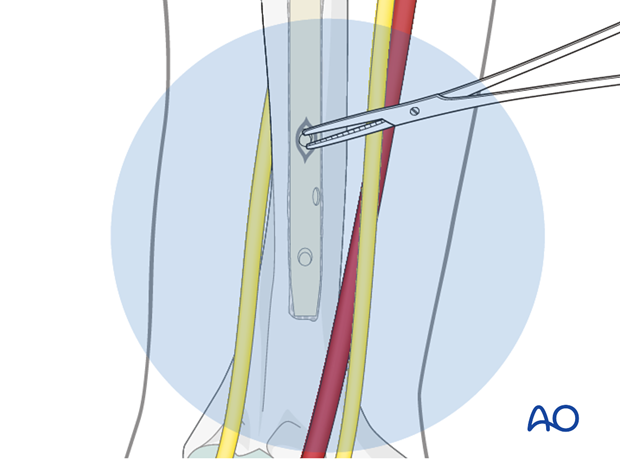
A rare but serious complication is injury to either the brachial artery and/or the median nerve while inserting the distal locking screw.
Therefore, take special care, using blunt dissection. If in any doubt widen the exposure and use retractors to protect the neurovascular structures.

Position the tip of the scalpel over the proximal hole, as shown under image intensification, and incise the skin.
Soft-tissue dissection
Use small scissors or artery forceps to prepare a track for insertion of the drill bit.
Drilling
Perform the positioning of the drill tip, its fine adjustment, and the drilling procedure under image intensification.
Many surgeons prefer a radiolucent drill attachment if it is available.
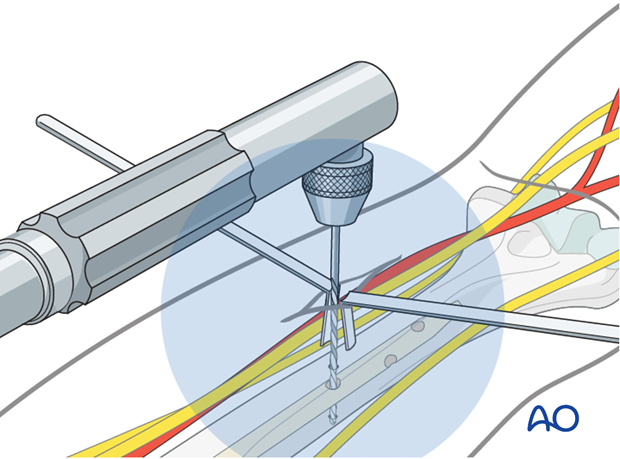
Center the radiopaque circles of the radiolucent drill on the locking hole.
Measure the length of the required screw with a depth gauge.

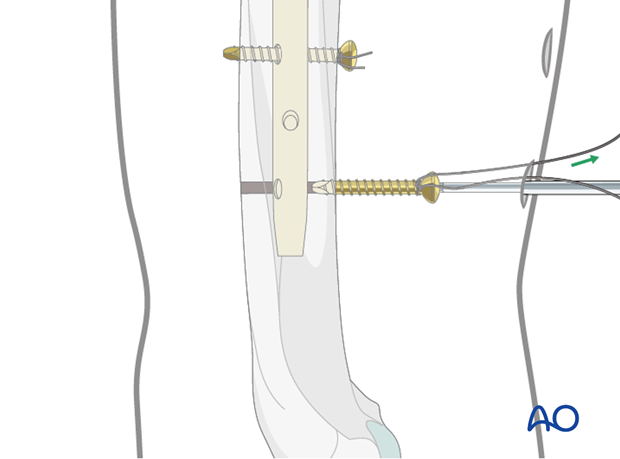
Insertion of interlocking screws
Insert the first interlocking screw and check for the correct position and length under image intensification in two planes.
Insert further interlocking screws as described above.
Pearl: absorbable suture around screw
To avoid losing the screw in the soft tissues during insertion and tightening, fasten an absorbable suture around the screw’s head beforehand.
Final remark
When interlocking is completed, check the definitive position of the implant under image intensification in two planes.
Take particular notice of the position of the proximal end of the nail, the location and length of all interlocking screws.
9. Option: fracture reduction/compression after distal locking
Distal locking
Insert the distal locking screws first as described above, ensuring that the top of the nail is sufficiently buried in the humeral head.
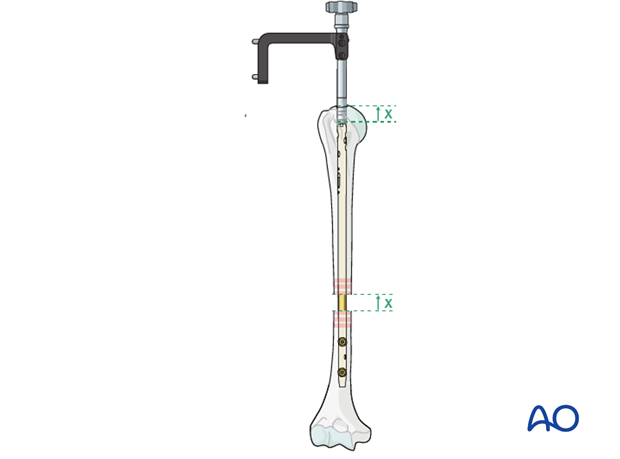
Manual reduction
Attach the removal device. Reduce the distal humeral fragment with gentle hammer blows, bringing the nail proximally within the proximal fragment. Confirm satisfactory reduction with image intensifier.
