ORIF - Plate fixation (distal 1/3)
1. Principles
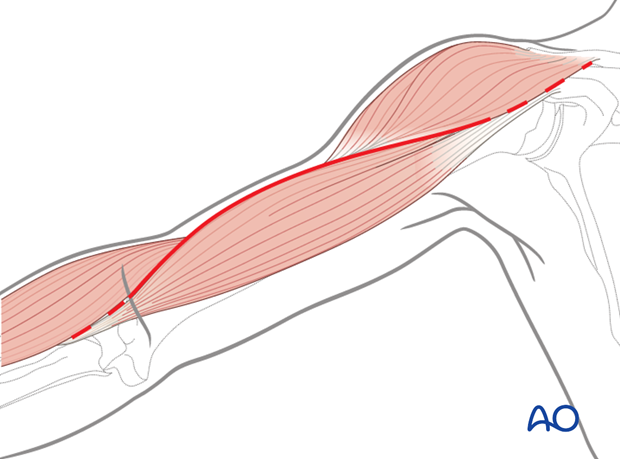
Plating in the distal humeral shaft
Depending on the fracture morphology it may be appropriate to obtain stable fixation with lag screws and then secure this with a neutralization plate. Alternatively, it may be better not to interfere with the fracture zone, and simply apply a bridge plate.
For stable plate fixation, typically three bicortical screws (6 cortical holds) would be used in each main segment. If locking head screws are used fewer screws may be sufficient.
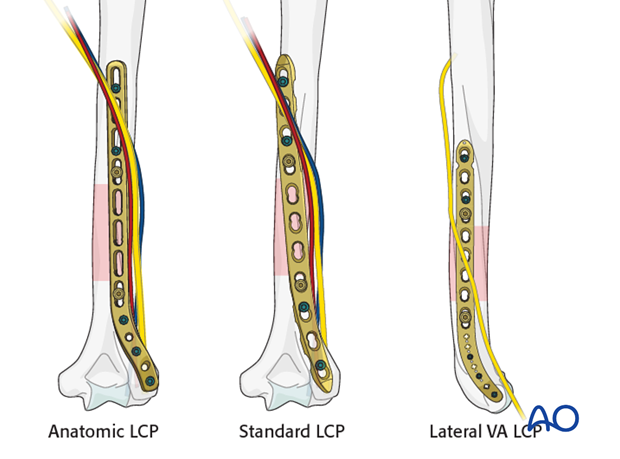
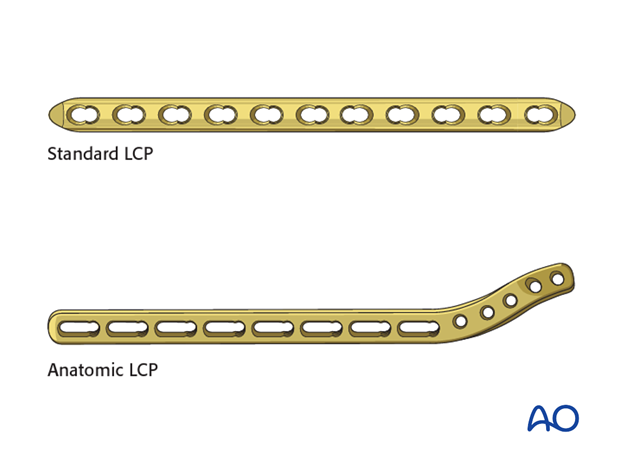
The use of standard LCP in the treatment of distal third shaft fractures is limited by the number of fixation points needed in the distal segment. More distal fixation may be obtained by placing the plate onto the lateral column. This is easier if precontoured (ie anatomic) extraarticular distal humerus LCP are used.
To illustrate the principles of plating a shaft fracture with distal extension, the posterior application of an anatomic plate (extraarticular distal humerus LCP) through a distal posterior approach (triceps-on) is described.
The application of a lateral or anterior plate follows the same principles.
Open fractures in the humeral shaft
Adequate surgical debridement is the crucial first step in the care of any open fracture.
Read more about the treatment of open fractures in the humeral shaft.
