Volar approach to the metacarpophalangeal joint
1. General considerations
Indications
This approach is used for the surgical treatment of fracture-dislocations of the metacarpophalangeal (MCP) joint.
AO teaching video
Palmar approach to metacarpophalangeal joint of the finger
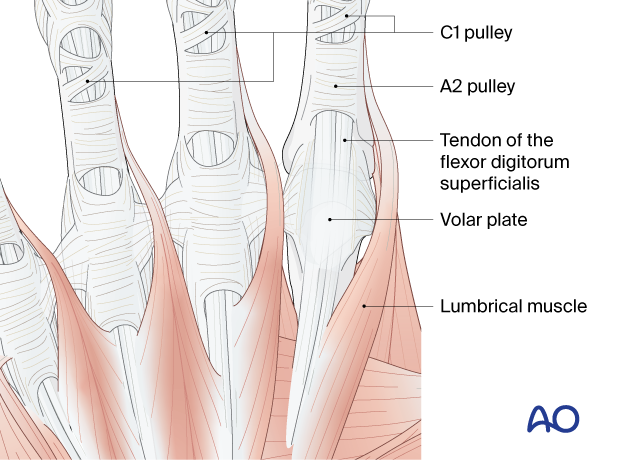
2. Surgical anatomy
Tendinous anatomy
The tendons of the flexor digitorum superficialis and profundus are closely applied to the volar plate and volar capsule of the MCP joints.
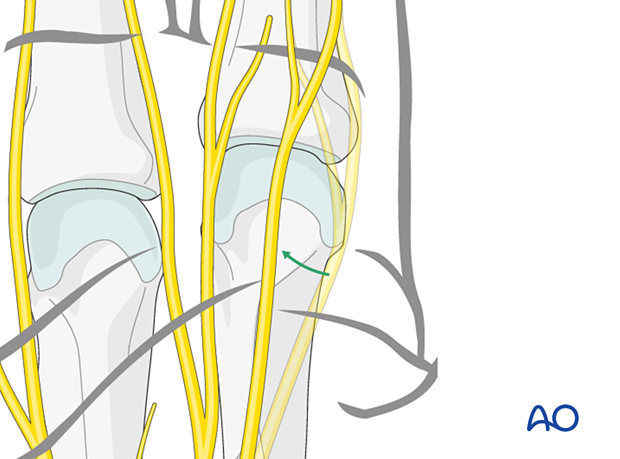
Nerve identification
In the thin subcutaneous tissue, identify and protect the collateral neurovascular bundles of the ulnar and median nerves.
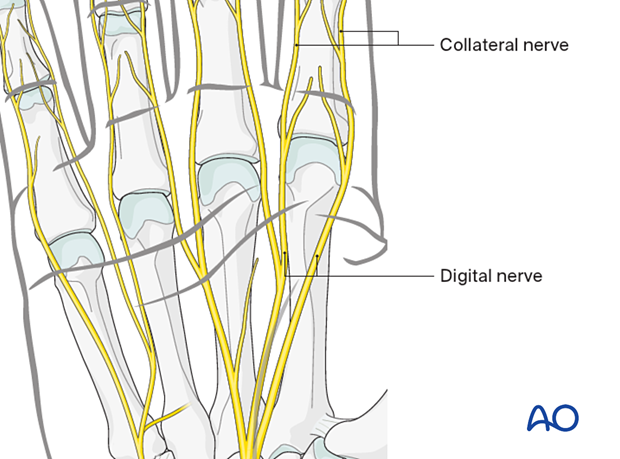
Sometimes the digital nerve is dislocated volarly with the metacarpal head. Take care to identify the nerve during the approach.
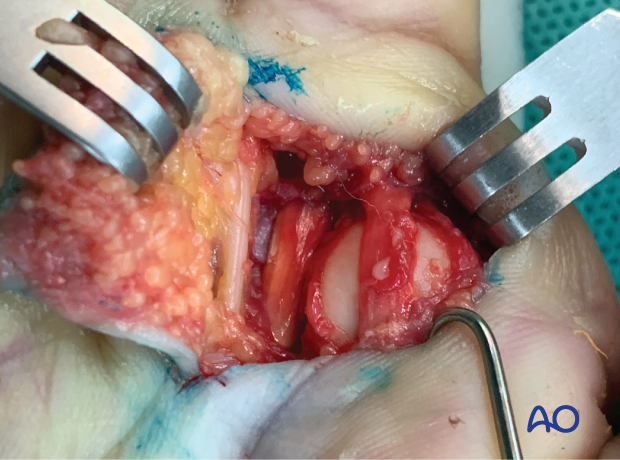
Intraoperative photo showing a volar approach to the 2nd metacarpal head with displacement of the digital nerve after a metacarpophalangeal joint dislocation
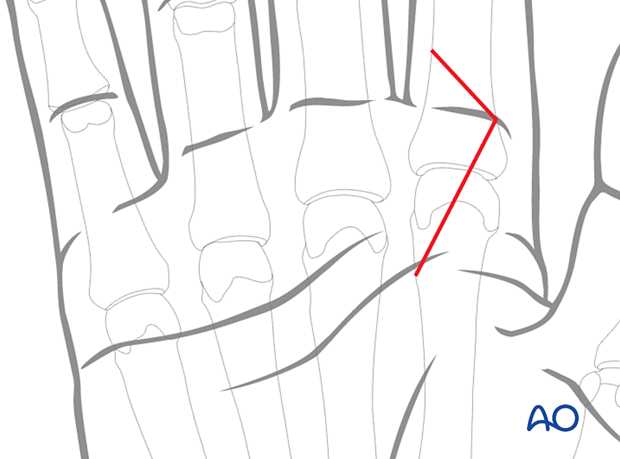
3. Skin incision
Make a Z-shaped incision over the MCP joint with the apex either radially or ulnarly at the level of the skin crease.
