MIO - Minimally invasive compression plating
1. Indications
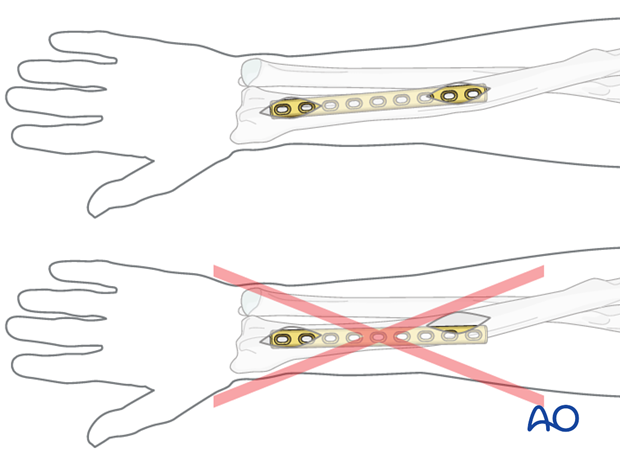
The minimally invasive (sometimes referred to as "limited open") technique is only applicable in the forearm for transverse distal third radial shaft fractures. This technique requires considerable surgical experience. The fractures best suited for this technique are those with dorsal displacement of the distal fragment in the lateral view, with only minimal displacement in the AP view.
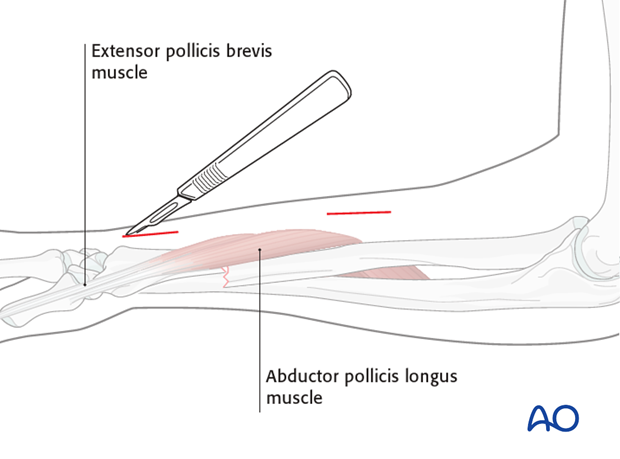
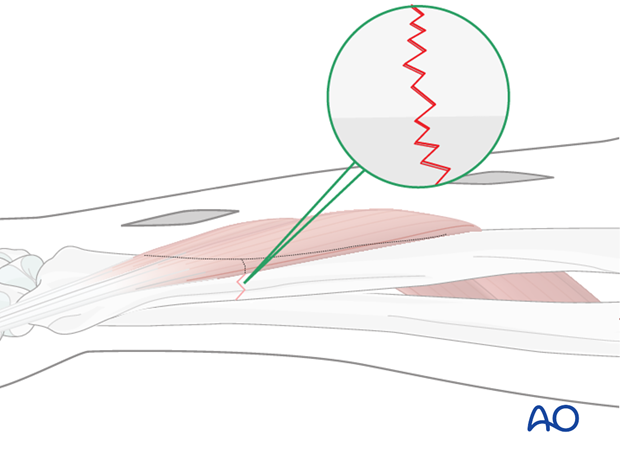
Fractures especially suitable are at the level of the abductor pollicis longus muscle belly.
Oblique distal radial shaft fractures are not suitable because the necessary anatomical reduction and interfragmentary compression are difficult to achieve with this technique.
The advantage of the minimally invasive technique is the preservation of a skin bridge in the region of the abductor pollicis longus muscle.
2. Principles
Compression
Absolute fracture stability, achieved by interfragmentary compression, results in direct bone healing.
Axial compression
Using self-compressing plates (DCP, LC-DCP, LCP, etc.), axial compression results from eccentric screw (load screw) insertion.