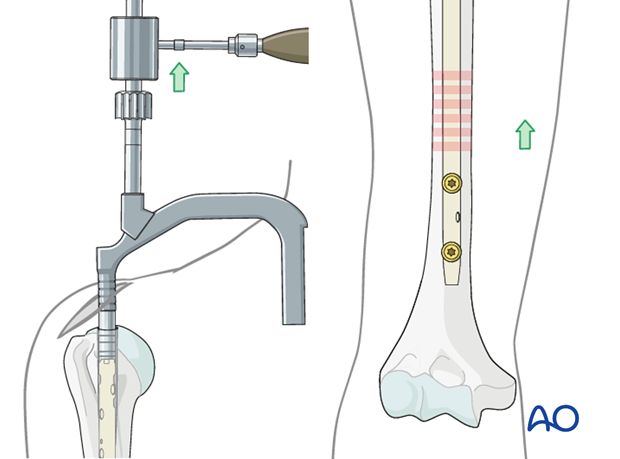
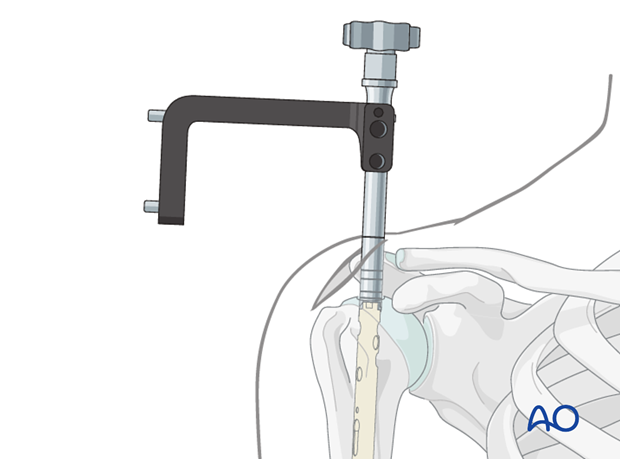
Reduction with compression device
Prior to compression insert a proximal gliding screw, which is applied through the dedicated guide hole in the aiming device.
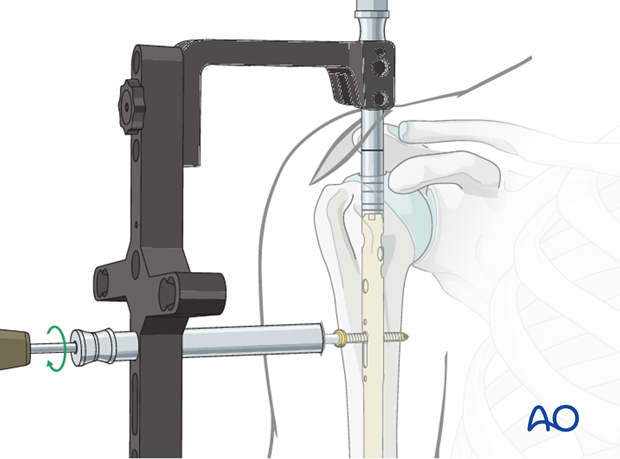
Compression of the fracture site or closure of a gap is applied by inserting a compression screw from the top of the nail. By tightening the screw, the whole nail with the distal fragment is pulled retrogradely.
Confirm the effect under image intensification.
After achieving satisfactory reduction remove the compression screw.
Proceed with the proximal locking as described above for static interlocking.
