Reduction with or without joint transfixation
1. General considerations
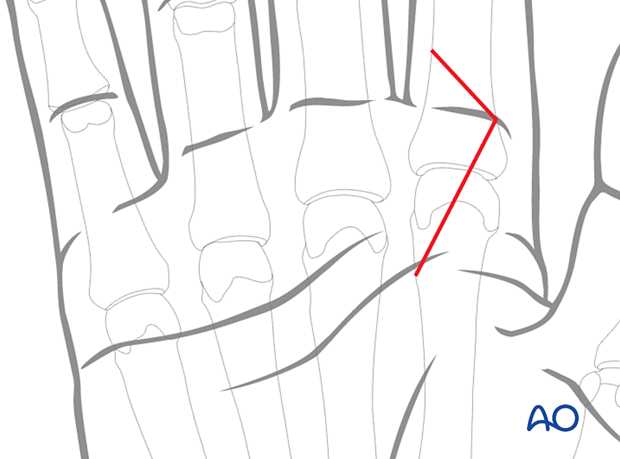
Dislocation of the metacarpophalangeal (MCP) joint, with or without small bony or ligamentous avulsions, may be reduced closed and the stability should then be evaluated.
If there is persistent instability, the joint may be transfixed with a temporary K-wire. In noncompliant patients, transfixation is recommended.
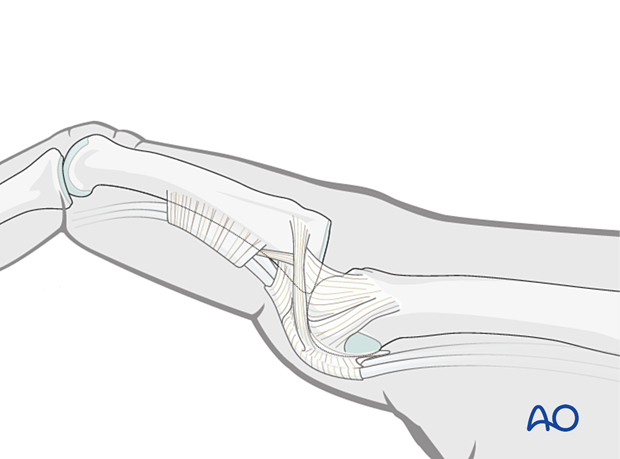
Often a volar approach to remove interposed soft tissues and repair of the sagittal bands are necessary.
Depending on the stability, the MCP joint may be stabilized with buddy strapping or a dorsal splint.
2. Patient positioning
Place the patient supine with the arm on a radiolucent hand table.
Local or regional anesthesia may be applied.

3. Approach
For this treatment, a volar approach to the MCP joint is normally used for irreducible dislocations.
4. Reduction
Closed reduction
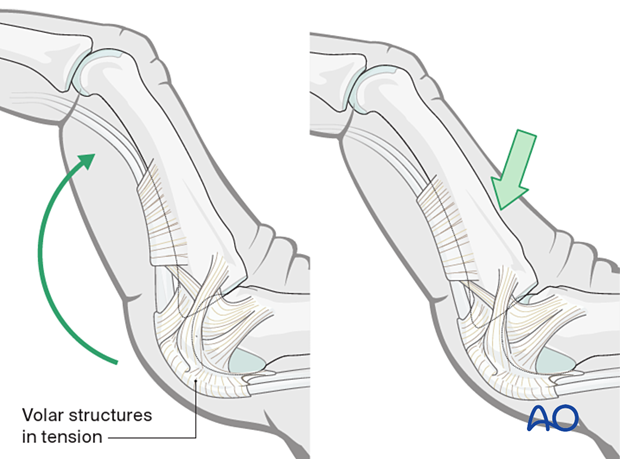
Dislocation usually occurs as an extension deformity.
This can be reduced by increasing the deformity with some dorsally applied pressure on the proximal phalanges to reduce the joint. This keeps the volar structures in tension and reduced the risk of soft-tissue interposition.
Stability evaluation
Confirm reduction with an image intensifier and check the joint stability by flexion and extension. This should show congruent movement compared with the adjacent joints.
Open reduction
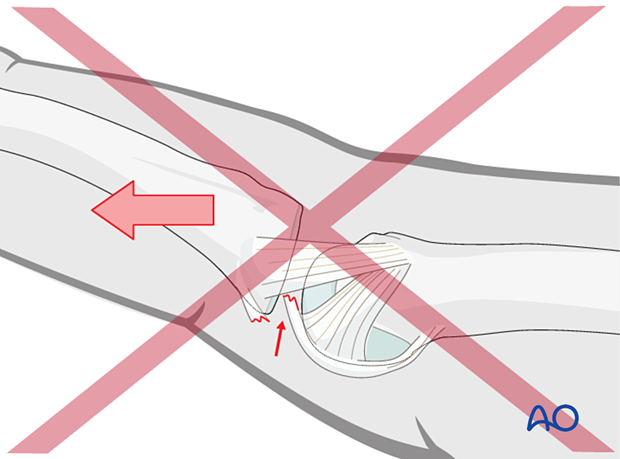
If congruent reduction cannot be achieved, often due to interposed soft tissue, an open reduction is necessary.