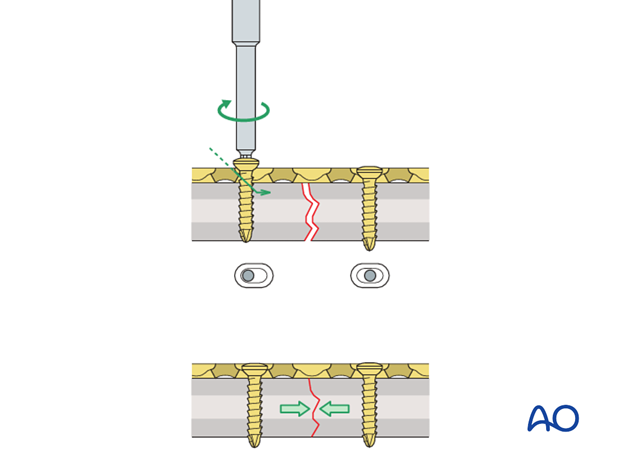
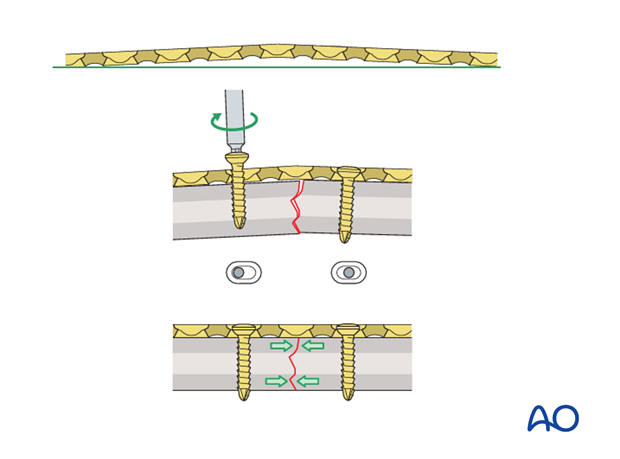
Prebending the plate
If the plate which will exert axial compression is exactly contoured to the anatomically reduced fracture surface, there will be some gapping of the opposite cortex, when the plate is tensioned by tightening the load screw.
The solution to this problem is to “over-bend” the plate so that its centre stands off 1-2 mm from the anatomically reduced fracture surface.
When the neutral side of the plate is applied to the bone, slight gapping of the cortex will occur directly underneath the plate.
As the load screw is tightened, the tension generated in the plate compresses the fracture evenly across the full diameter of the bone.
3. Perioperative planning
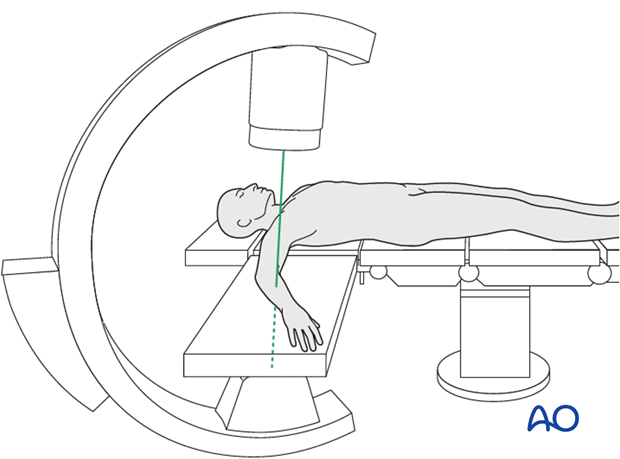
Throughout this procedure, use of image intensification is essential.
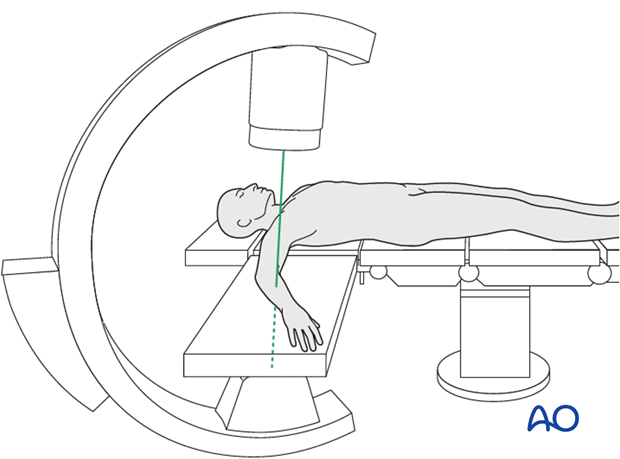
Plate length
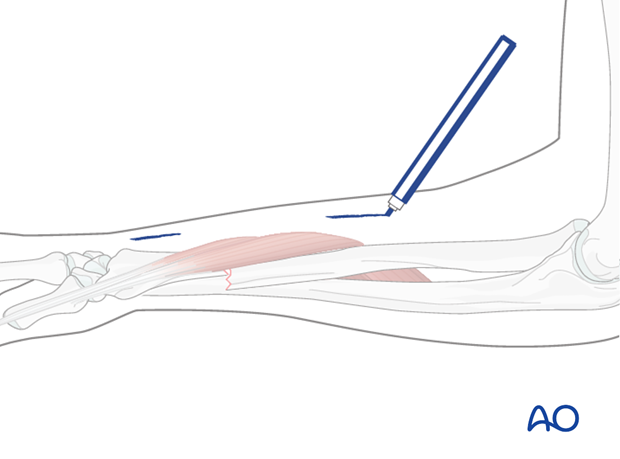
Determine the required plate length (two to three screws on the distal fragment).
