ORIF - Compression Plating
1. General considerations
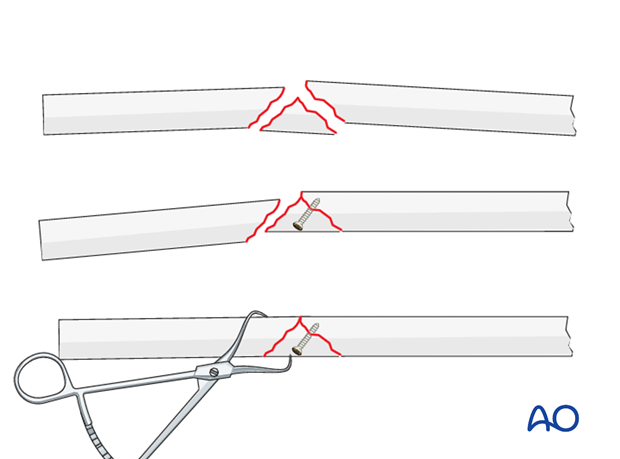
In the past, wedge fractures have usually been fixed rigidly. The underlying principle focused on mechanical issues, not on biology. Today, biology takes precedence and for this reason not all wedge fragments are incorporated rigidly into the fixation.Small wedge fragments that do not have a significant effect on stability should not be addressed (they will become incorporated into the fracture by indirect bone healing). Larger wedge fragments that contribute to the stability of the fixation, are fixed to one main fragment. Sometimes, fixation of the wedge to one main fragment helps reduction of the residual fracture.
If a lag screw is inserted separate from the plate, a 2.7 mm screw is often used, depending on the size of the bone, for biological reasons, and to reduce the risk of splitting the wedge.
If a lag screw is inserted through a 3.5 mm plate, a 3.5 mm screw should be used.
2. Principles
Decision making based on wedge morphology
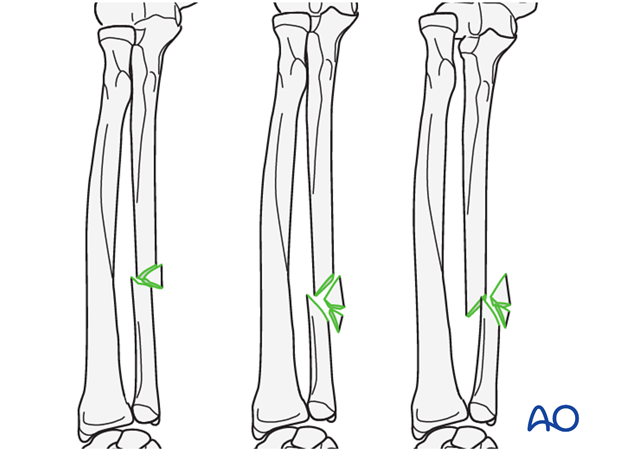
If an intact wedge occupies the majority of the diameter of the bone, there is minimal contact between the two main fragments and the wedge should be fixed to at least one of the main fragments by a lag screw technique. Then, the remaining instability is equivalent to a simple oblique fracture which will lend itself to one of the methods described for such a fracture.
If such a wedge is fragmented, it is unlikely to be suitable for lag screw fixation and bridge plating will often be chosen.
If the wedge occupies less than 50% of the diameter of the bone, there is likely to be sufficient cortical contact between the two main fragments to allow primary fixation by axial compression.
Depending on the exact fracture configuration, there is a “grey zone” in which the area of contact between the two main fragments, the obliquity of the contact zone, the length of the wedge fragment, any fragmentation of the wedge and the quality of the bone will all be factors to be taken into account by the surgeon when deciding which technique to use.
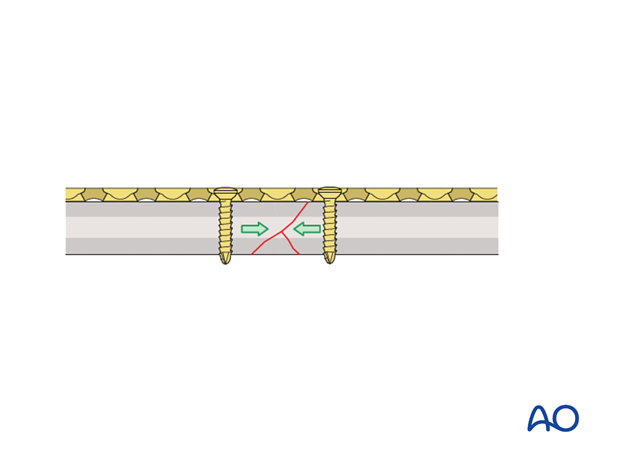
Axial compression
Using self-compressing plates (DCP, LC-DCP, LCP, etc.), axial compression results from eccentric screw (load screw) insertion
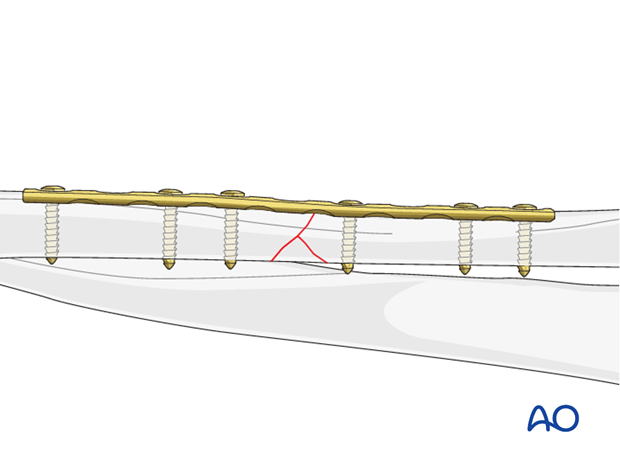
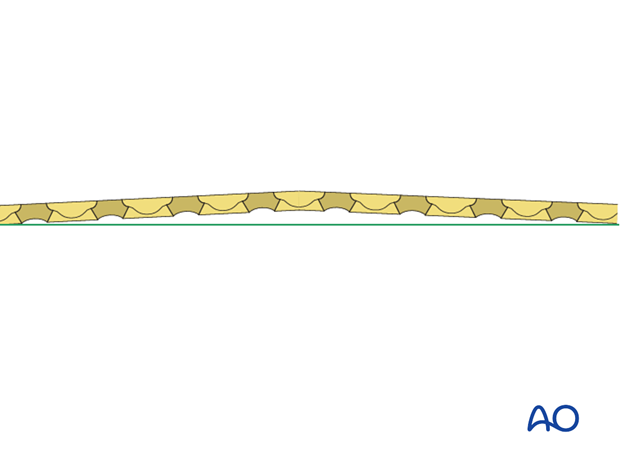
Prebending the plate
In simple transverse fractures, to achieve even compression over the whole fragment contact area, including the far cortex, the plate is slightly prebent.
This principle also applies to partial wedge fractures.
If there is a wedge present opposite the planned plate position it must be borne in mind that compression on the far side of the bone may result in holding the wedge in place, but the risk of extrusion of the wedge cannot be discounted.
Should the wedge become displaced, it will unite by indirect healing, provided its vascularity is not impaired by inappropriate attempts to reduce it. However, the surgeon should bear in mind that until the wedge is healed, there will be increased stress on the plate at the fracture site.
