Compression with a dorsal T-plate with or without lag screw
1. General considerations
Introduction
In this procedure, compression of an extraarticular oblique fracture with a dorsal T-plate screw is shown.
This follows the principles of compression plating of oblique fractures, ie, the plate should create an axilla (acute angle) with the oblique fracture line. If such an axilla cannot be created, lateral plating or lag-screw fixation with a neutralization plate should be considered.
Depending on the fracture morphology and surgeon’s preference, compression can be applied in one of the following modes:
- Compression with a plate
- Compression with a lag screw through a plate
Fracture plane
Obliquity of the fracture is possible either in the plane visible in the AP view or the lateral view. Always confirm the fracture configuration with views in both planes.
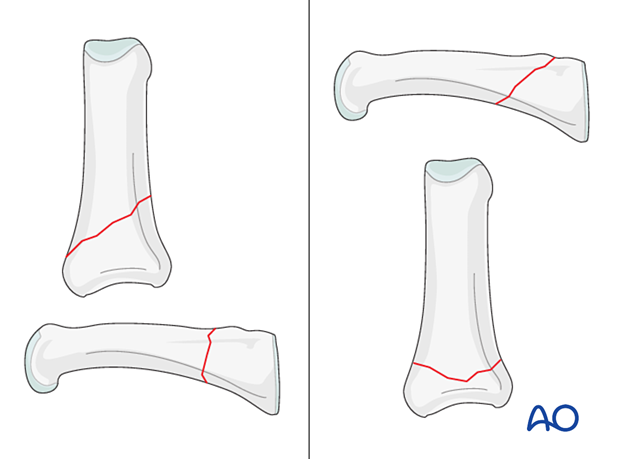
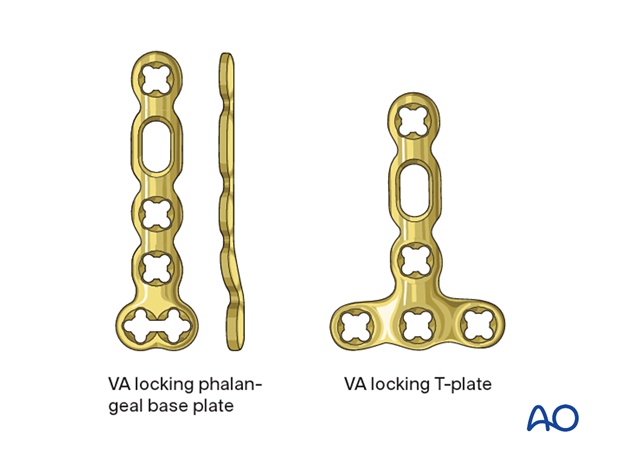
Plate selection
Two plate types are available for treatment of this fracture:
- 1.5 mm phalangeal base plate; lateral or dorsal
- 1.5 mm T-plate (adaption plate); dorsal
Select a plate according to fragment size, fracture geometry, and surgeon’s preference.
The T-plate is available as a plate with variable-angle (VA) locking-head screws. This plate type has the advantage of allowing insertion of two or three screws at variable angles into the articular block. The rounded plate edges avoid soft-tissue irritation and adhesion.
The plate needs to be contoured to fit the anatomy of the phalangeal base.
2. Patient preparation
Place the patient supine with the arm on a radiolucent hand table.