Determine the exact location of the incisions and mark them on the skin. Additional marking of the fracture location can be helpful.
4. Patient preparation and approach
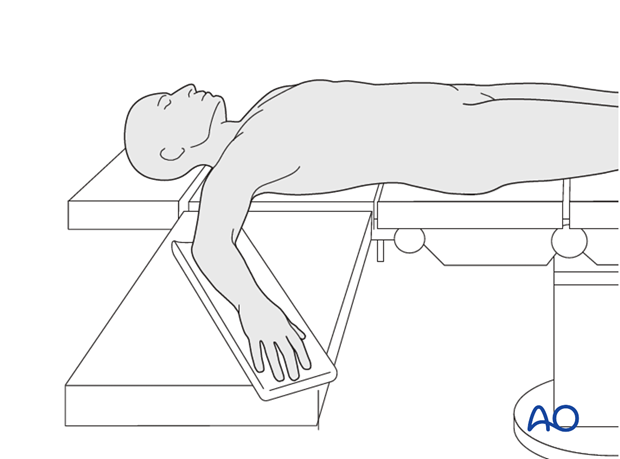
Patient preparation
This procedure is normally performed with the patient in a supine position.
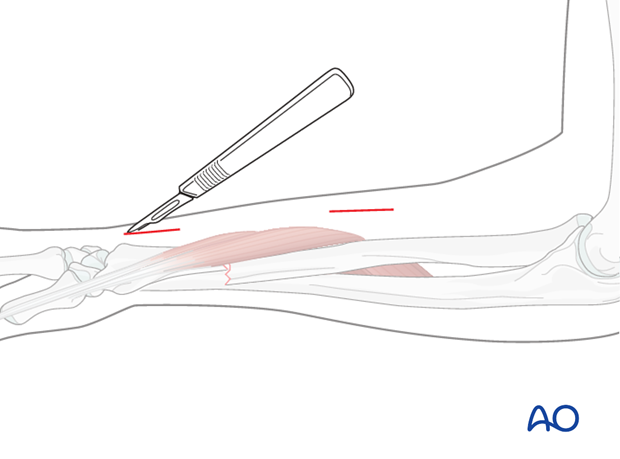
Approach
Parts of a posterolateral (Thompson) approach are used. Additional screws may be inserted through stab incisions (consult the additional material on safe zones).
5. Reduction
Anatomical surgical reduction
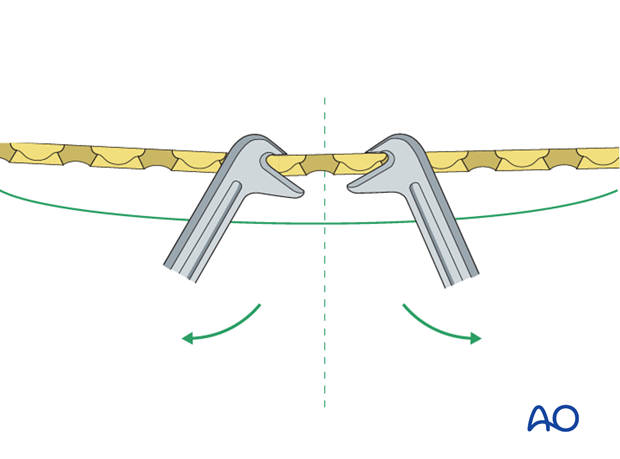
Reduce the fracture anatomically, using a reduction forceps on each main fragment. The use of a blunt, as opposed to pointed, reduction forceps can exceptionally be helpful, if additional manipulative force is required to achieve reduction.
If closed reduction is not possible, open reduction and fixation should be performed as for other transverse radial shaft fractures.
