Bridge plating
1. General considerations
Multifragmentary fractures are best treated with bridge plating.
ORIF provides sufficient stability for immediate mobilization, reducing the risk of joint stiffness and tendon adhesions.
Even in the hand, which is well vascularized, small fragment comminution means poor soft-tissue attachment to the fragments and, thereby, compromised vascularity.
Some wedge fracture patterns, eg, with a small wedge fragment, cannot be stabilized with lag screw and plate fixation and therefore need bridge plating.
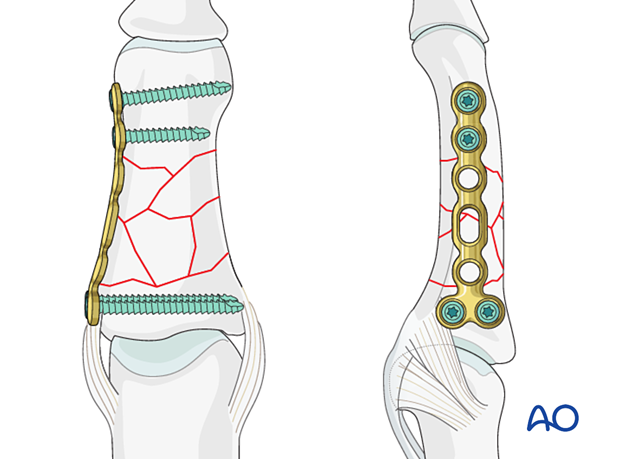
The plate may be applied laterally or dorsally. The lateral application is preferred as it avoids disturbance of the extension mechanism insertion.
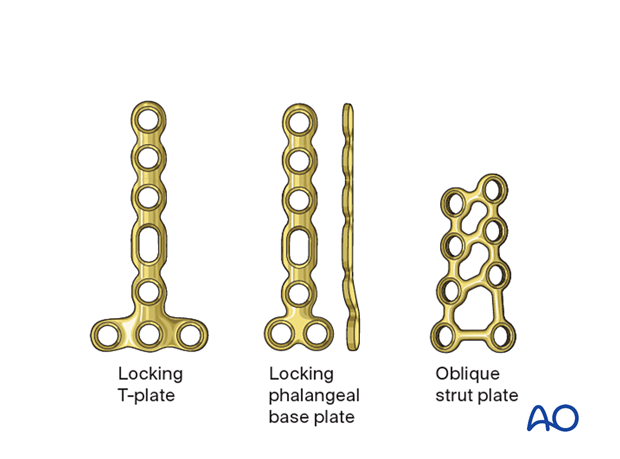
For bridge plating, several plate types (low profile) may be used:
- T-plate; dorsal
- Strut plate; dorsal
- Phalangeal base plate; lateral
The selection of the plate depends on the fracture pattern and should allow for at least two screws in the proximal and distal main fragment.
In this procedure, bridge plate fixation of a metadiaphyseal multifragmentary fracture with a lateral phalangeal base plate is shown.
2. Patient preparation