Remove the obstructing soft tissues or fragments, reduce the joint and confirm congruity and stability of the joint.
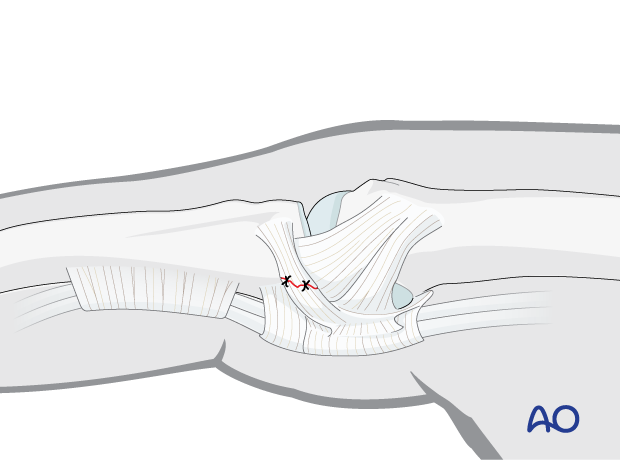
Repair the joint capsule and close the skin incision.
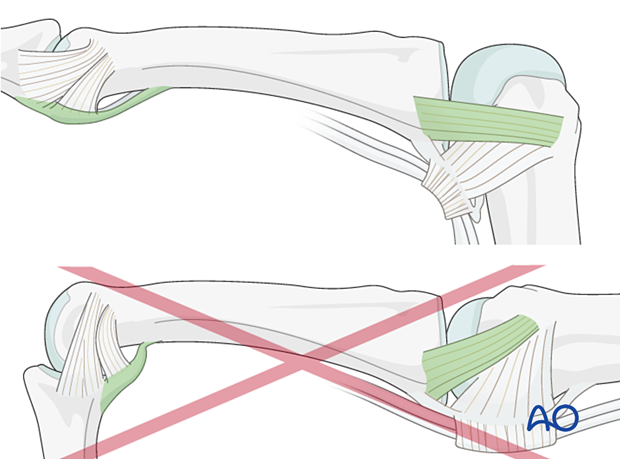
5. Ligament repair
If there is insufficient MCP joint stability, ligament repair of the volar plate or sagittal band and the extensor mechanism may be required.
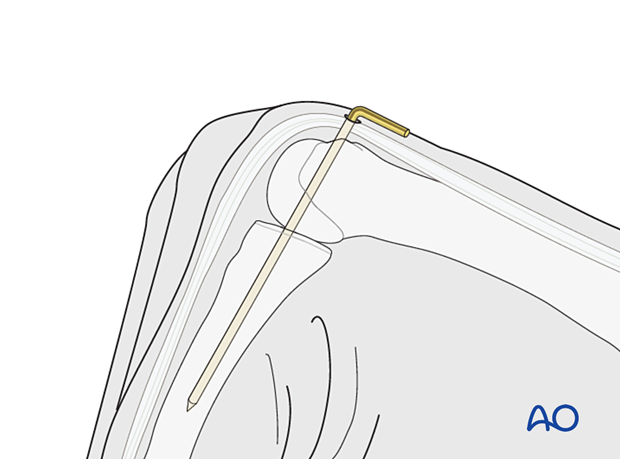
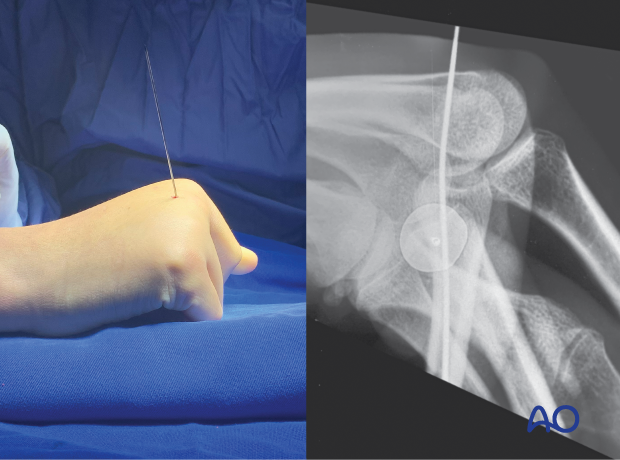
6. Joint transfixation with a temporary K-wire
If there is persistent instability, transfix the joint temporarily with a K-wire. Flex the MCP joint to 90° and insert the K-wire in an antegrade fashion through the head of the metacarpal into the medullary canal of the proximal phalanx.
Bend the end of the K-wire above the skin and cut it with enough length to avoid migration.