Pearl: leverage technique for transverse fractures
A small bone lever can be used…
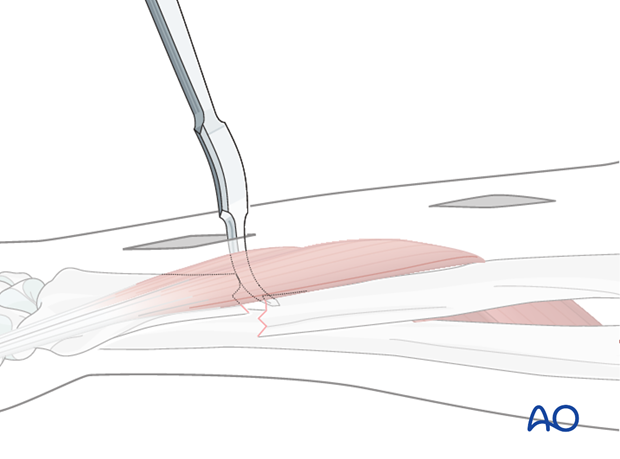
…to reposition transverse fractures…
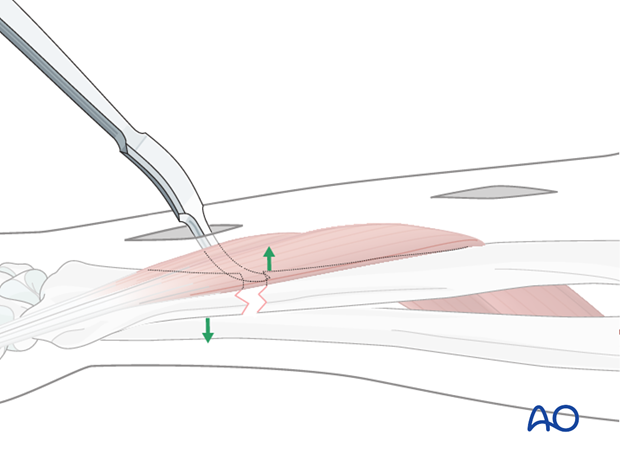
…and achieve anatomical reduction.
Maintain fracture reduction
A reduced transverse fracture can not be maintained with reduction forceps alone. However, transverse fractures are usually dentate and are intrinsically stable after anatomical reduction.
6. Plate contouring
The slight bow of the distal radial shaft has to be respected in the contouring of the plate. Nevertheless, the prebending principle still applies and the adapted plate should still stand off the surface of the reduced fracture by about 1 mm.
7. Fixation
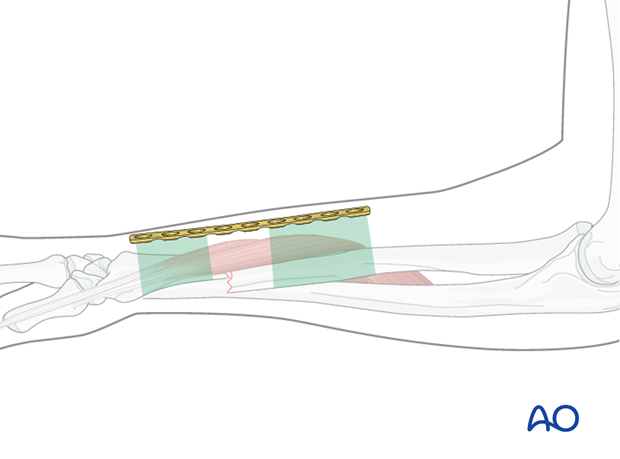
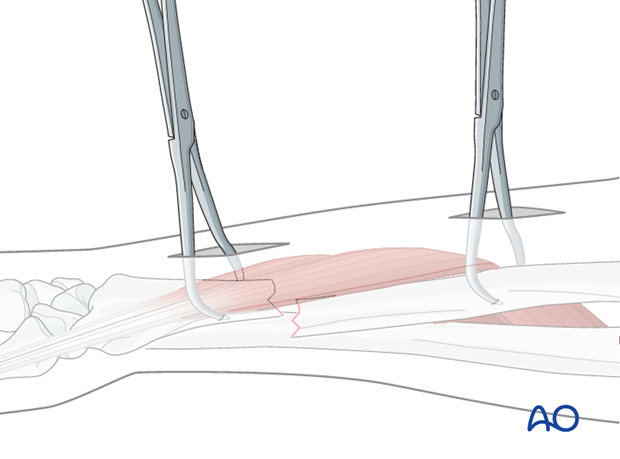
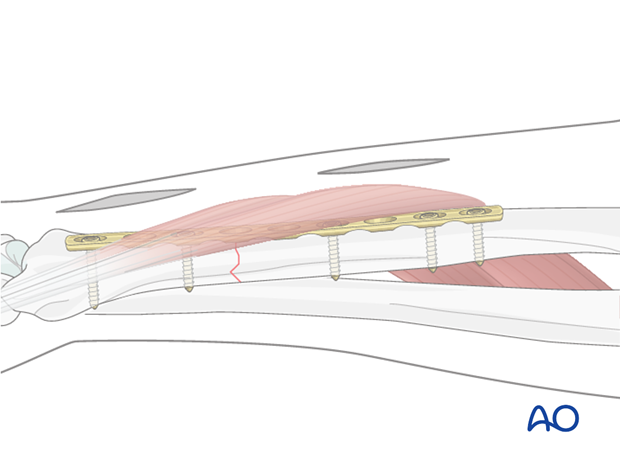
Plate insertion
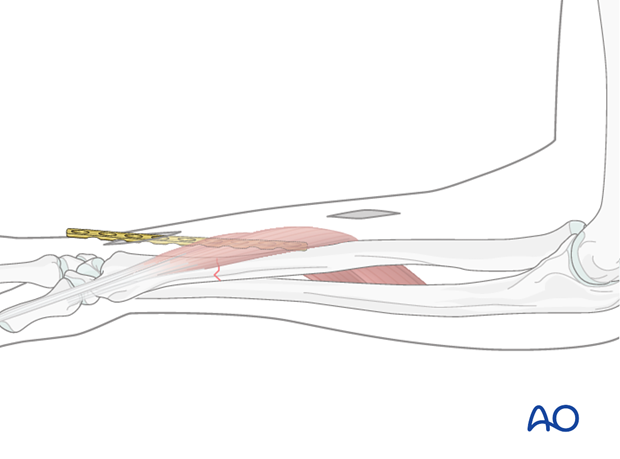
Insert the plate from distal to proximal underneath the abductor pollicis longus muscle. Plate insertion can usually be done by hand.