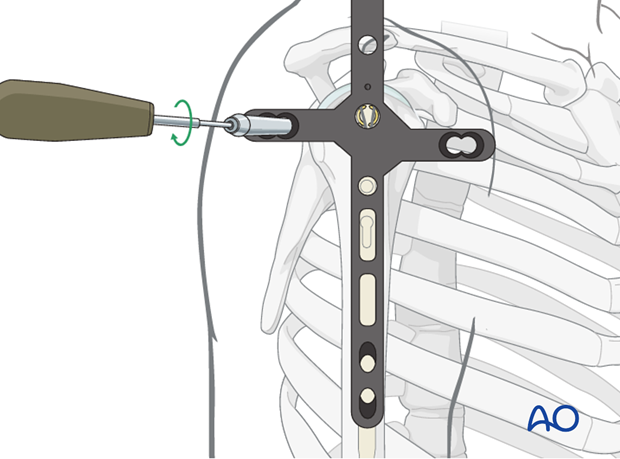
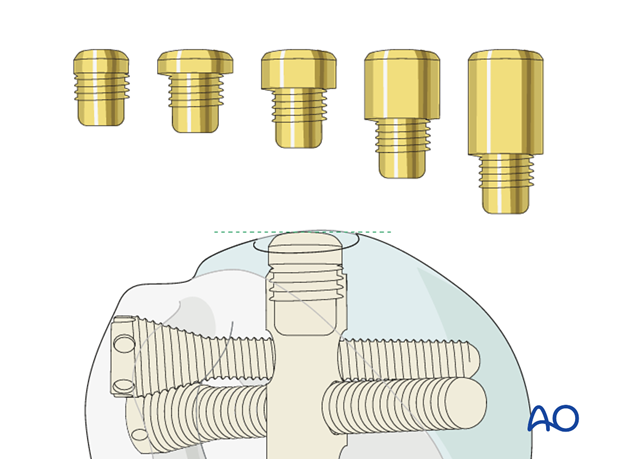
10. Nail capping
Remove the insertion handle/aiming guide and its connecting screw.
Insert an end cap to prevent ingrowth of bony tissue.
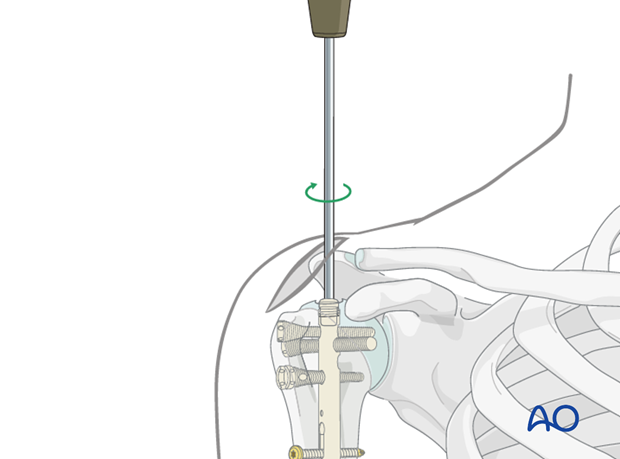
End caps of different lengths may be available. The top of the end cap should lie just below the articular cartilage, to facilitate later implant removal, but must not protrude above the humeral surface.
Check the proper dimension of the end cap under image intensification.
11. Aftercare
Principles
The aim of any surgical fixation of humeral shaft fractures is a stable osteosynthesis of the fracture allowing early passive and active motion. This is crucial to prevent shoulder stiffness.
The rehabilitation regimen should take account of the quality of the rotator cuff, its split and fixation.
Immediate postoperative care
Carefully examine the patient for neurological deficits and pulses.
Early treatment
In the beginning lymph drainage and elastocompressive bandages may be helpful.
Consider a sling for pain relief within the first days.
Treatment for rotator cuff split fixation at risk
If the rotator cuff quality is poor, or the split was not in line with the fibers and/or there was detachment of the rotator cuff footprint, active shoulder abduction should be delayed within the first six weeks. Consider a shoulder abduction pillow and a continuous passive motion chair.
Mobilization
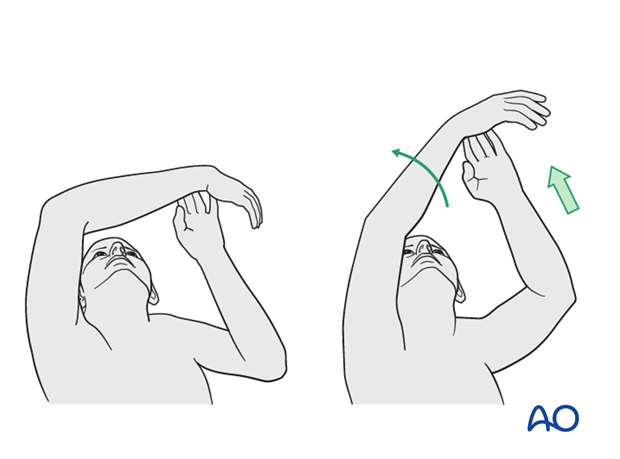
In the early phase the rehabilitation consists of classic maneuvers eg overhead motion exercises.
Rehabilitation should address the entire upper limb.
Exercise against resistance
Depending on the bone quality and compliance of the patient, exercise against resistance might be limited.
Follow-up
Clinical and radiological follow-up should be scheduled at least 6 weeks, 12 weeks and 6 months after surgery and continued until a bony healing is confirmed.
Hardware removal
Typically, humeral nails are left in situ indefinitely.
If the head of the nail is prominent and causing impingement or partial shoulder stiffness, it may require removing. If individual locking screws cause problems, they may be removed without having to remove the nail.
When removing a nail minimize any damage to the rotator cuff and take care to perform a secure repair, especially in poor rotator cuff quality.