Place the patient supine with the arm on a radiolucent hand table.
3. Approaches
For this procedure the following approaches may be used:
4. Reduction
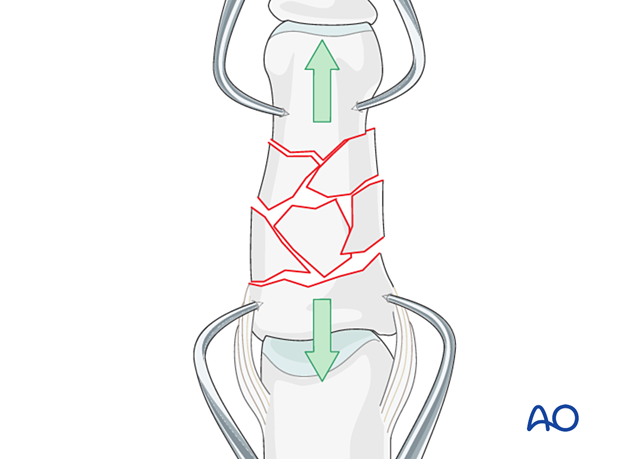
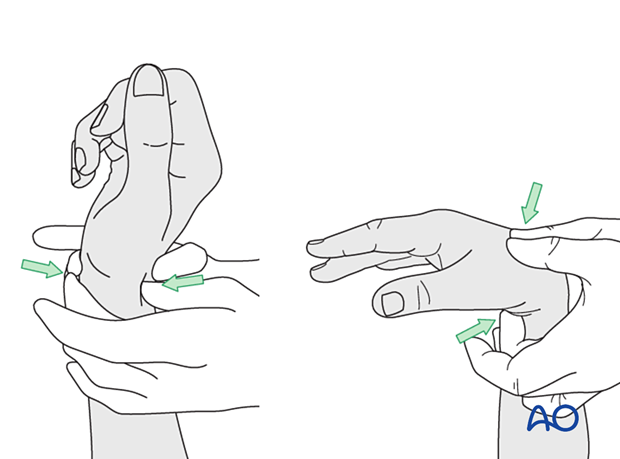
Gaining length
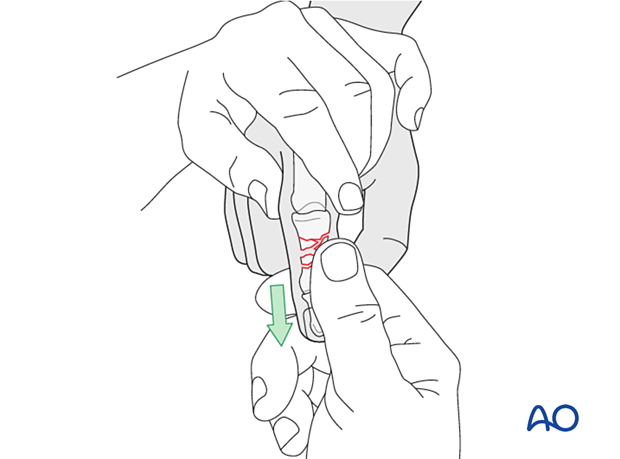
Length can be gained by manual traction ...
...or using two forceps.
Confirm length and rotation clinically and with an image intensifier.
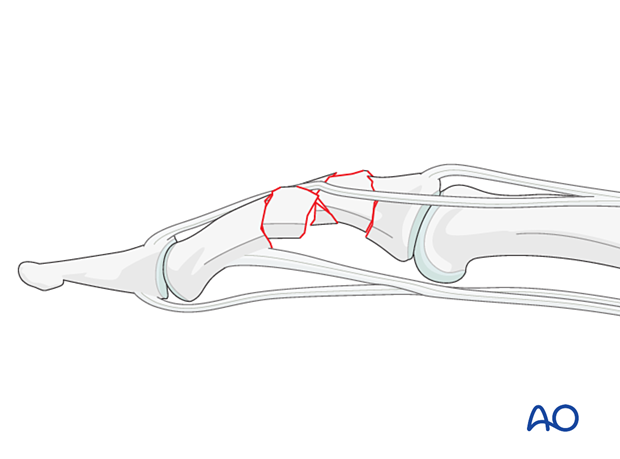
Sometimes indirect reduction may be prevented by interposition of the lateral band.
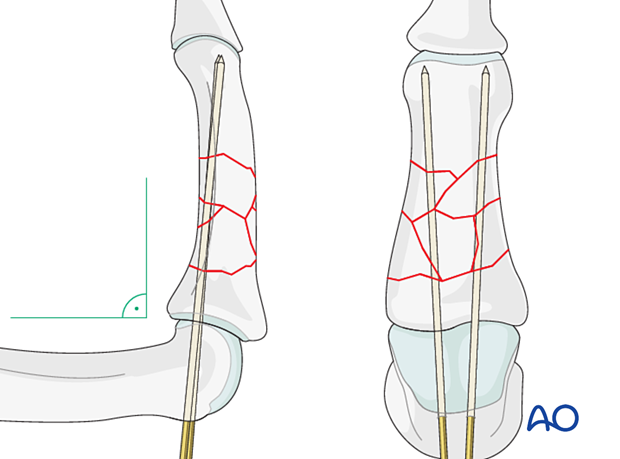
Provisional K-wire fixation
Provisional fracture stabilization can be provided by K-wires.
If the base fragment is short, insert the K-wires, with the PIP joint in 90° of flexion, through the proximal phalangeal head and PIP joint through the base, medullary canal, and into the head of the middle phalanx.
If the base fragment is large enough, insertion through the tip of the finger may be selected.
To avoid conflicts with the plate screws, the K-wires should be inserted slightly oblique to the phalangeal axis.
Take great care to control rotational alignment.
The K-wire provides angular alignment in both planes but does not control rotation.