Pearl: use of a right-angled retractor
Use a small right-angled retractor to lift the abductor pollicis longus while inserting the plate.
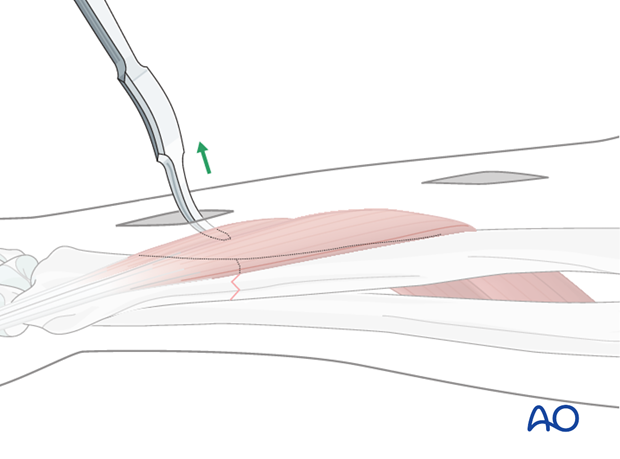
Check proper plate location
Check the correct plate position visually through both incisions. The plate has to be perfectly aligned to the bone.
Insert 1st screw
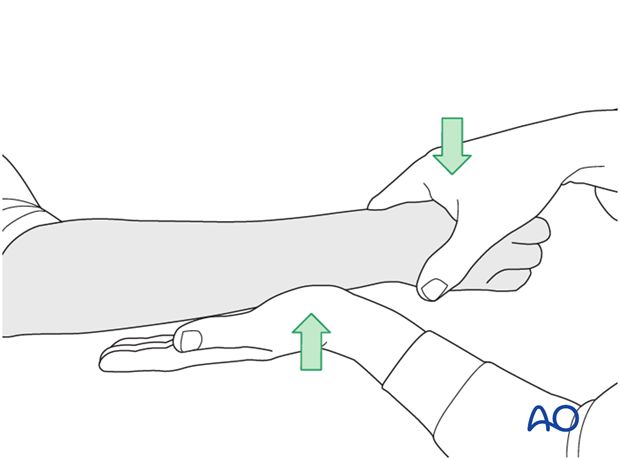
The prebent plate is fixed with a screw in a neutral position to one of the main fragments. A reduction forceps is placed carefully around the opposite fragment to hold it in the reduced position against the plate.
Note: Because of the design of the LC-DCP holes, the neutral drill guides for the LC-DCP have a very slightly eccentric hole and an arrow, which needs always to point towards the fracture line.