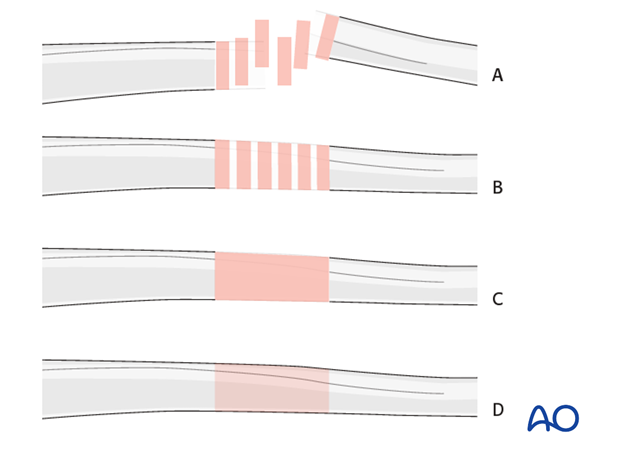
Note on illustrations
Throughout this treatment option illustrations of generic fracture patterns are shown, as four different types:
A) Unreduced fractureB) Reduced fracture
C) Fracture reduced and fixed provisionally
D) Fracture fixed definitively
2. Plate positioning
Introduction
The choice of plate position depends on the fracture morphology, the radial nerve pathology and the surgeon’s preference. The lateral, anterior, and posterior surfaces of the distal humeral shaft are all possible choices.
Posterior plating
Choose a plate long enough to achieve secure fixation in each main segment.
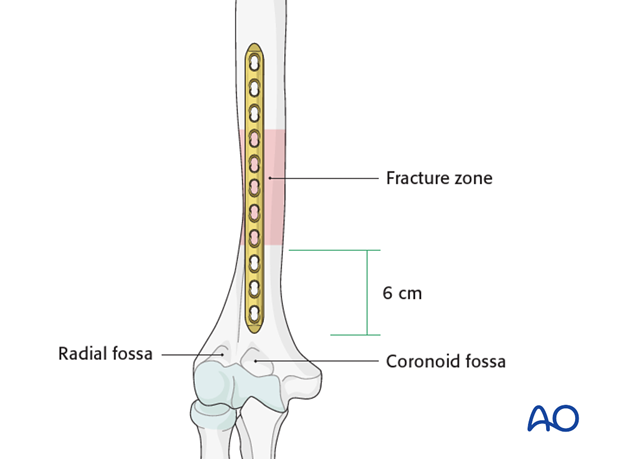
If the fracture extents distally to less than 6 cm proximal to the olecranon fossa, a standard plate (eg 4.5 mm LCP narrow) must be bent and/or twisted to obtain fixation on the lateral column of the distal humerus.
Alternatively, anatomic, extraarticular distal humeral plates may be used in fixation of these fractures.
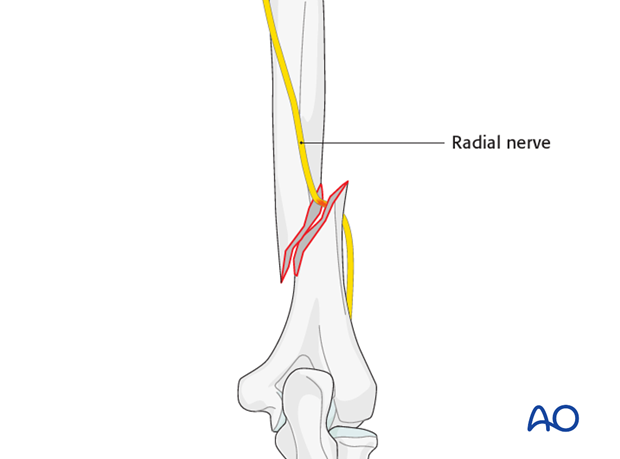
Lateral plating
Lateral plating is recommended if a radial nerve injury is apparent and requires further exploration/treatment (ie Holstein-Lewis fracture).
Typically, a straight LCP requires bending to fit the lateral aspect properly. Alternatively, anatomic, lateral distal humeral plates (VA-LCP) may be used.

Anterior plating
The anterior plate position is appropriate for those fractures which extend distally up to 6 cm above the coronoid fossa allowing for 6 cortical fixation points in the distal segment.
Typically, straight 4.5 mm LCP narrow can be used. Anatomic plates are not available for this region.
3. Patient preparation and approaches
For fractures extending distally the distal posterior or lateral approaches are recommended, as they provide access to more fixation points in the lateral column of the humerus.
The distal posterior approach may be performed with the patient either in a lateral or prone position.