Three options will be described:
- No direct fixation of the wedge fragment
- Fixation of the wedge fragment with a lag screw through the plate
- Fixation of the wedge fragment with a separate lag screw
3. Plate position, length and number of screws
Plate position
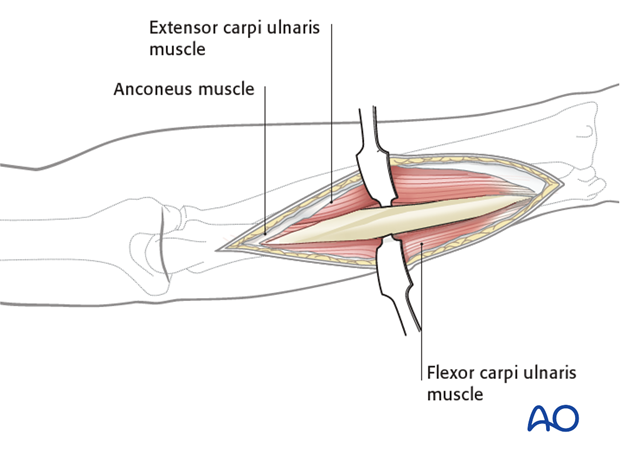
The plate on the ulna can be positioned under the extensor carpi ulnaris muscle (A), under the flexor carpi ulnaris muscle (B), or in the interval between extensor and flexor carpi ulnaris muscles (C). With a more proximal fracture it can be more difficult to place the plate underneath the extensor muscle. With more distal fractures, plates should be placed in the interval between the extensor and flexor carpi ulnaris muscles (C).
While plate position on the tensile (subcutaneous) aspect of the ulna (C) is biomechanically preferable, plate prominence can be a problem and cause irritation. To avoid too superficial a position of the plate, it can be placed towards positions (A) or (B) where it will be covered by the muscle compartment.
In wedge fractures, the plate position must consider the fracture morphology.
In the following procedure, we demonstrate the plate positioned deep to the extensor carpi ulnaris muscle (A).

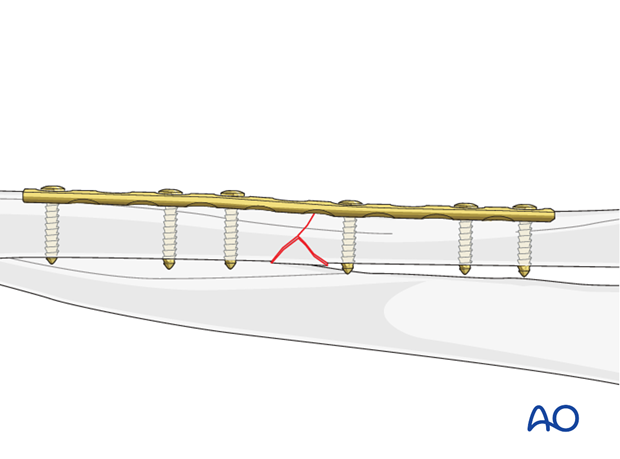
Plate length and number of screws
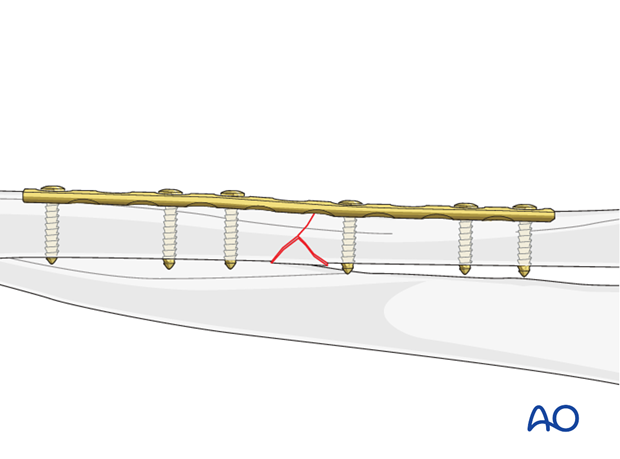
In the forearm, three bicortical screws are required in each main fracture fragment due to the high torsional stresses. For biological reasons, not every plate hole needs to be occupied by a screw. Therefore, in fractures with a wedge fragment, plates with at least 9 holes should be used.
Of necessity, in wedge fractures at least one empty plate hole is usually at the level of the wedge.
4. Patient preparation and approach
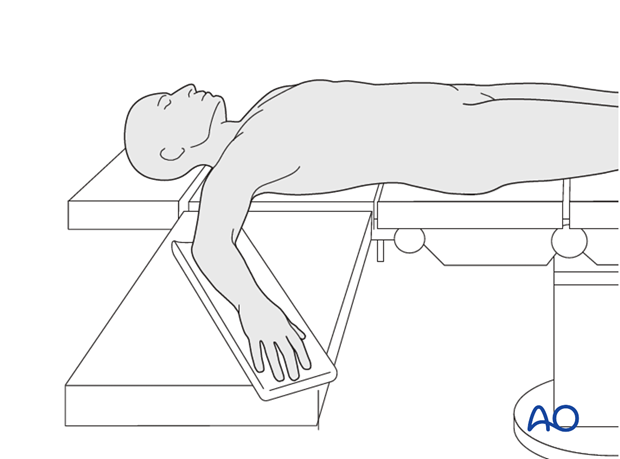
Patient perparation
This procedure is normally performed with the patient in a supine position.
Approach
For this procedure an approach to the ulna is normally used.
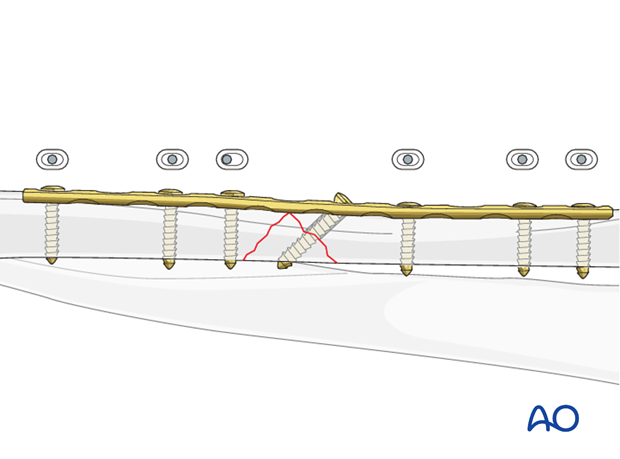
5. No direct fixation of the wedge fragment
Reduction of the two main fragments
Reference for reduction is the cortex opposite to the base of the wedge.