3. Approach
For this procedure, the following approach may be used:
4. Reduction
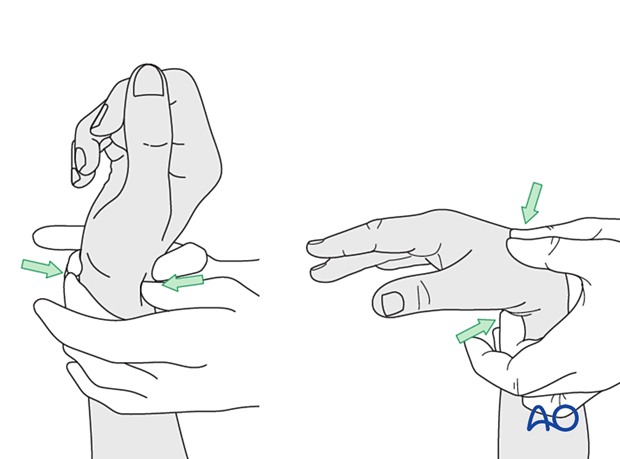
Indirect reduction
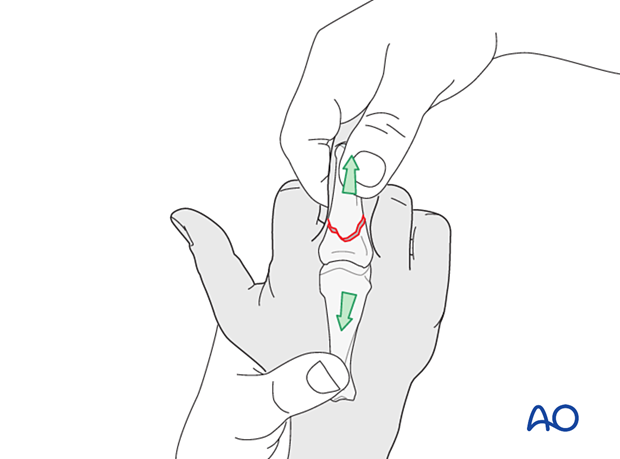
Reduction can be achieved by traction and lateral pressure exerted at the site of maximal displacement.
Confirm reduction clinically and with an image intensifier. If there is shortening of the finger, then there is often malrotation of the fracture.
If the fracture appears stable after reduction, nonoperative treatment can be considered. Confirming reduction with an image intensifier is then essential.
Direct reduction
Direct reduction is necessary when the fracture cannot be reduced by traction and flexion or is unstable.
When indirect reduction is not possible, this is usually due to interposing parts of the extensor apparatus.
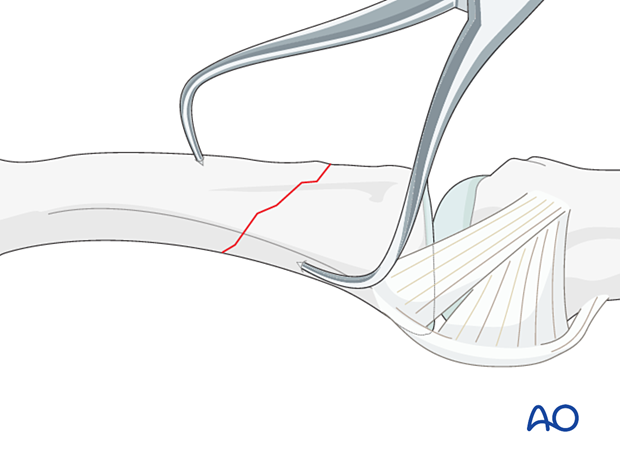
Use pointed reduction forceps for direct reduction.
Preliminary fixation
Retain the pointed reduction forceps for preliminary fixation or insert a 1.0 mm K-wire.
5. Checking alignment
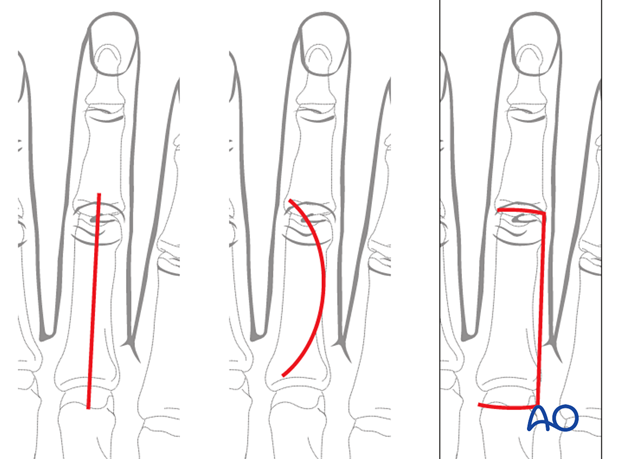
Identifying malrotation
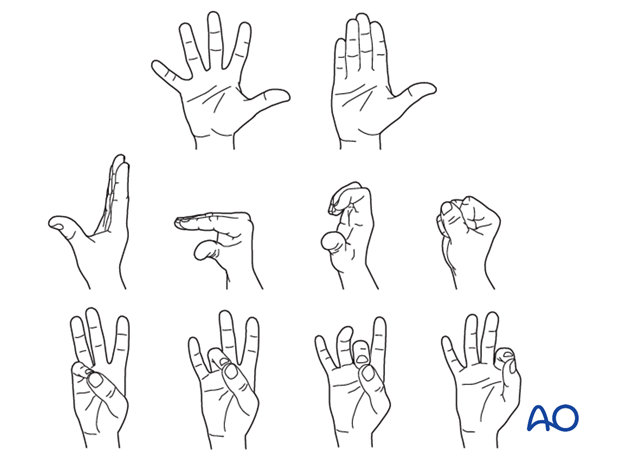
At this stage, it is advisable to check the alignment and rotational correction by moving the finger through a range of motion.