5. Checking alignment
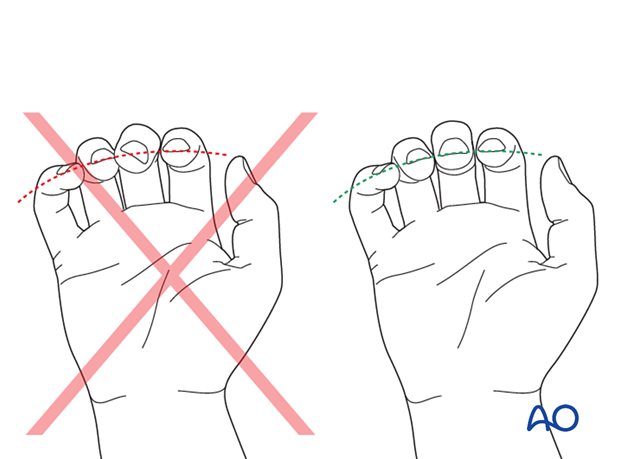
Identifying malrotation
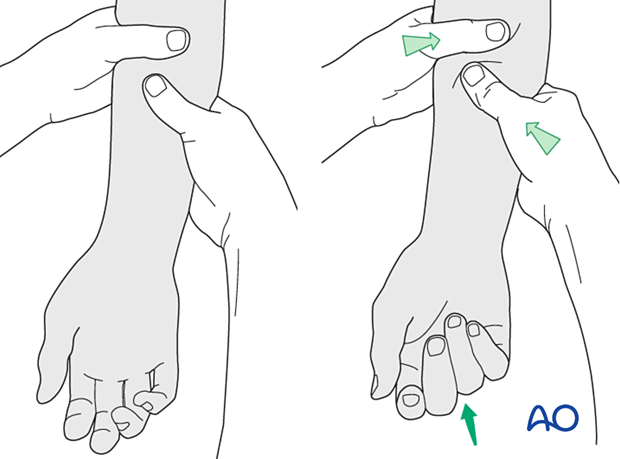
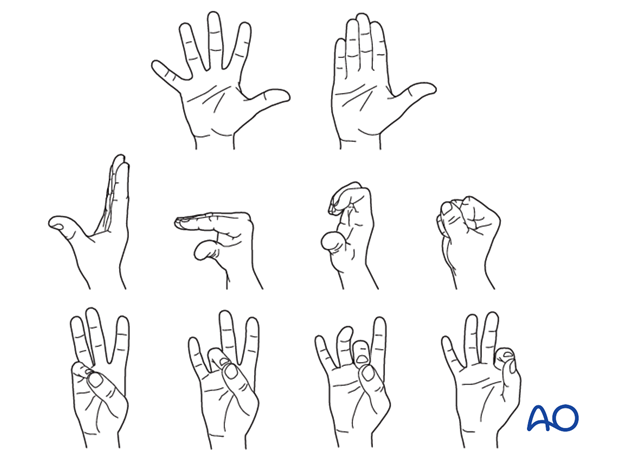
At this stage, it is advisable to check the alignment and rotational correction by moving the finger through a range of motion.
Rotational alignment can only be judged with the fingers in a degree of flexion, and never in full extension. Malrotation may manifest itself by overlap of the flexed finger over its neighbor. Subtle rotational malalignments can often be judged by tilting of the leading edge of the fingernail when the fingers are viewed end-on.
If the patient is conscious and the regional anesthesia still allows active movement, the patient can be asked to extend and flex the finger.
Any malrotation is corrected by direct manipulation and later fixed.
Using the tenodesis effect when under anesthesia
Under general anesthesia, the tenodesis effect is used, with the surgeon fully flexing the wrist to produce extension of the fingers and fully extending the wrist to cause flexion of the fingers.
Alternatively, the surgeon can exert pressure against the muscle bellies of the proximal forearm to cause passive flexion of the fingers.
6. Plate fixation
Plate trimming
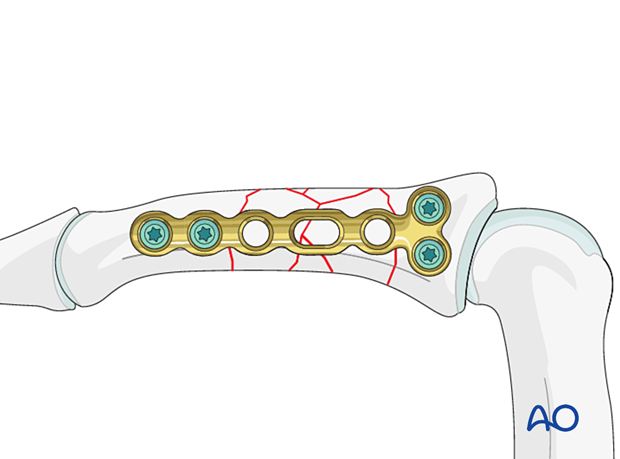
Adapt the plate length to fit the length of the middle phalanx. Avoid sharp edges, which may be injurious to the tendons. At least two screws need to be inserted on either side of the fracture zone.