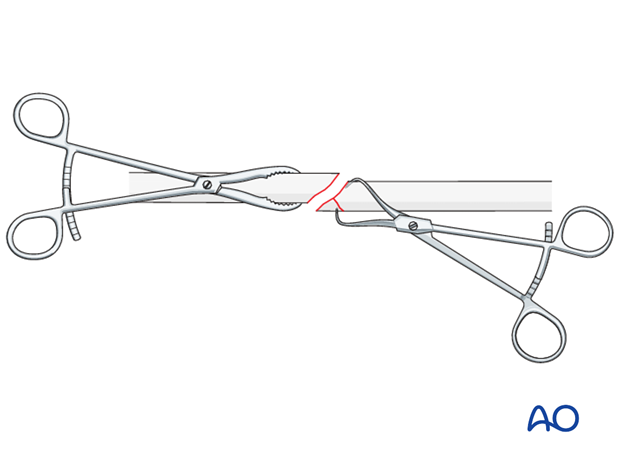
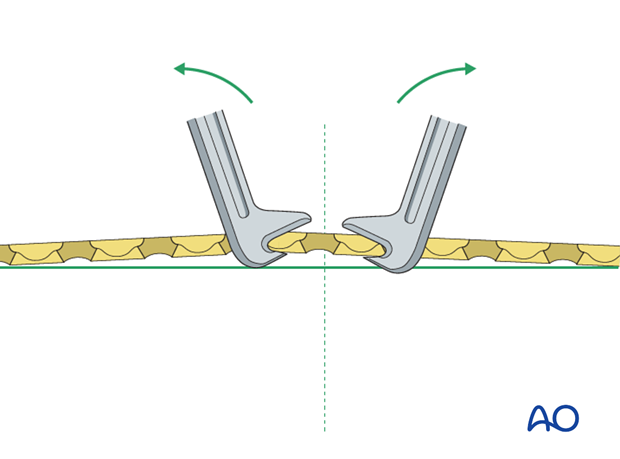
Reduce the main fracture fragments anatomically, using a reduction forceps on each main fragment. The use of blunt reduction forceps can be helpful, particularly if greater forces are required.
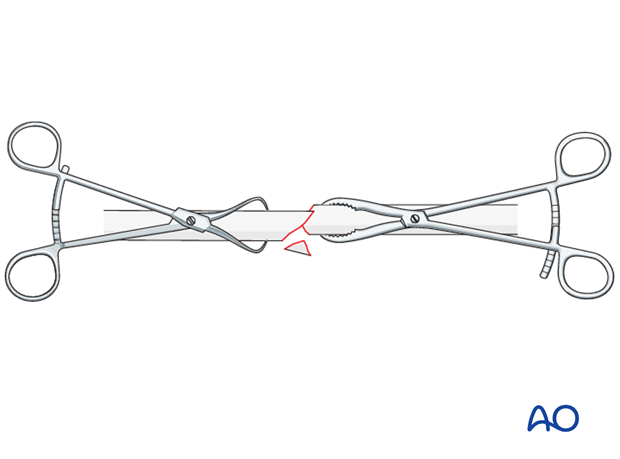
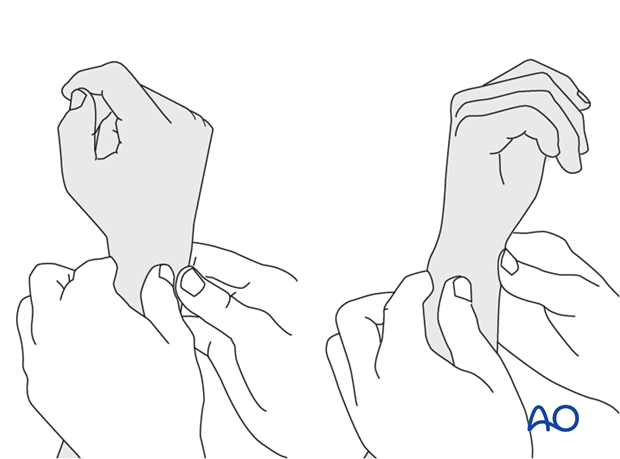
If unstable, temporary stabilization of the small wedge fragment onto one of the main fragments helps anatomical reduction. When performing this maneuver, pointed reduction forceps are preferred. In placing the forceps take care not to interfere with the planned plate position, or to damage the soft-tissue attachments of the wedge. If necessary, apply the forceps through a plate hole.
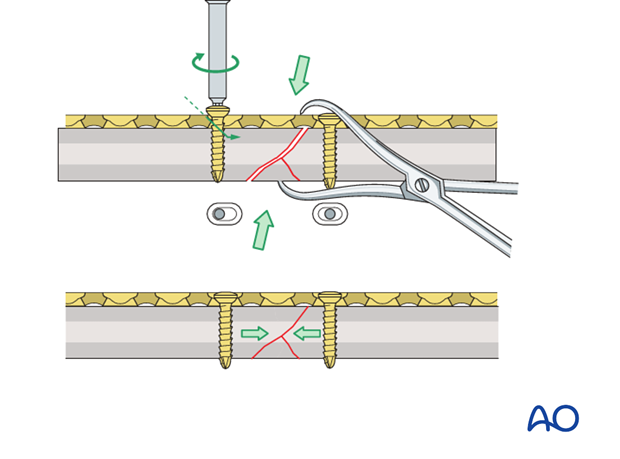
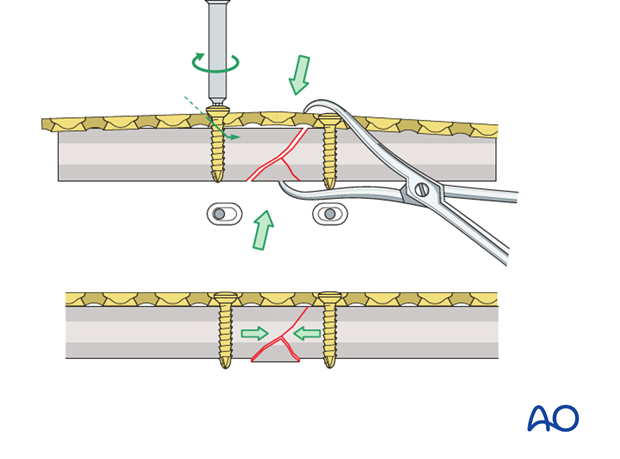
Dynamic compression principle
The holes of the plate are shaped like an angled cylinder. The spherical undersurface of the screw head slides down the inclined cylinder as the screw is tightened.
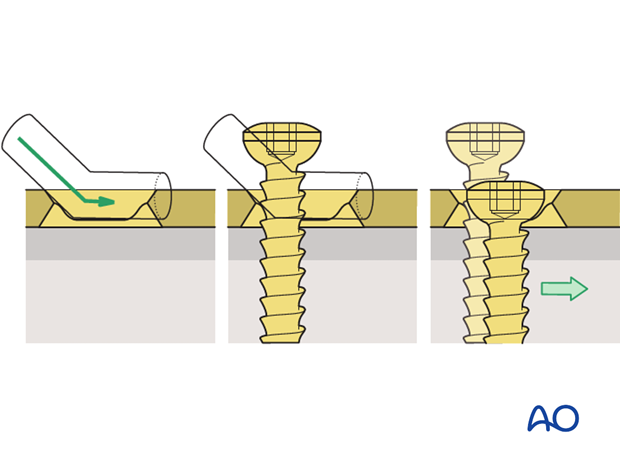
The horizontal movement of the head, as it impacts against the angled side of the hole, results in movement of the bone fragment relative to the plate and leads to compression of the fracture.
Prebend the plate
After the plate has been contoured anatomically to the reduced bone surface, prebend it with the handheld bending pliers, or a pair of bending irons, as explained in the principles section.