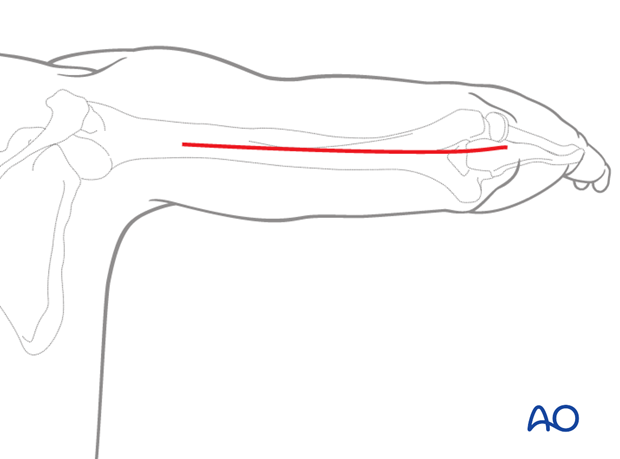
The lateral approach, with the patient in a supine position, provides good access to the radial nerve alongside the intermuscular septum which is necessary in cases of radial nerve injuries.
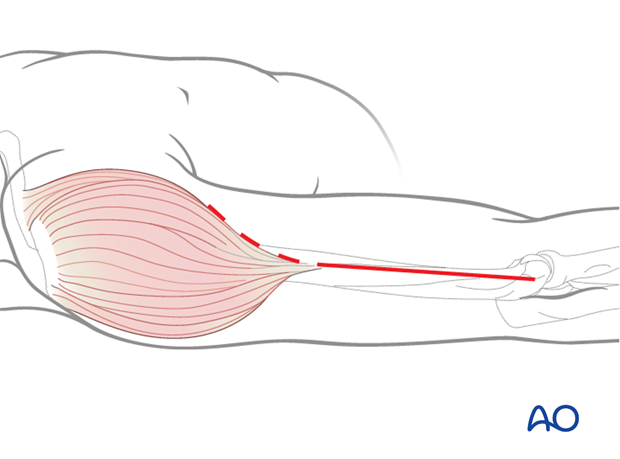
For plate application on the anterior aspect of the distal humerus the approach uses the distal part of the extended anterolateral approach with the patient in a supine position.
4. Reduction and lag screw fixation
Reduction
It is important to restore axial alignment and rotation.
In osteoporotic bone anatomic reduction should be achieved as callus formation is poor.
Anatomic reduction and internal fixation follows the principle of reducing the numbers of fragments from 4 to 3, 3 to 2 and 2 to 1 starting distally.
Alternatively, a bridging technique may be used.
Lag screw fixation
If the fragments are big enough and the fracture planes are suitable, the fragments may be reduced and held with lag screws or cerclage.
Reduce the most distal fragment to the distal humerus, hold it with a pointed reduction forceps and fix it with a lag screw.
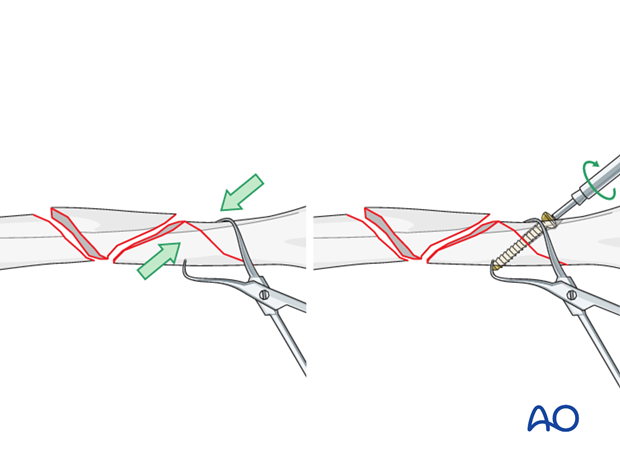
Then proceed with the next fragment and fix it to the proximal humerus.
If possible reduce the two main fragments using a pointed reduction forceps. Take care of proper rotation.
Option: A further lag screw may be used but typically it is not necessary.