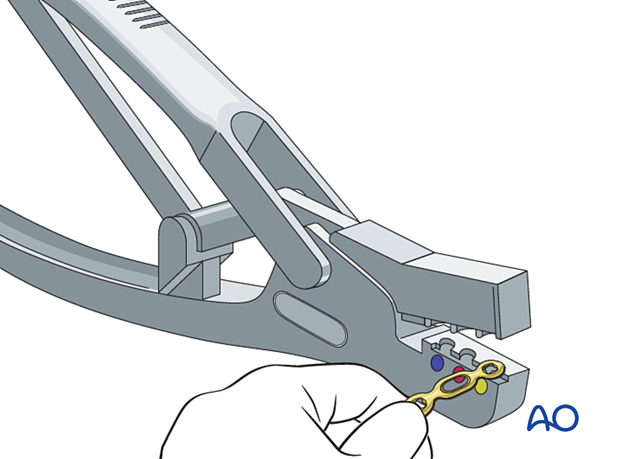
Plate positioning
Place the plate slightly dorsal to the midaxial line of the bone, allowing at least two screws in both main fragments.
Keep the plate in place with the atraumatic forceps.
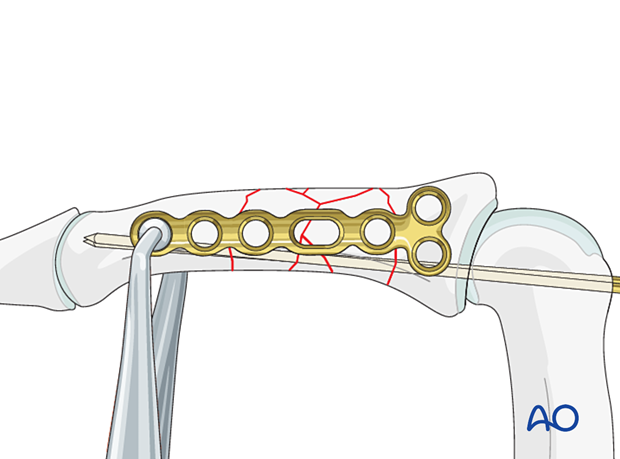
Screw insertion
Insert the screw according to the fracture configuration and stability.
Start with insertion of a locking head screw in the articular block.
Check the plate position and rotational alignment with an image intensifier and adjust it if necessary.
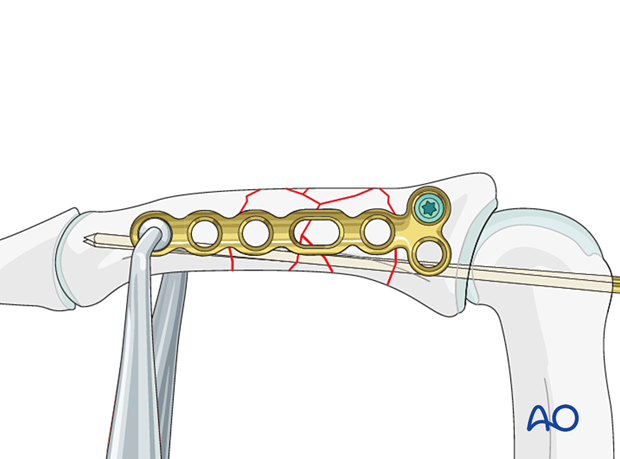
Add a screw in the other main fragment distal to the fracture zone.
Recheck the plate position and rotational alignment with an image intensifier and adjust it if necessary.
Complete the screw fixation according to the fracture configuration.
Cover the plate with periosteum to avoid adhesion between the tendon and the implant leading to limited finger movement.
7. Final assessment
Confirm fracture reduction and stability and implant position with an image intensifier.
8. Aftercare
Postoperative phases
The aftercare can be divided into four phases of healing:
- Inflammatory phase (week 1–3)
- Early repair phase (week 4–6)
- Late repair and early tissue remodeling phase (week 7–12)
- Remodeling and reintegration phase (week 13 onwards)
Full details on each phase can be found here.