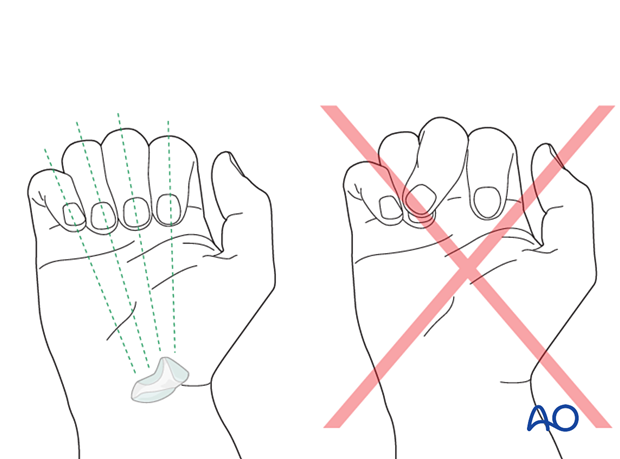
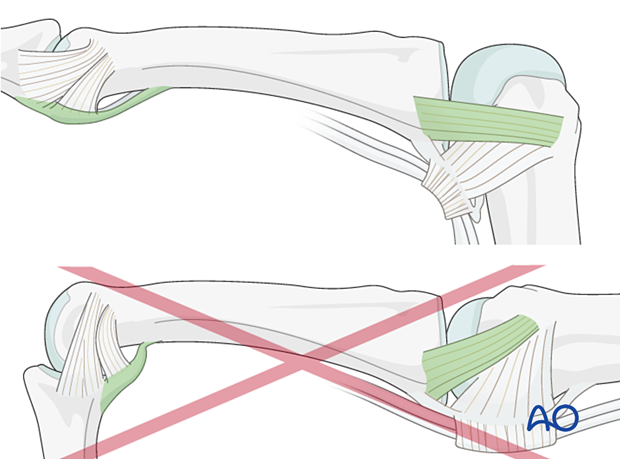
Rotational alignment can only be judged with flexed metacarpophalangeal (MCP) joints. The fingertips should all point to the scaphoid.
Malrotation may manifest by an overlap of the flexed finger over its neighbor. Subtle rotational malalignments can often be judged by a tilt of the leading edge of the fingernail when the fingers are viewed end-on.
If the patient is conscious and the regional anesthesia still allows active movement, the patient can be asked to extend and flex the finger.
Any malrotation is corrected by direct manipulation and later fixed.
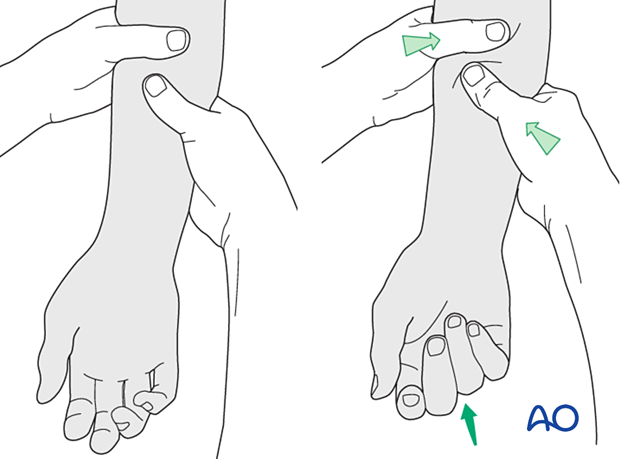
Using the tenodesis effect when under anesthesia
Under general anesthesia, the tenodesis effect is used, with the surgeon fully flexing the wrist to produce extension of the fingers and fully extending the wrist to cause flexion of the fingers.