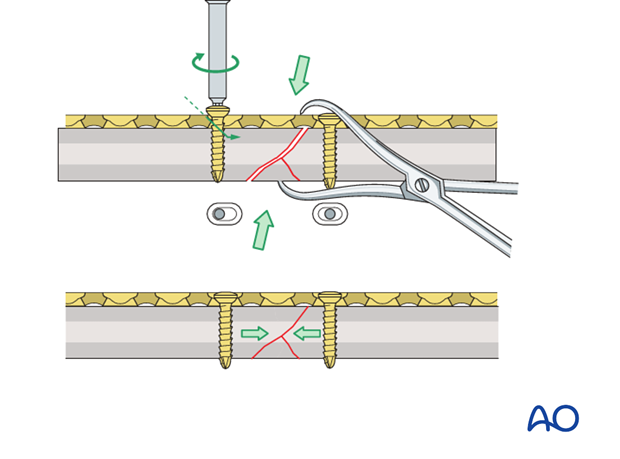
Insert 1st screw
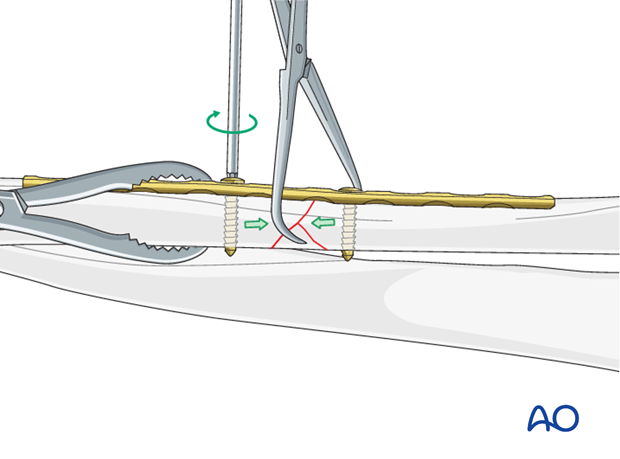
The prebent plate is fixed to one of the main fragments with a screw in a neutral position. A pointed reduction forceps is used to hold the wedge fragment in the reduced position.
A reduction forceps is placed on the opposite fragment to hold it in the reduced position against the plate.
Note: Because of the design of the LC-DCP holes, the neutral drill guides for the LC-DCP have a very slightly eccentric hole and an arrow, which needs always to point towards the fracture line.

Insert 2nd screw eccentrically
A second screw is inserted eccentrically (yellow drill sleeve) into the opposite fragment.
Note: the arrow on the drill sleeve has to point towards the fracture line.
Tighten load screw
By tightening the eccentrically-inserted screw, axial compression is achieved. Retain the pointed reduction forceps, while the axial compression is being applied.
Insert additional screws
All other screws are inserted in a neutral mode (green drill sleeve) and do not serve to increase compression.
After all screws have been inserted, any reduction forceps can be removed. Note that the wedge can slightly displace at this stage, which is quite acceptable.
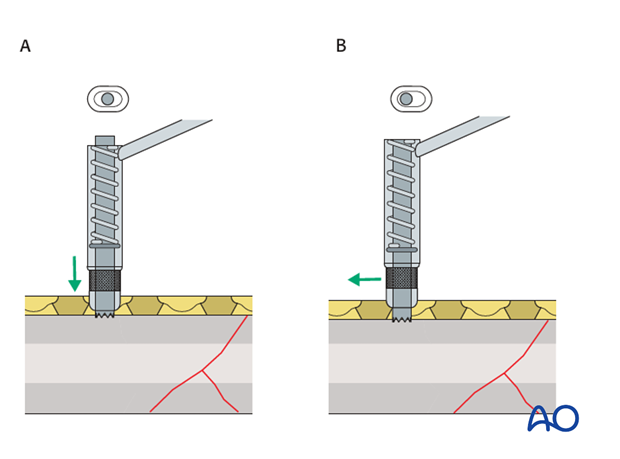
Pearl: alternative drill sleeve
For inserting screws into the limited contact dynamic compression plate (LC-DCP), the Universal Drill Guide can be used as well. When this drill guide is pressed into the plate hole, the screw position will be neutral (A). When it is held against the end of the plate hole, without exerting downward pressure, the screw position will be eccentric (B).
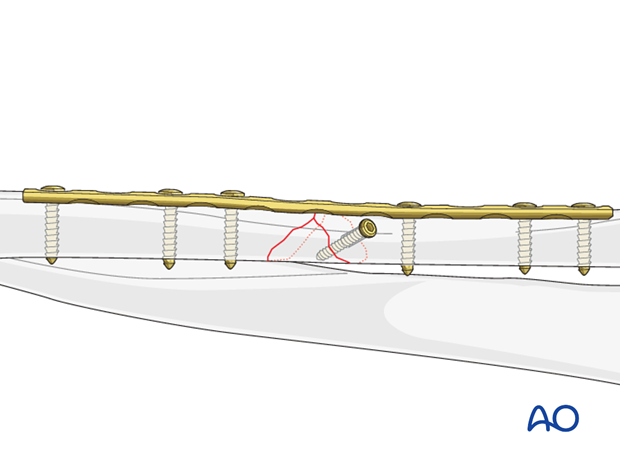
6. Fixation of the wedge fragment with a lag screw through the plate
Reducing and fixing wedge fragment to one main fragment
If possible, reduce the large wedge fragment(s) to one of the main fragments. The main fragment with the more oblique fracture line is often preferred. A smaller i.e. 2.7 mm or 2.0 mm lag screw may sometimes be appropriate, if the fragment(s) is small.
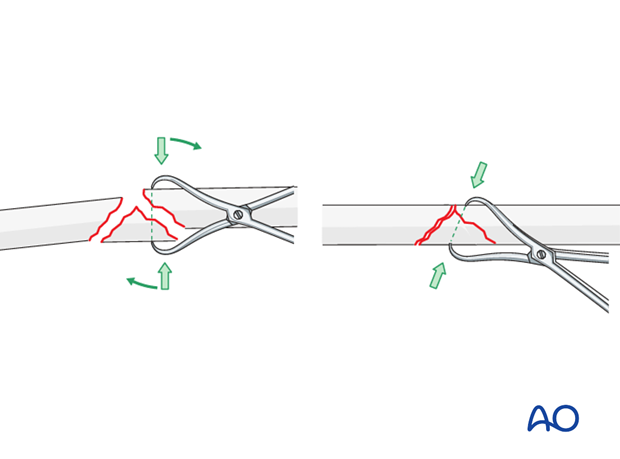
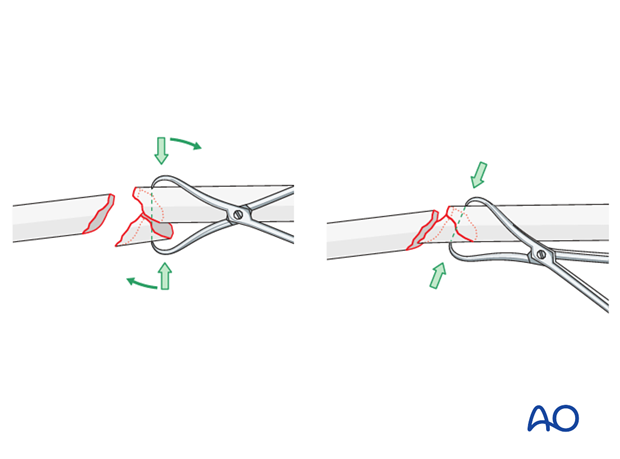
Use of reduction forceps
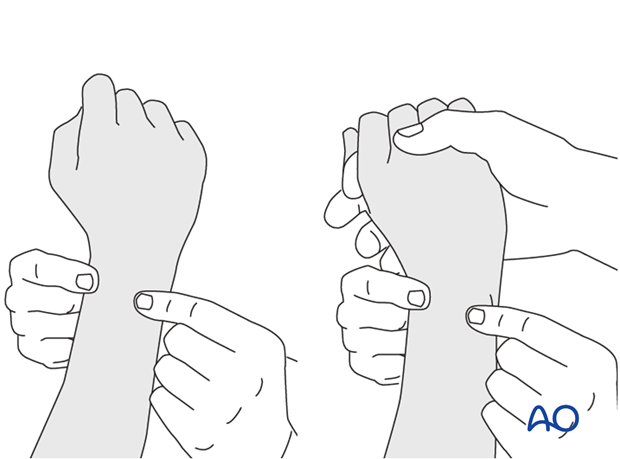
Anatomical reduction of the wedge fragment is achieved by using a pointed reduction forceps. Often, twisting the forceps aids the reduction.