Postoperative treatment
If there is swelling, the hand is supported with a dorsal splint for a week. This should allow for movement of the unaffected fingers and help with pain and edema control. The arm should be actively elevated to help reduce the swelling.
The hand should be immobilized in an intrinsic plus (Edinburgh) position:
- Neutral wrist position or up to 15° extension
- MCP joint in 90° flexion
- PIP joint in extension
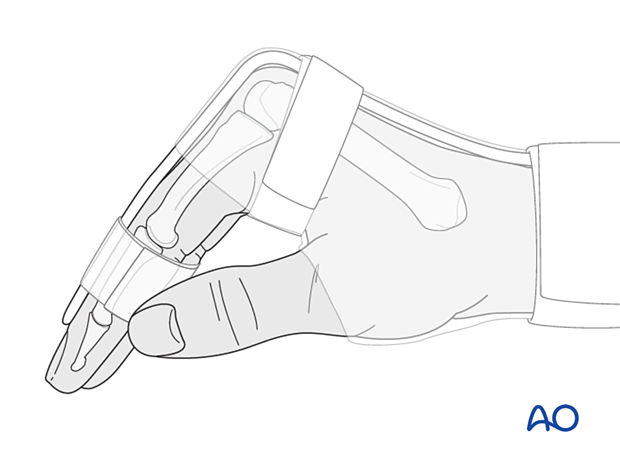
The MCP joint is splinted in flexion to maintain its collateral ligaments at maximal length to avoid contractures.
The PIP joint is splinted in extension to maintain the length of the volar plate.
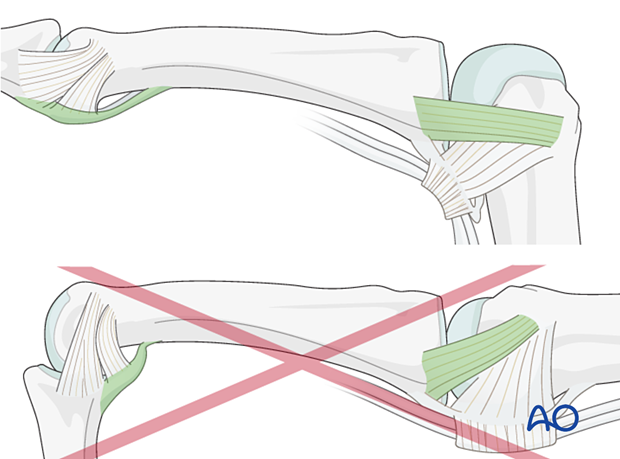
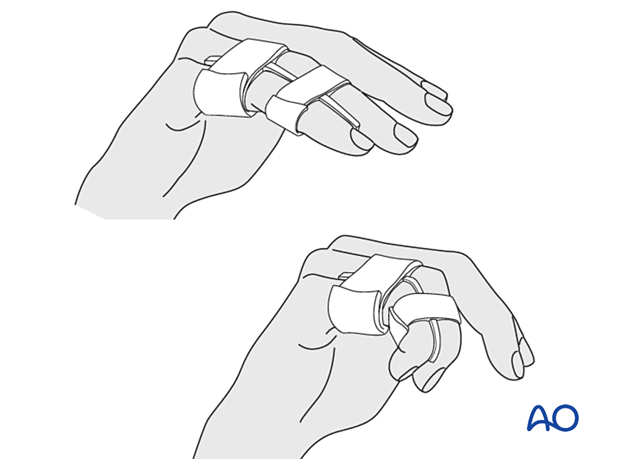
After swelling has subsided, the finger is protected with buddy strapping to neutralize lateral forces on the finger until full fracture consolidation.
Mobilization
To prevent joint stiffness, the patient should be instructed to begin active motion (flexion and extension) of all nonimmobilized joints immediately after surgery.
Follow-up
The patient is reviewed frequently to ensure progression of hand mobilization.
In the middle phalanx, the fracture line can be visible in the x-ray for up to 6 months. Clinical evaluation (level of pain) is the most important indicator of fracture healing and consolidation.
Implant removal
The implants may need to be removed in cases of soft-tissue irritation.
In case of joint stiffness or tendon adhesion restricting finger movement, arthrolysis or tenolysis may become necessary. In these circumstances, the implants can be removed at the same time.