Alternatively, the surgeon can exert pressure against the muscle bellies of the proximal forearm to cause passive flexion of the fingers.
6. Plate preparation
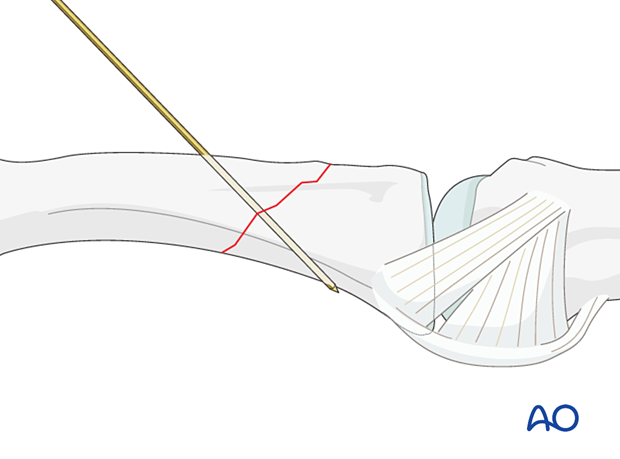
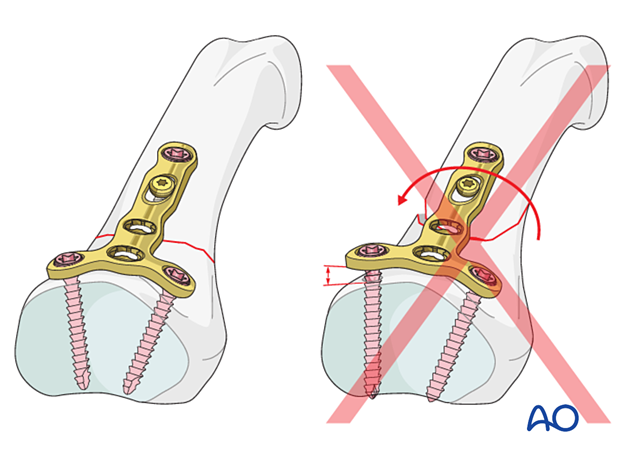
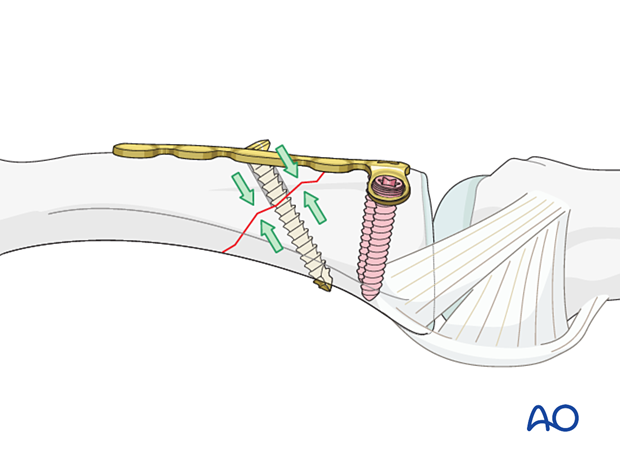
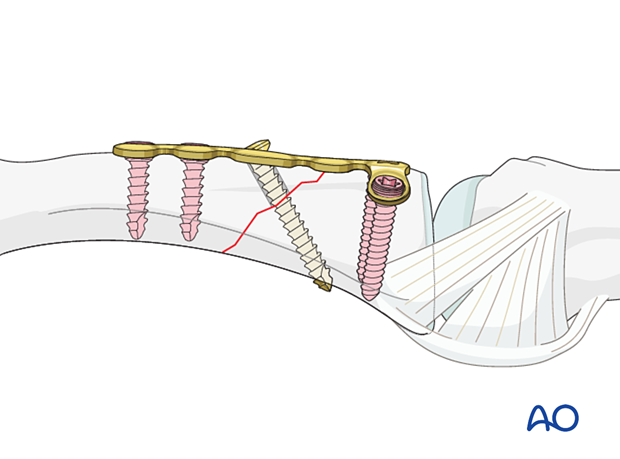
The fixation of an oblique fracture with a dorsal plate follows the principles of compression plating of oblique fractures, ie, the plate should create an axilla with the oblique fracture line.