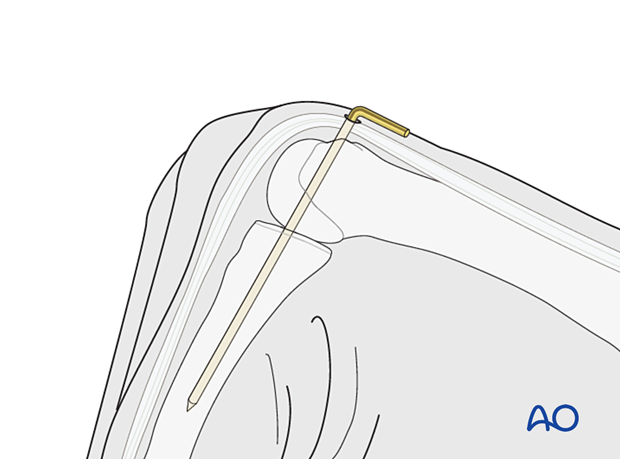
Intraoperative view of K-wire transfixation of the 2nd MCP joint
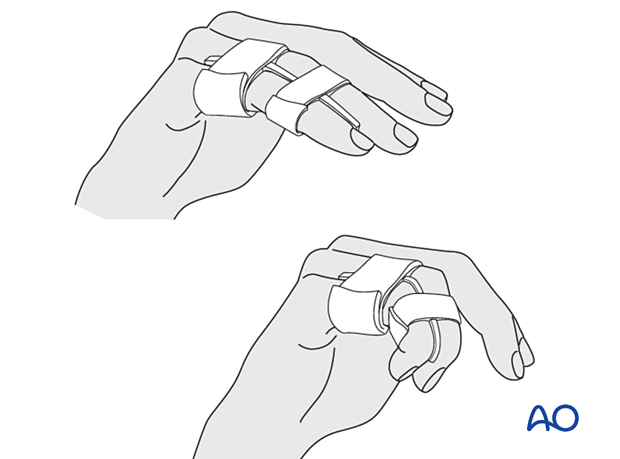
7. Buddy strapping
If the joint is stable, buddy strapping only may be considered.
Strap the injured finger to a neighboring finger.
The strapping should leave the joints free for mobilization.
Direct skin contact with adjacent fingers should be prevented by placing gauze pads between them.
8. Application of a dorsal splint
The hand is supported with a dorsal splint for at least 3 weeks. This would allow for finger movement and help with pain and edema control.
The hand should be splinted in an intrinsic plus (Edinburgh) position:
- Neutral wrist position or up to 15° extension
- MCP joint in 90° flexion
- PIP joint in extension
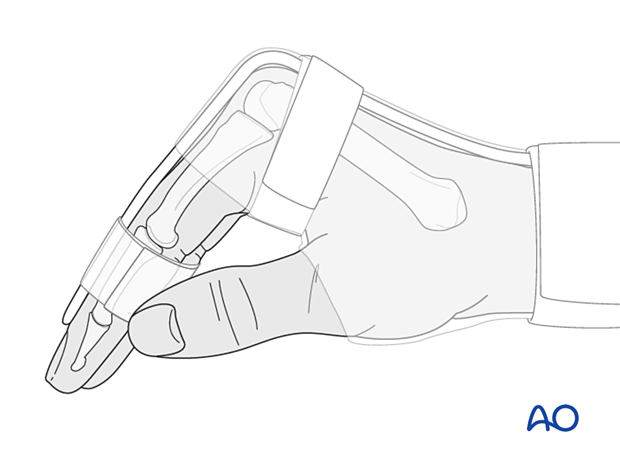
The reason for splinting the MCP joint in flexion is to maintain its collateral ligament at maximal length, avoiding scar contraction.
PIP joint extension in this position also maintains the length of the volar plate.
9. Aftercare
Postoperative phases
The aftercare can be divided into four phases of healing:
- Inflammatory phase (week 1–3)
- Early repair phase (week 4–6)
- Late repair and early tissue remodeling phase (week 7–12)
- Remodeling and reintegration phase (week 13 onwards)
Full details on each phase can be found here.
Follow-up
X-ray checks of joint position have to be performed immediately after the splint has been applied.
Follow-up x-rays with the splint should be taken after 1 week, and possibly every 2 weeks.
The K-wire can be removed 2 weeks after surgery.
Splinting is continued until about 4 weeks after the injury. At that time, an x-ray without the splint is taken to confirm healing and range of motion should be pain-free.
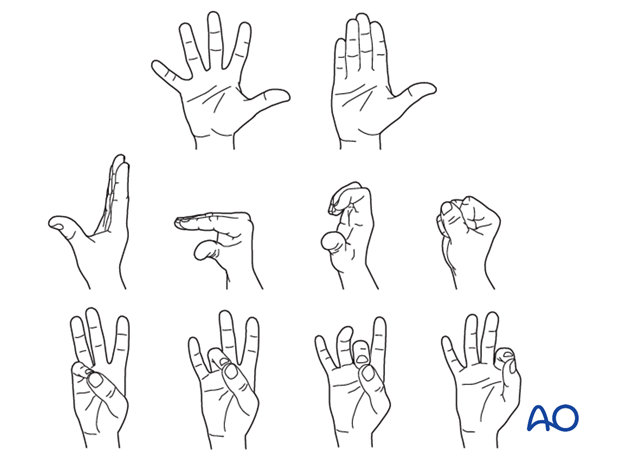
Mobilization
Splinting can then usually be discontinued, and active mobilization is initiated. Functional exercises are recommended.