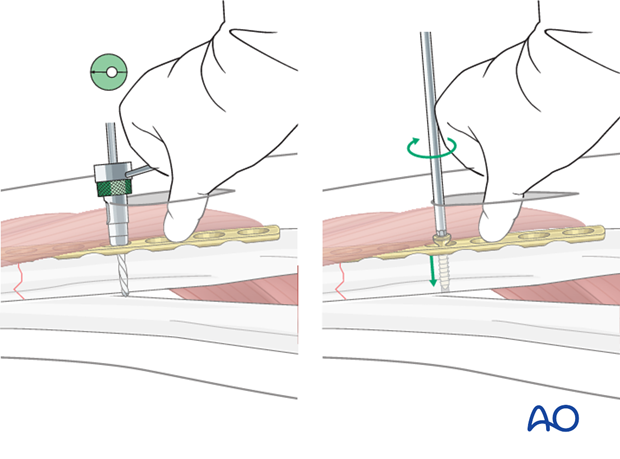
Insert 2nd screw eccentrically
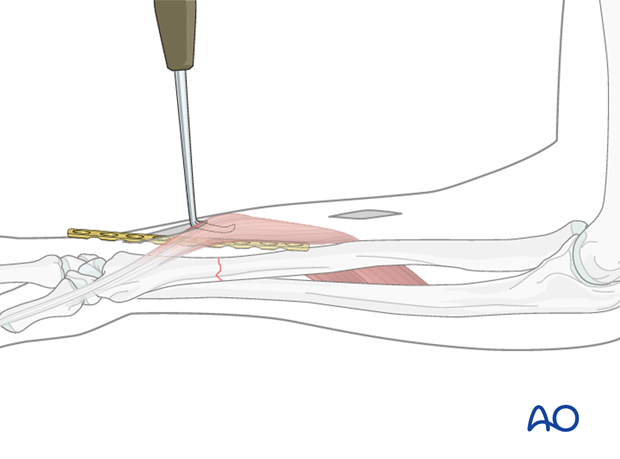
A second screw is inserted eccentrically (yellow drill sleeve) into the other main fragment, gently retracting the abductor pollicis longus muscle aside, as necessary.
Note: the arrow on the drill sleeve has to point towards the fracture line.
If necessary, the distal end of the plate can be held against the bone surface using a finger or a “pusher”. This may require a small separate stab incision.
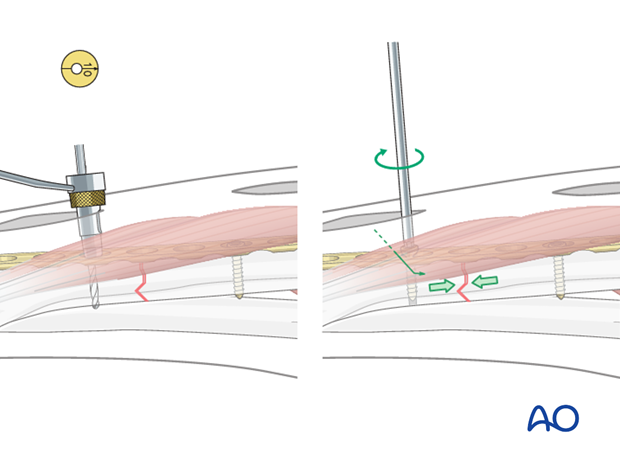
Tighten screw
By tightening the eccentrically inserted screw, axial compression is achieved.
Check preliminary fixation
Check reduction, plate position and fracture compression using image intensification.
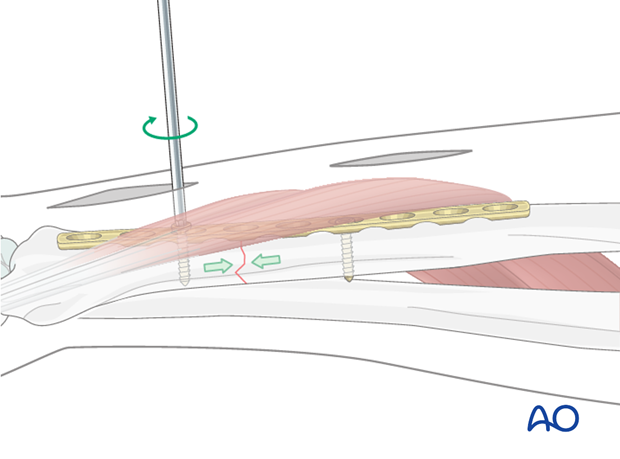
Remaining screws
All the other planned screws are inserted in neutral mode (green drill sleeve) and do not serve to increase compression.
Depending on the exact location of the incisions and the length of plate chosen, an additional proximal stab incision might be necessary. If inserting additional screws through such stab incisions, the soft-tissue structures must be protected by using small retractors.
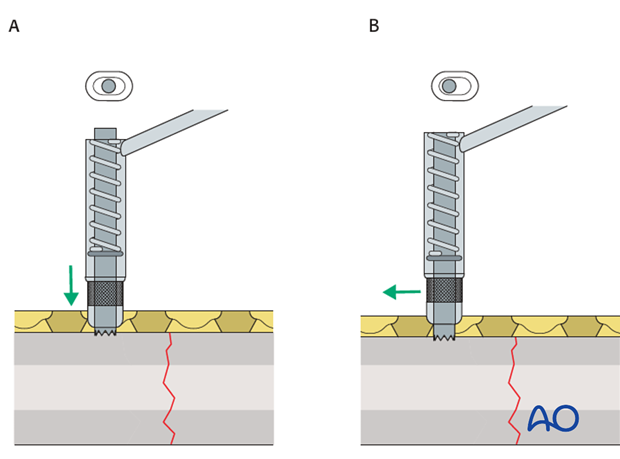
Pearl: alternative drill sleeve
For inserting screws into the limited contact dynamic compression plate (LC-DCP), the Universal Drill Guide can be used as well. When this drill guide is pressed into the plate hole, the screw position will be neutral (A). When it is held against the end of the plate hole, without exerting downward pressure, the screw position will be eccentric (B).