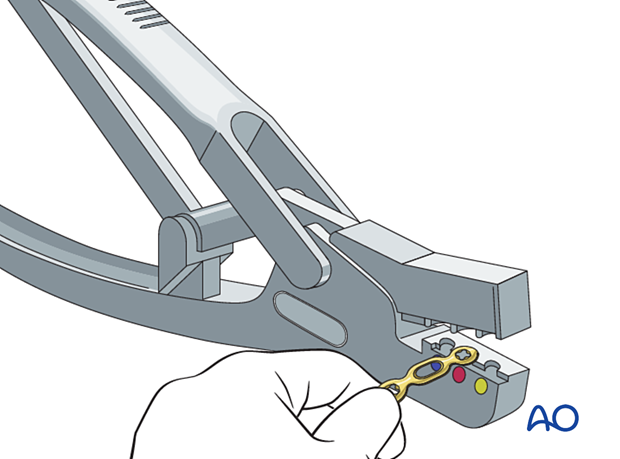
Plate trimming
Adapt the plate length to fit the length of the proximal phalanx. Avoid sharp edges, which may be injurious to the tendons. There should be at least 3 plate holes distal to the fracture available for fixation in the diaphysis. At least two screws need to be inserted into the diaphysis.
Contouring
The dorsal surface of the proximal phalanx is gently convex. If the straight T-plate is not adequately contoured to follow this convexity, tightening the distal screw will open the fracture on its palmar aspect.
If the plate is perfectly adapted to the dorsal surface of the phalanx, tightening the screws may result in a gap in the opposite cortex.
The solution is the same as all diaphyseal long bone transverse and oblique fractures. The plate is overbent so that when the screws are tightened, compression is applied across the whole fracture plane including the opposite cortex.
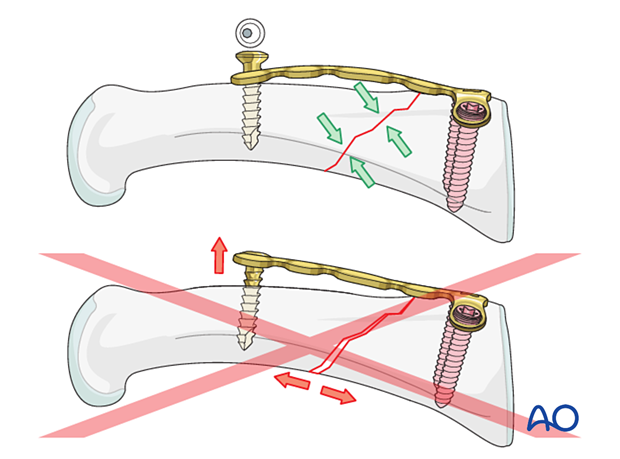
Check for perfect adaptation of the plate to the diaphysis and metaphysis.
If it is not perfectly adapted, fracture displacement or malrotation may occur.