Apply the plate
The plate should be anatomically contoured to the reduced bone surface, but with the addition of a slight prebend.
Apply the plate to the main fragment and hold it in position with a blunt reduction forceps. Should this result in any loss of position of the wedge fragment, re-reduction should be undertaken by adjustment of the pointed forceps.
Ensure that the plate hole for the interfragmentary lag screw is in the correct position for a lag screw through the plate and into the wedge.
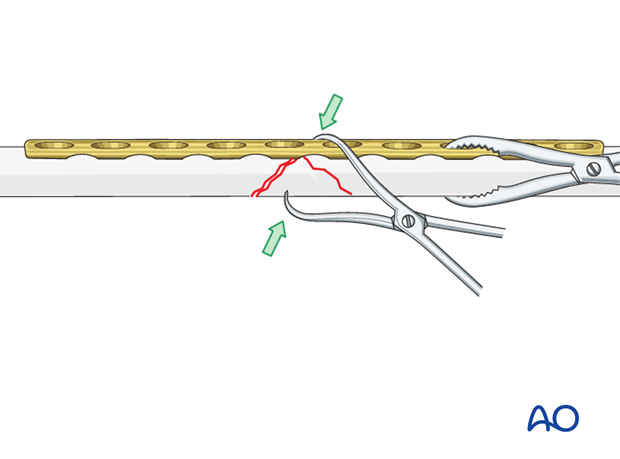
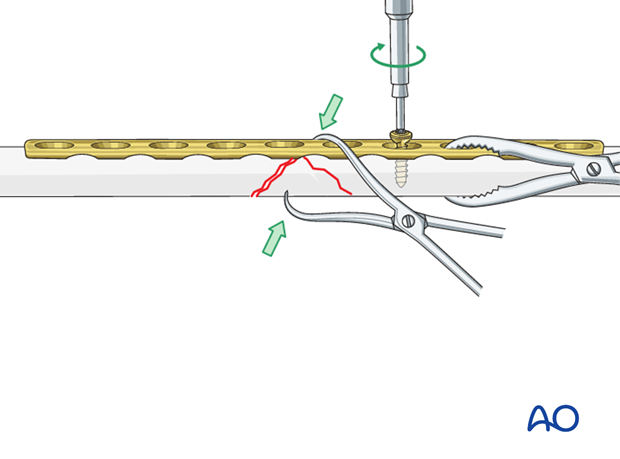
Fix the plate to one main fragment
Fix the plate to the bone with a screw in neutral mode.
The blunt reduction forceps can now be removed.
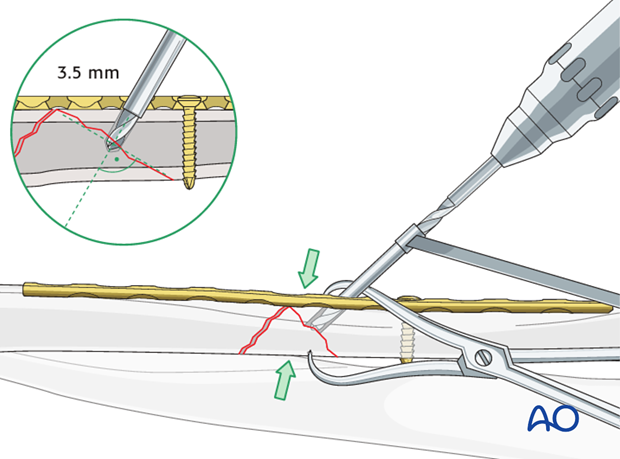
Drill gliding hole through plate
The interfragmentary lag screw can then be inserted through the appropriate plate hole.
Using a 3.5 mm drill sleeve and a 3.5 mm drill bit, drill a gliding hole in the near cortex.
Ensure that the direction of the drill is as perpendicular to the fracture plane as possible.
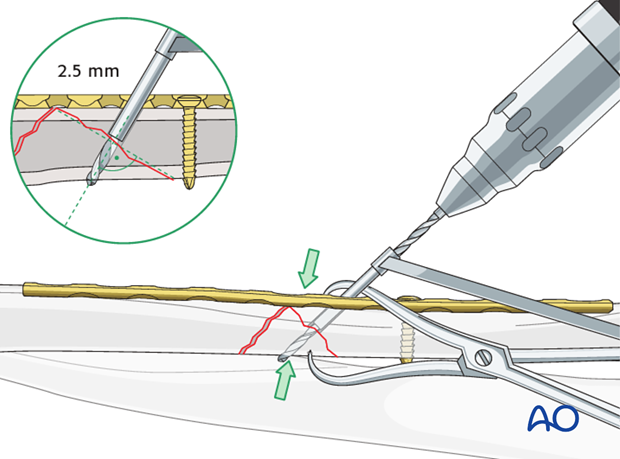
Thread hole: guide in gliding hole
Insert the sleeve of the 3.5 mm / 2.5 mm drill guide through the plate and into the gliding hole. Check that the anatomical reduction of the wedge fragment is maintained and use a 2.5 mm drill bit to drill a pilot hole just through the far cortex of the wedge.
Measure for screw length
Use a depth gauge through the plate to measure for screw length.
Measure the longer side of the oblique drill hole, as shown, to ensure sufficient screw length.
A screw should protrude 1-2 mm through the opposite cortex to ensure maximal thread purchase. However, too long a screw may be tender, or injure soft tissues.
Tap the pilot hole
Using a 3.5 mm cortical tap with the corresponding drill sleeve to protect adjacent soft tissues, create a thread in the pilot hole of the far cortex of the wedge.
This maneuver is not necessary when using self-tapping screws.
Lag screw insertion
Insert the lag screw through the plate and carefully tighten it, making sure that the wedge fragment stays reduced and is compressed.
Reduce wedge to second main fragment
Remove the pointed reduction forceps and use it to reduce the wedge to the other main fragment. Ensure that the plate is correctly aligned to the other main fragment and hold its position using a blunt reduction forceps.