8. Check of osteosynthesis
Check the completed osteosynthesis by image intensification. Make sure that the plate is at a proper location, the screws are of appropriate length and a desired reduction was achieved.
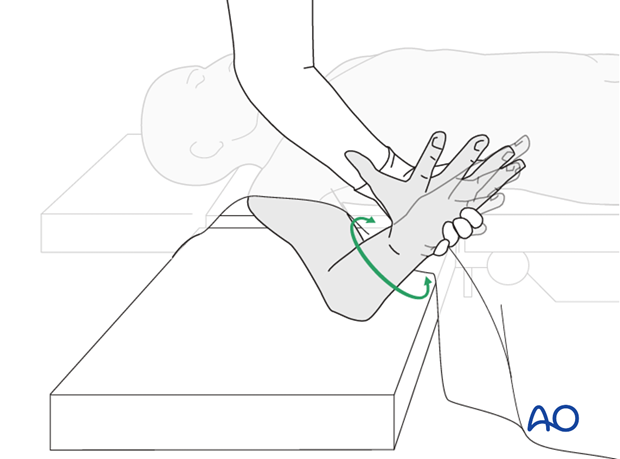
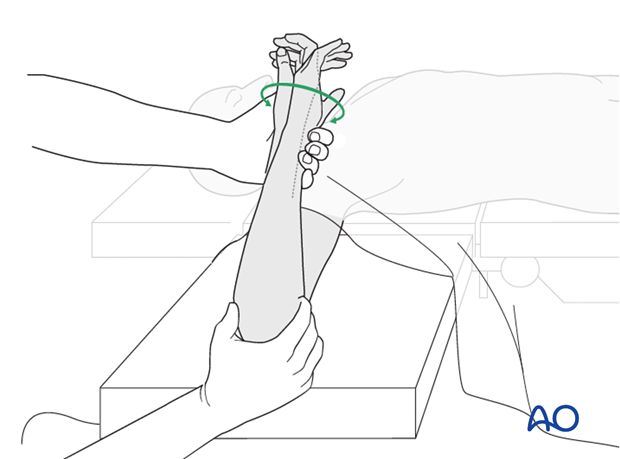
The elbow should be stabilized at the epicondyles and the forearm rotation should be checked between the radial and ulnar styloids.
9. Assessment of Distal Radioulnar Joint (DRUJ)
Before starting the operation the uninjured side should be tested as a reference for the injured side.
After fixation, the distal radioulnar joint should be assessed for forearm rotation, as well as for stability. The forearm should be rotated completely to make certain there is no anatomical block.
Method 1
The elbow is flexed 90° on the arm table and displacement in dorsal palmar direction is tested in a neutral rotation of the forearm with the wrist in neutral position.
This is repeated with the wrist in radial deviation, which stabilizes the DRUJ, if the ulnar collateral complex (TFCC) is not disrupted.
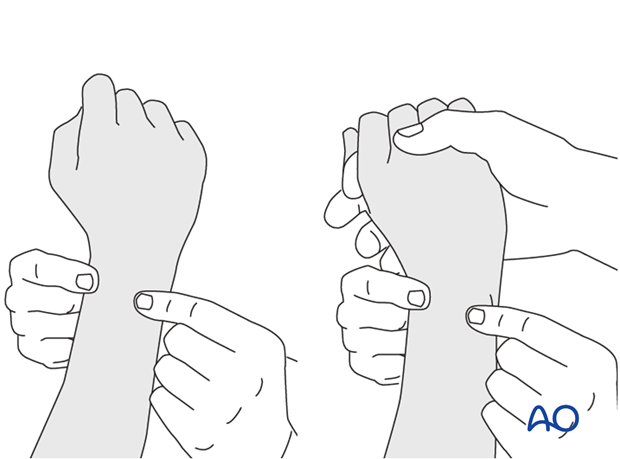
This is repeated with the wrist in full supination and full pronation.