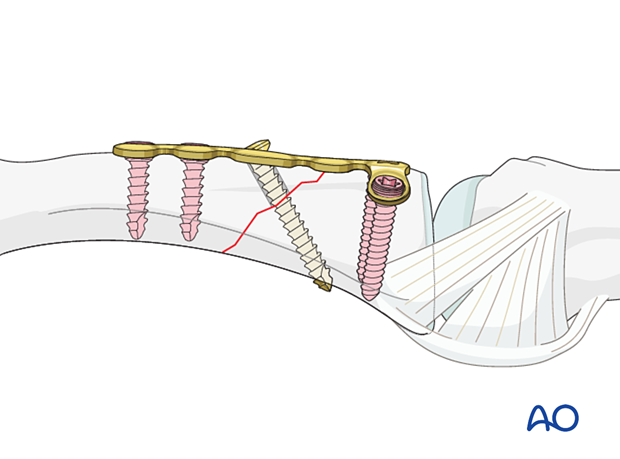
7. Plate fixation
Plate application
Place the plate dorsally on the phalanx, as proximally as possible, without interfering with the joint.
Ensure that the plate is centered on the diaphysis in the coronal plane.
Keep the plate in place with the atraumatic forceps.
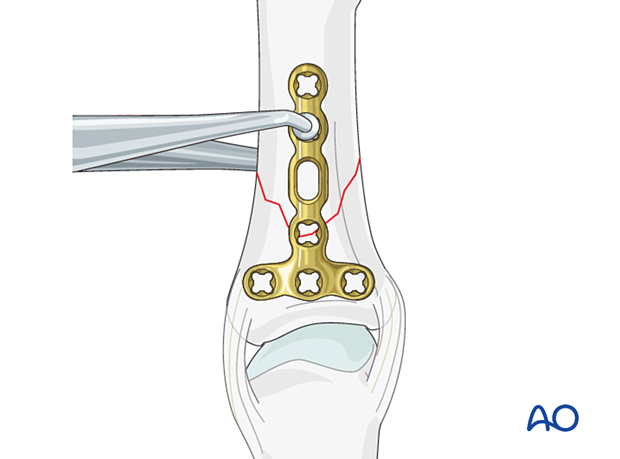
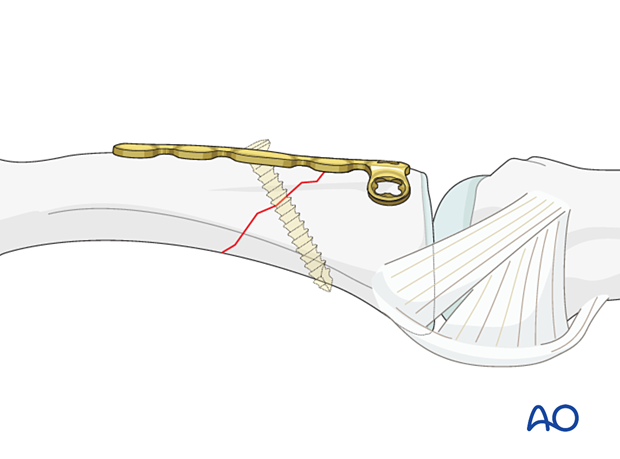
Introduction of a lag screw through the plate should be considered at this stage. The screw should run through the oblong hole and the middle of the fracture plane and as perpendicular as possible to it.
Order of screw insertion
The screws are inserted in an order determined by the direction of the oblique fracture plane.
In our example, we will show an oblique fracture running from dorsal/proximal to palmar/distal.
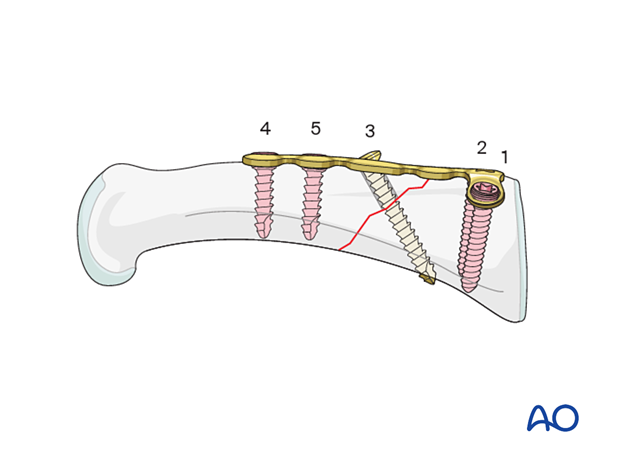
Screw insertion (proximal)
Insert two proximal screws:
Carefully drill a first hole for a screw through the transverse plate part with a 1.0 mm drill bit. The drill bit should engage but not penetrate the far cortex.