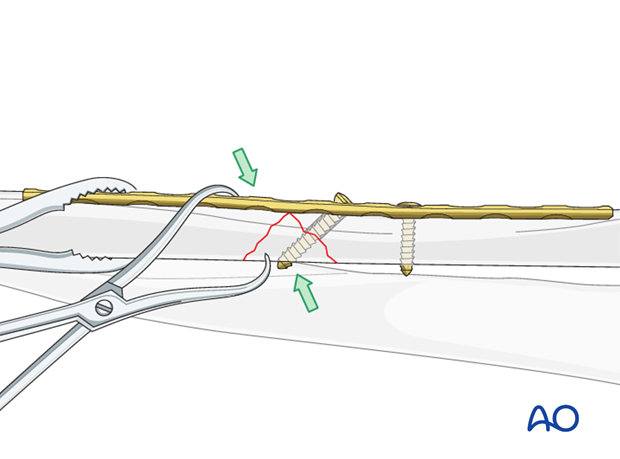
Plate fixation
Fix the plate to the bone using three 3.5 mm bicortical cortex screws in each main fragment. The first screw into the main fragment that is not attached by a lag screw is inserted eccentrically. As this load screw is tightened, take great care not to over-compress. The purpose of this axial compression is to close the fracture gap without producing excessive interfragmentary compression, for fear that the wedge fragment could be split.
All other screws are then inserted in neutral positions.
7. Fixation of the wedge fragment with a separate lag screw
Reducing and fixing wedge fragment to one main fragment
Reduce the large wedge fragment to one of the main fragments. The main fragment with the more oblique fracture line is often preferred.
Use of reduction forceps
Anatomical reduction of the wedge fragment is achieved by using a pointed reduction forceps. Often, twisting the forceps aids the reduction.
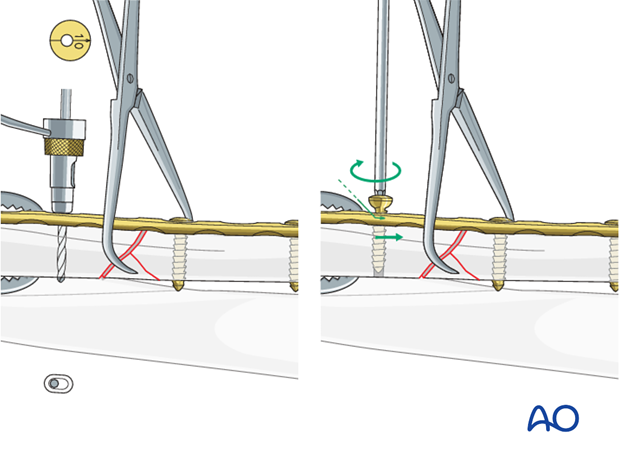
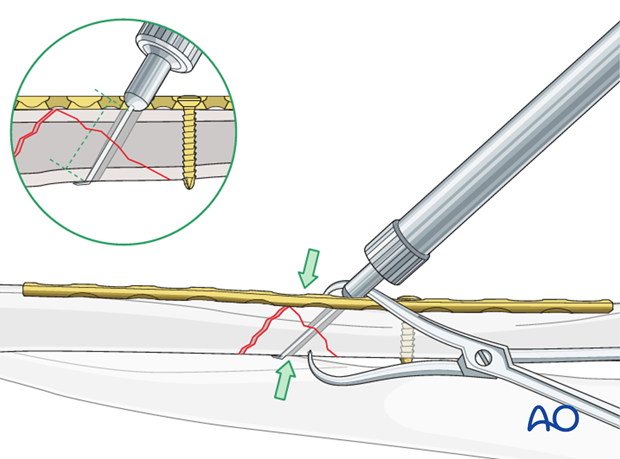
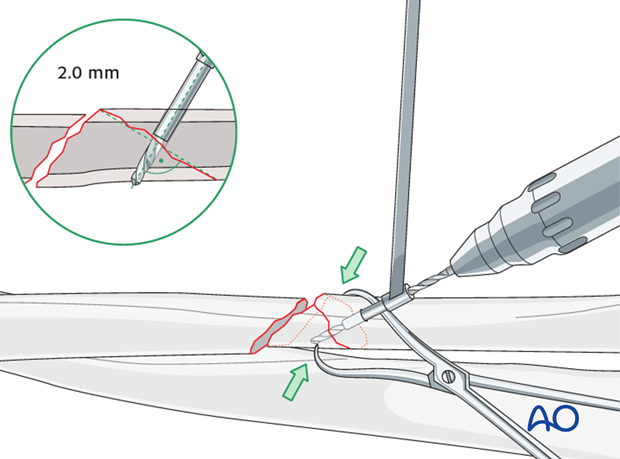
Drill gliding hole
Using a 2.7 mm drill sleeve and a 2.7 mm drill bit, drill a gliding hole in the near cortex of the main fragment.
Ensure that the direction of the drill is as perpendicular to the fracture plane as possible. Bear in mind that the dissection must not strip soft tissue from the wedge fragment.
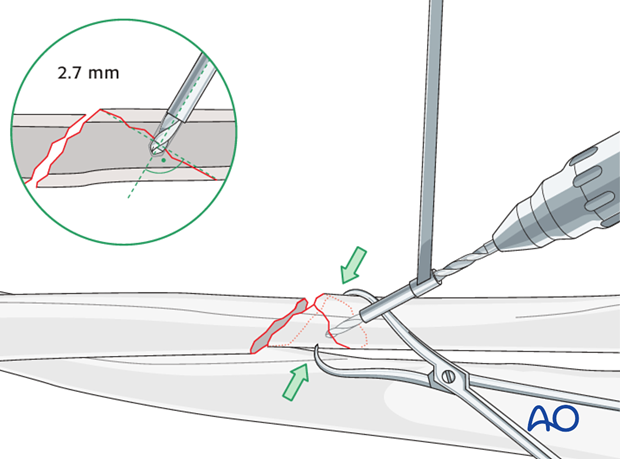
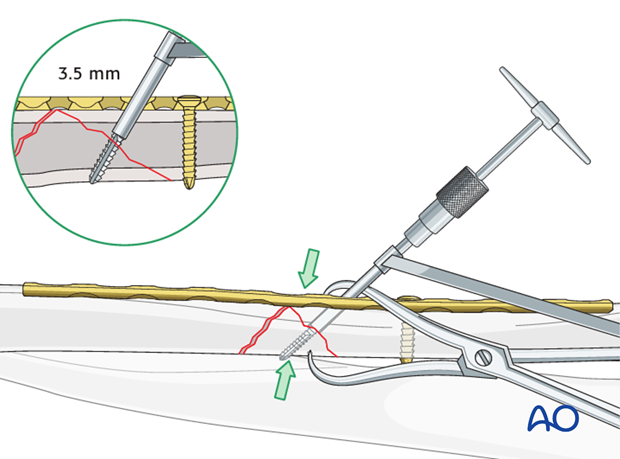
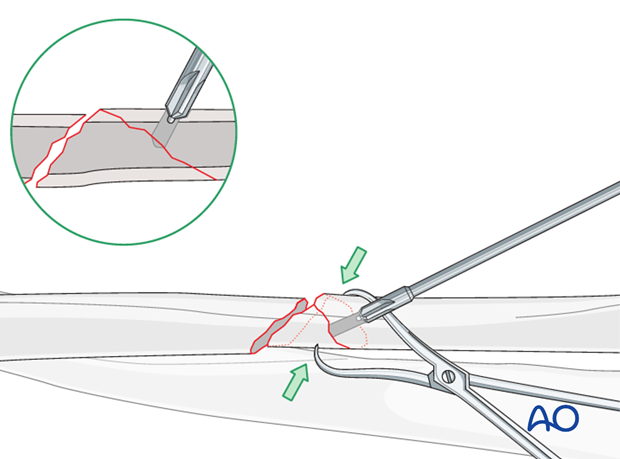
Thread hole: guide in gliding hole
Insert the sleeve of the 2.7 mm / 2.0 mm drill guide into the gliding hole until in gentle contact with the opposite wedge cortex. Check that the anatomical reduction of the wedge is maintained and use a 2.0 mm drill bit to drill a pilot hole just through the far cortex of the wedge.