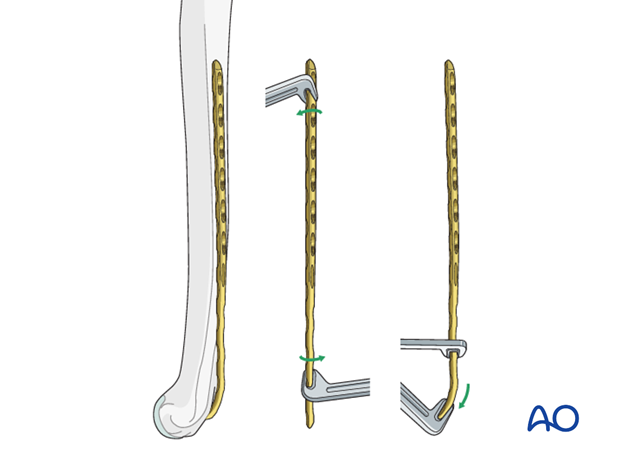
5. Plate contouring
Anatomic plates may not need contouring, but sometimes they need some fine adjustment.
If a standard LCP plate will be positioned over the lateral column of the distal humerus bending of the plate is necessary. In-plane bending is not possible except with reconstruction plates. The plate must be twisted, and also bent to allow for the physiological antecurvature of the lateral column.
The screw application follows the same order as for the precontoured plate described below.
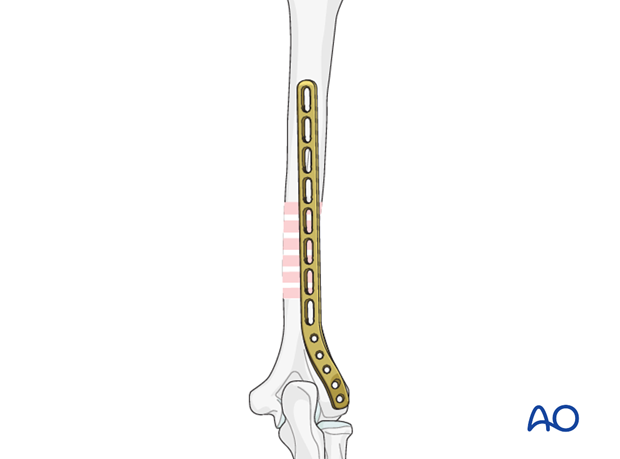
6. Plate application
Plate positioning
Position the plate on the posterior aspect of the humerus.
Adjust the distal end of the plate to the lateral column of the distal humerus. Take care that the plate does not cause an impingement with the olecranon.
Check the correct plate position proximally in line with the humerus.
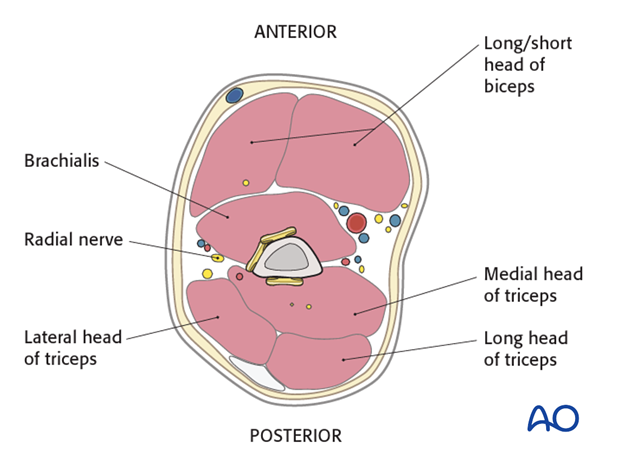
Placement under radial nerve
Frequently the posterior plate is longer than expected and requires a proximal placement under the radial nerve which must be identified and mobilized. In these cases, proper documentation of the relation between the radial nerve and the plate should be recorded in the operation note.