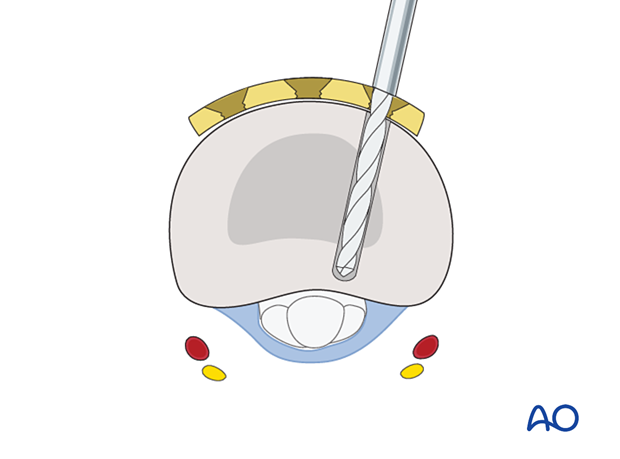
Insert the first screw. Ensure it engages the far cortex but does not protrude into the fibroosseous flexor digital channel, where the flexor tendons run. The digital nerve and artery are also at risk of injury.
Insert a second screw into the opposite end of the transverse plate section in the same fashion, alternately tightening both screws.
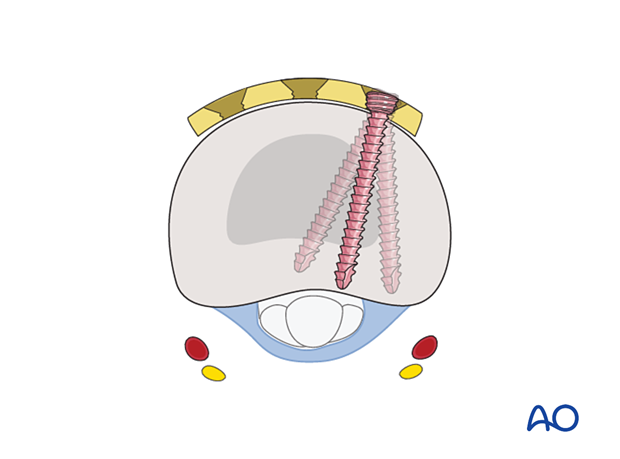
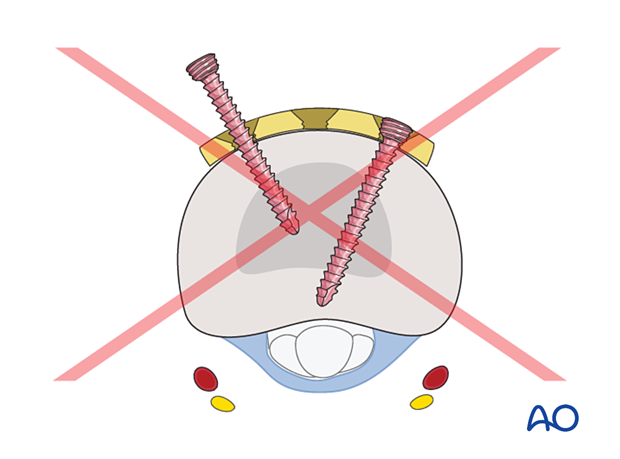
Pitfall: interfering screws
Compression with the plate
Insert a cortical screw in compression mode in the distal hole.
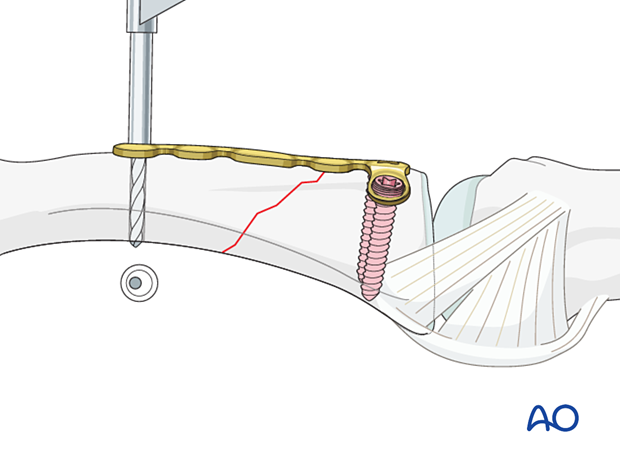
Compression with a lag screw
Insert a planned lag screw through the oblong hole as perpendicularly to the fracture line as possible.