Countersinking
To spread the load of the screw head on the underlying cortex, the cortex is lightly countersunk, taking care not to overdeepen, which could weaken the cortex.
Measure for screw length
Use a depth gauge to measure for screw length.
Measure the longer side of an oblique drill hole, as shown, to ensure sufficient screw length.
A screw should protrude 1-2 mm through the opposite cortex to ensure maximal thread purchase. However, too long a screw may be tender, or injure soft tissues.

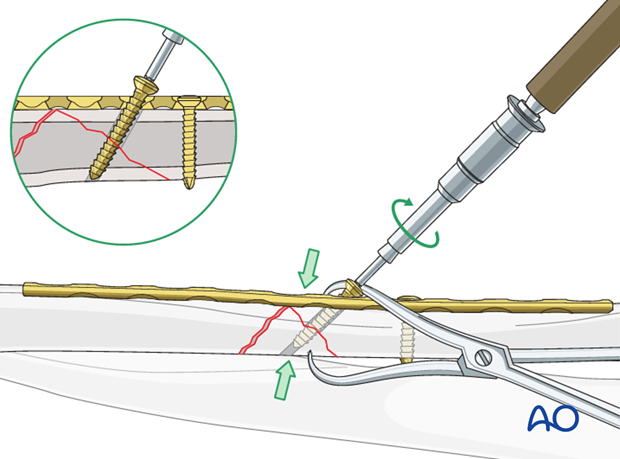
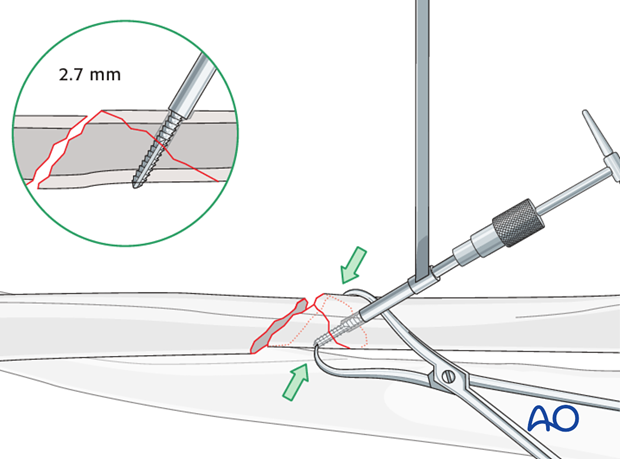
Tap the thread hole
Using a 2.7 mm cortical tap with the corresponding drill sleeve to protect adjacent soft tissues, create a thread in the pilot hole of the far cortex.
This maneuver is not necessary when using self-tapping screws.
Lag screw insertion
Insert the lag screw and carefully tighten it, making sure that the fracture stays reduced, and is compressed.
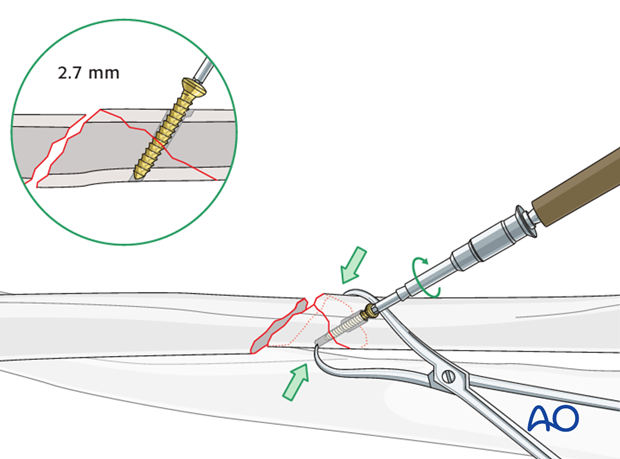
Plate application
The plate should be anatomically contoured to the reduced bone surface but with the addition of a slight prebend.
After fixing the plate with a neutral screw to the fragment bearing the wedge, the first screw in the other main fragment is inserted eccentrically. As this load screw is tightened, take great care not to over-compress. The purpose of this axial compression is to close the fracture gap without producing excessive interfragmentary compression, for fear that the wedge fragment could be split.
The remaining screws are then inserted in neutral positions.
The plate is fixed to the bone using a total of three 3.5 mm bicortical cortex screws in each main fragment.

8. Check of osteosynthesis
Check the completed osteosynthesis by image intensification. Make sure that the plate is at a proper location, the screws are of appropriate length and a desired reduction was achieved.
The elbow should be stabilized at the epicondyles and the forearm rotation should be checked between the radial and ulnar styloids.
9. Assessment of Distal Radioulnar Joint (DRUJ)
Before starting the operation the uninjured side should be tested as a reference for the injured side.
After fixation, the distal radioulnar joint should be assessed for forearm rotation, as well as for stability. The forearm should be rotated completely to make certain there is no anatomical block.
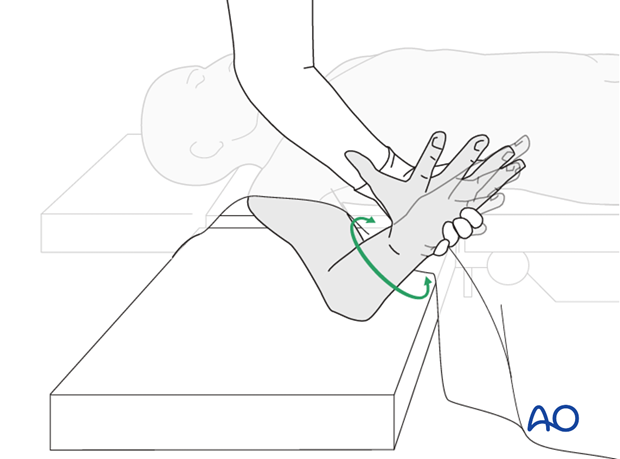
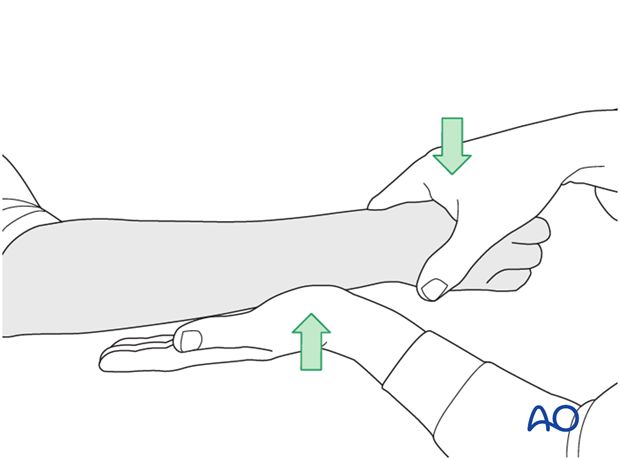
Method 1
The elbow is flexed 90° on the arm table and displacement in dorsal palmar direction is tested in a neutral rotation of the forearm with the wrist in neutral position.