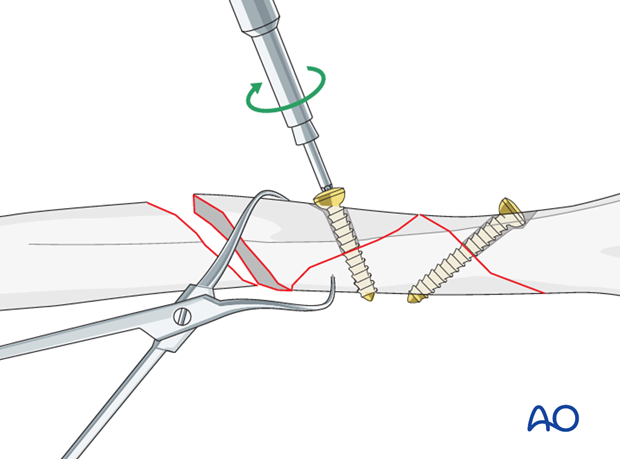
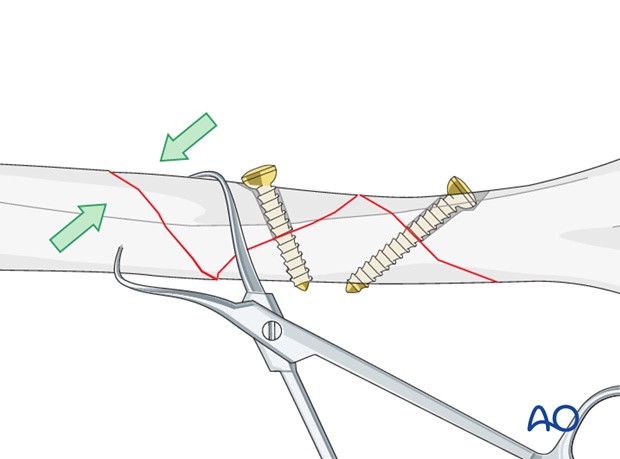
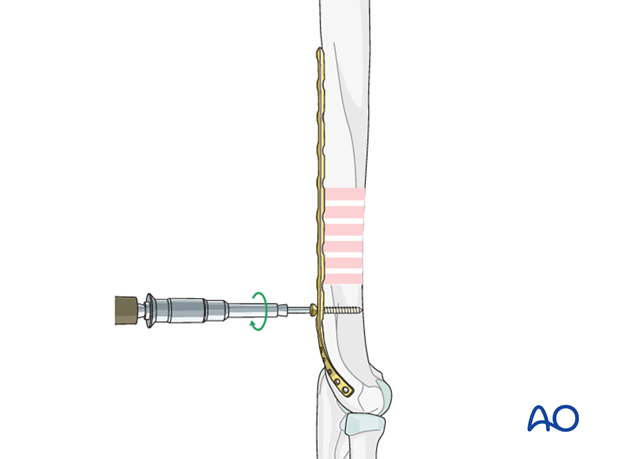
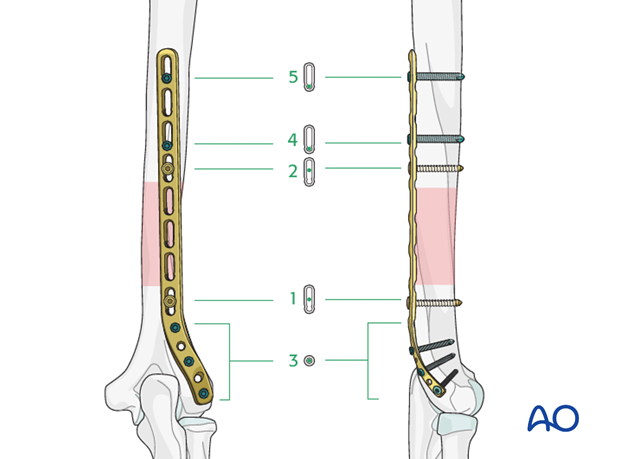
Insert first distal screw
Fix the plate to the distal humeral segment by using a bicortical cortical screw.
Check the fracture reduction and plate position again.
Insert first proximal screw
Fix the plate to the humerus proximal to the fracture by using a second bicortical cortical screw.
Check the fracture reduction and plate position again.
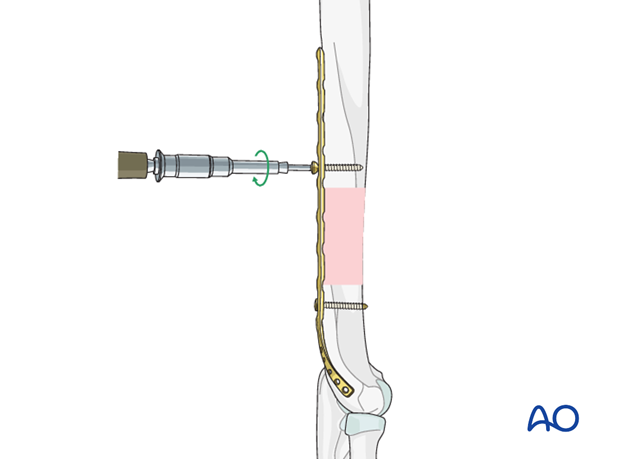
Final screw insertion
Insert the remaining locking screws through the plate distal and proximal to the fracture. Typically, one should look for 6 cortical holds each proximal and distal to the fracture.