Finalizing fixation
Insert further diaphyseal locking screw(s) to complete the fixation.
Cover the plate with periosteum to avoid adhesion between the tendon and the implant leading to limited finger movement.
8. Final assessment
Confirm fracture reduction and stabilization and implant position with an image intensifier.
9. Aftercare
Postoperative phases
The aftercare can be divided into four phases of healing:
- Inflammatory phase (week 1–3)
- Early repair phase (week 4–6)
- Late repair and early tissue remodeling phase (week 7–12)
- Remodeling and reintegration phase (week 13 onwards)
Full details on each phase can be found here.
Postoperative treatment
If there is swelling, the hand is supported with a dorsal splint for a week. This would allow for finger movement and help with pain and edema control. The arm should be actively elevated to help reduce the swelling.
The hand should be splinted in an intrinsic plus (Edinburgh) position:
- Neutral wrist position or up to 15° extension
- MCP joint in 90° flexion
- PIP joint in extension
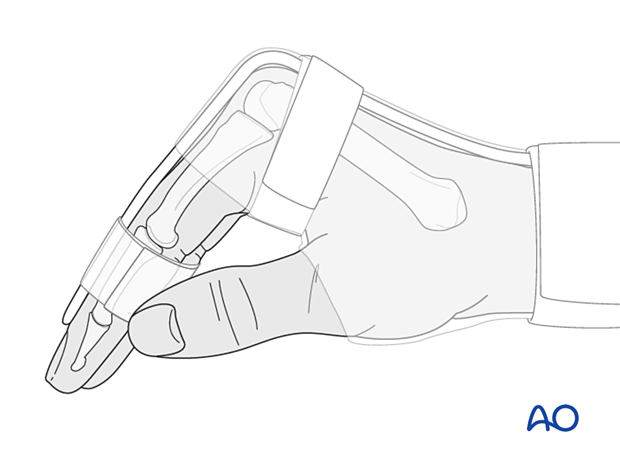
The reason for splinting the MCP joint in flexion is to maintain its collateral ligament at maximal length, avoiding scar contraction.
PIP joint extension in this position also maintains the length of the volar plate.
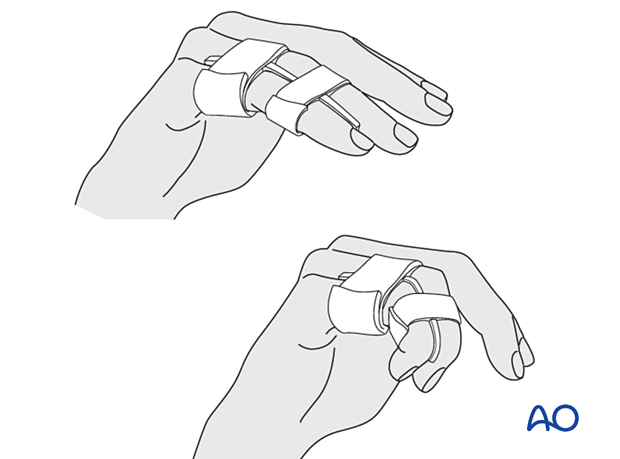
After subsided swelling, protect the digit with buddy strapping to a neighboring finger to neutralize lateral forces on the finger.
Functional exercises
To prevent joint stiffness, the patient should be instructed to begin active motion (flexion and extension) immediately after surgery.
Follow-up
See the patient after 5 and 10 days of surgery.
Implant removal
The implants may need to be removed in cases of soft-tissue irritation.
In case of joint stiffness or tendon adhesion restricting finger movement, arthrolysis or tenolysis may become necessary. In these circumstances, the implants can be removed at the same time.