In case of multiple neighboring incisions, the apexes should point in the same direction to avoid ischemia and necrosis of the intervening skin flaps.

Extension of the incision
According to the dislocation complexity or soft-tissue interposition, the incision can be extended proximally in a Z-shape respecting the natural skin creases. This helps to avoid contracture of the skin.

4. Exposure of the retinaculum and A1 pulley
The skin flaps are retracted to expose the distal part of the flexor retinaculum and A1 pulley.
Be aware of overretraction to avoid damage to the nerves.
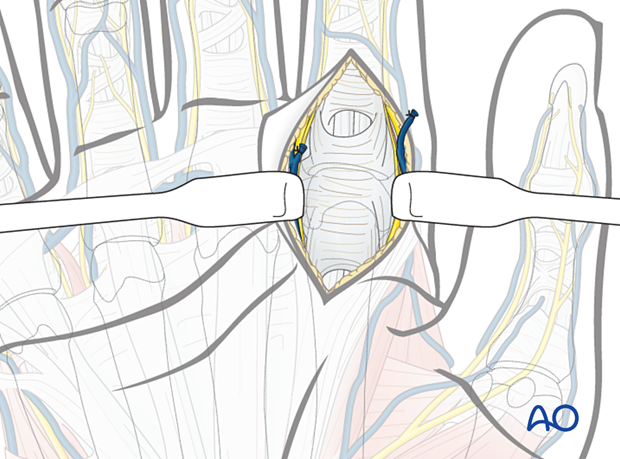
5. Exposure of the joint
Identify and protect the digital nerves.
The flexor digitorum superficialis and profundus are sharply dissected from the volar plate and capsule and retracted to expose the volar aspect of the joint. Usually, in a dislocation, the volar joint capsule is ruptured and may be interposed in the joint space.
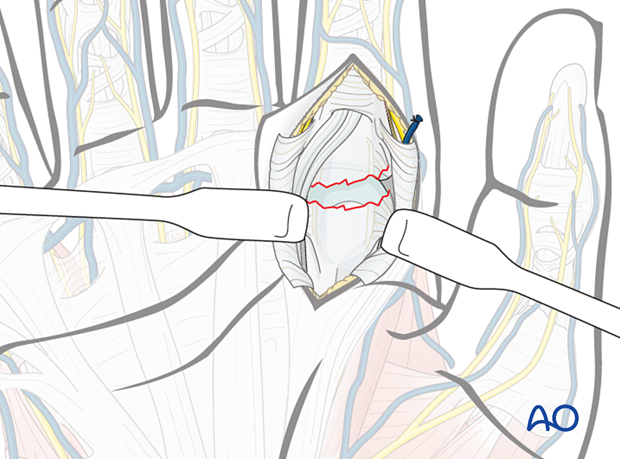
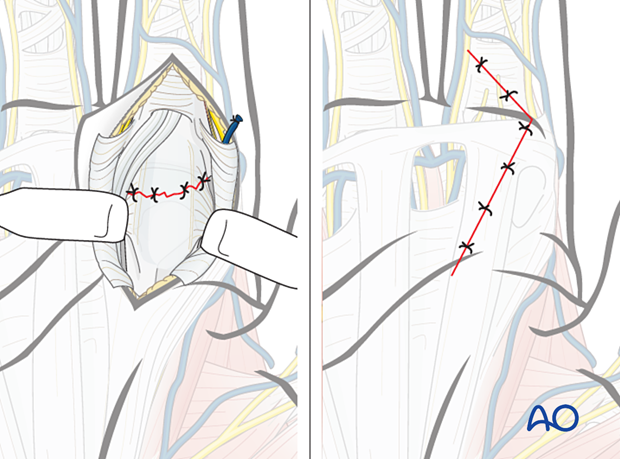
6. Wound closure
The joint capsule is repaired with fine sutures. The flexor tendon is repositioned. The skin is closed in a standard manner.
The A1 pulley does not need repair, as this may lead to contracture of the tendon sheath with restriction of flexor tendon excursion.