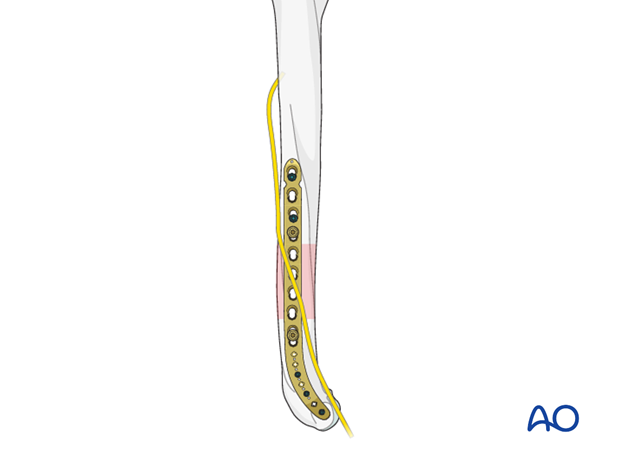
7. Application of a lateral plate
The application of the lateral plate follows the same sequence as with the posterior plate.
Slide the plate underneath the radial nerve which runs through the intermuscular septum towards the anterior compartment of the distal humerus.
Proper documentation of the relation between the radial nerve and the plate should be noted in the operation note.
8. Final radiological assessment
Check for proper reduction and implant position with image intensification in AP and lateral views.
Also confirm correct torsional alignment of the humerus.
9. Aftercare
Principles
The aim of any surgical fixation of humeral shaft fractures is a stable osteosynthesis of the fracture allowing early passive and active motion. This is crucial to prevent elbow stiffness.
The rehabilitation regimen should take account of any damage to soft tissues, either as a result of the injury or due to the surgery. It also needs to take account of the security of the fixation.
Immediate postoperative care
Carefully examine the patient for neurological deficits and pulses.
Early treatment
In the beginning lymph drainage and elastocompressive bandages may be helpful.
Consider a sling for pain relief within the first days.
Treatment for refixation of deltoid detachment
If the deltoid was detached and reattached, active deltoid contraction should be delayed for the first six weeks.
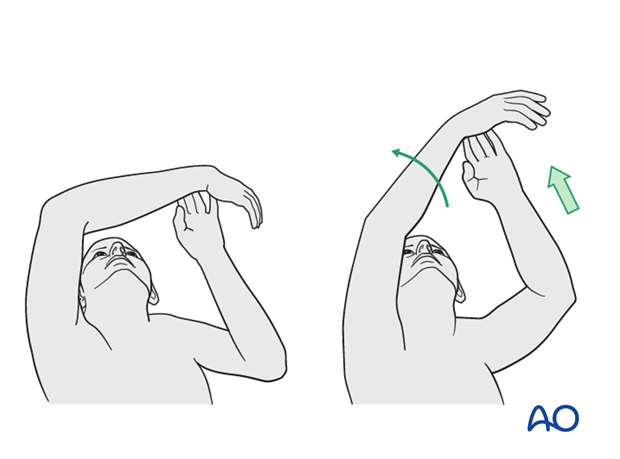
Mobilization
In the early phase the rehabilitation consists of classic maneuvers eg overhead motion exercises.
Rehabilitation should address the entire upper limb.
Exercise against resistance
Depending on the bone quality and compliance of the patient, exercise against resistance might be limited.
Follow-up
Clinical and radiological follow-up should be scheduled at least 6 weeks, 12 weeks and 6 months after surgery and continued until a bony healing is confirmed.
Hardware removal
Typically, humeral plates are left in situ indefinitely.
If removal is considered, bony healing should be confirmed. Plates are not normally removed for at least one year after surgery.
Be aware of the risk to the various nerves when dissecting the soft tissues to gain access to the distal humerus for removing anterior or anterolateral plates.
As the radial nerve runs over a posterior plate, removing this plate should only be considered with great caution, and the patient must be well informed about the risks. The original operation note should describe the relation of the nerve to the plate and should be reviewed before plate removal.