This is repeated with the wrist in radial deviation, which stabilizes the DRUJ, if the ulnar collateral complex (TFCC) is not disrupted.
This is repeated with the wrist in full supination and full pronation.
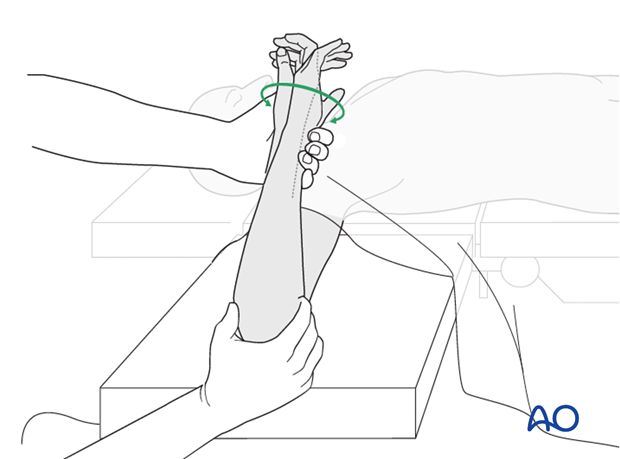
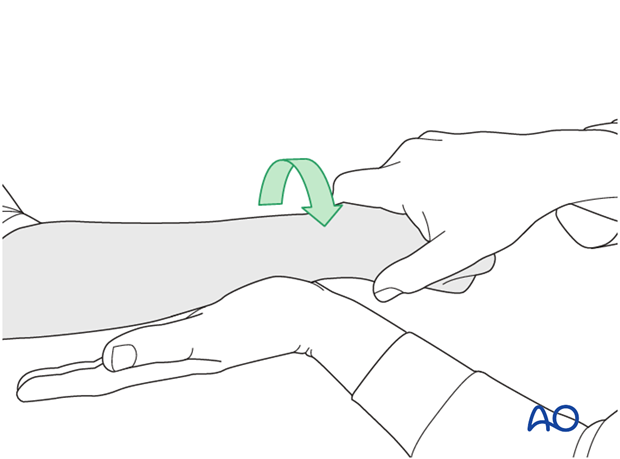
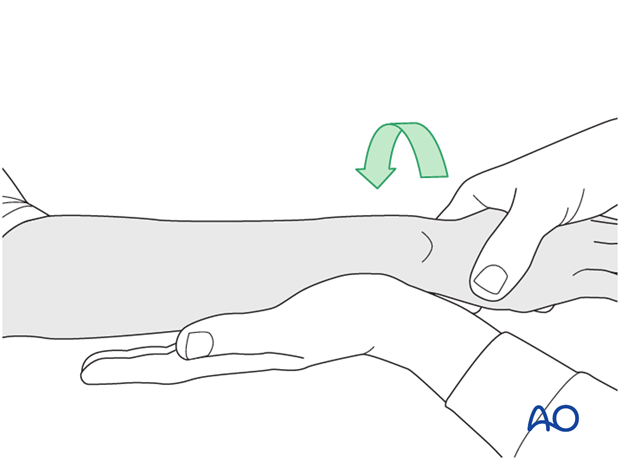
Method 2
In order to test the stability of the distal radioulnar joint, the ulna is compressed against the radius...
...while the forearm is passively put through full supination...
...and pronation.
If there is a palpable “clunk”, then instability of the distal radioulnar joint should be considered. This would be an indication for internal fixation of an ulnar styloid fracture at its base. If the fracture is at the tip of the ulnar styloid consider TFCC stabilization.
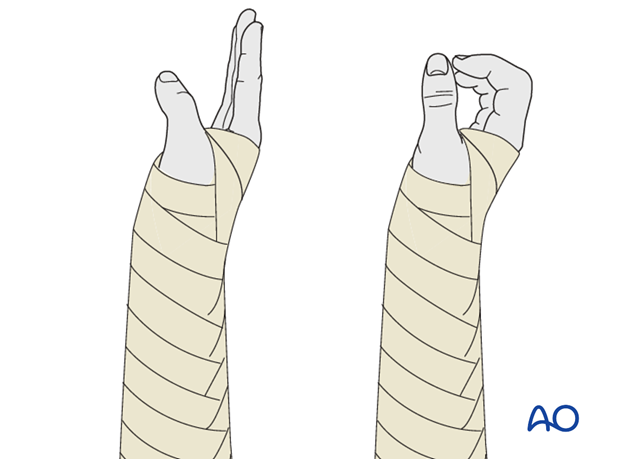
10. Postoperative treatment of a fracture treated with plating
Functional aftercare
Following stable fixation, postoperative treatment is usually functional.
Immobilization in a circular cast may compromise the range of motion later. Temporary immobilization with a well-padded, bulky splint for 10-14 days is advised to allow adequate soft-tissue healing. During this period, elevation, gentle finger motion, active and passive, together with elbow flexion/extension and shoulder motion, can be started. The splint is then removed and active assisted range of motion exercises, including gentle forearm rotation, begin.
Lifting and resisted exercises are restricted until radiographic signs of healing appear. More intensive exercises, such as progressive resisted exercises can start thereafter. Timing of return to sport will depend on the individual patient and the nature of the sport.
Follow-up
Close postoperative follow-up is required in fractures that have been treated by means of absolute stability. Direct bone healing without callus formation is anticipated and early signs of instability with the presence of irritation callus should alert the surgeon to consider secondary interventions, such as restabilization and bone grafting.
Follow-up x-rays should be obtained according to local protocol. X-rays to assess fracture position are usually taken at 1, 2, and 4 weeks after operation. Subsequent x-rays are usually taken to assess bony healing at appropriate intervals from 6-8 weeks, depending on the fracture configuration and potential for healing.
Implant removal
In forearm shaft fractures, the issue of implant removal is controversial. As the radius and ulna are not weightbearing bones, and as removal of plates can be a demanding procedure, implant removal is not indicated as a routine. There is a high risk of nerve damage associated with procedures to remove forearm plates.
Furthermore, as there is significant risk of refracture, most surgeons prefer not to remove plates from the forearm.
The general guidelines today are:
- removal only in symptomatic patients, possibly only on the ulna where the implants are subcutaneous
- removal no earlier than 2 years after osteosynthesis
- If both bones have been plated, sequential removal of implants with a least 6 months in between is recommended (risk of refracture).
References
- Bednar DA, Grandwilewski W (1992) Complications of forearm-plate removal. Can J Surg; 35(4):428-431.
- Langkamer VG, Ackroyd CE (1990) Removal of forearm plates. A review of the complications. J Bone Joint Surg Br; 72(4):601-604.
- Rosson JW, Shearer JR (1991) Refracture after the removal of plates from the forearm. An avoidable complication. J Bone Joint Surg; 73(3): 415-417.
- Heim D, Capo JT (2007) Forearm, shaft. Rüedi TP, Buckley RE, Moran CG (eds), AO Principles of Fracture Management, Vol. 2. Stuttgart New York: Thieme-Verlag, 643-656.