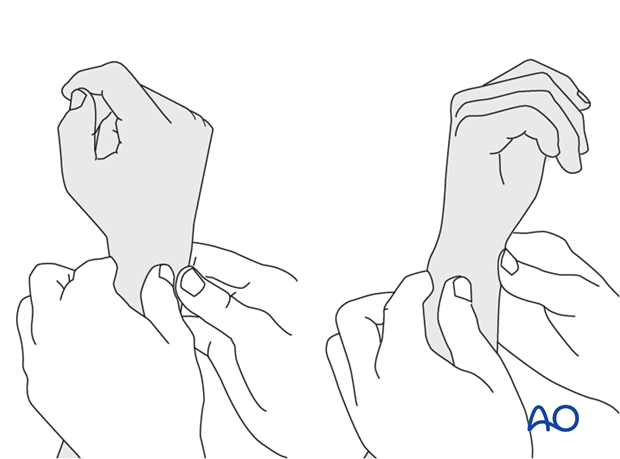
Method 2
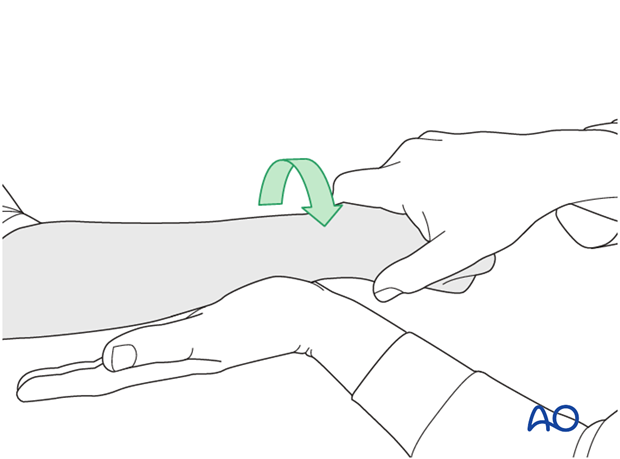
In order to test the stability of the distal radioulnar joint, the ulna is compressed against the radius...
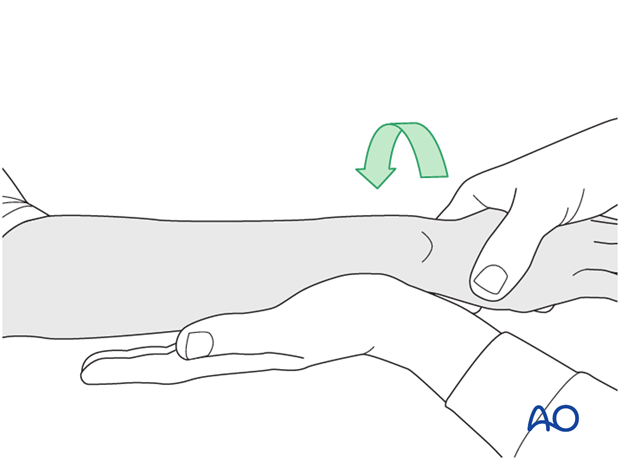
...while the forearm is passively put through full supination...
...and pronation.
If there is a palpable “clunk”, then instability of the distal radioulnar joint should be considered. This would be an indication for internal fixation of an ulnar styloid fracture at its base. If the fracture is at the tip of the ulnar styloid consider TFCC stabilization.
10. Postoperative treatment of a fracture treated with plating
Functional aftercare
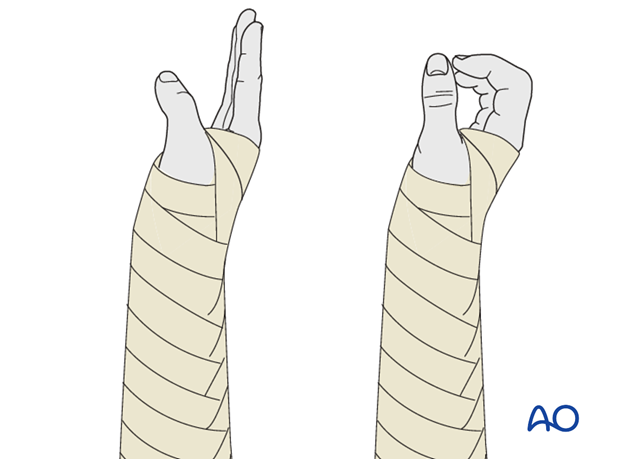
Following stable fixation, postoperative treatment is usually functional.
Immobilization in a circular cast may compromise the range of motion later. Temporary immobilization with a well-padded, bulky splint for 10-14 days is advised to allow adequate soft-tissue healing. During this period, elevation, gentle finger motion, active and passive, together with elbow flexion/extension and shoulder motion, can be started. The splint is then removed and active assisted range of motion exercises, including gentle forearm rotation, begin.
Lifting and resisted exercises are restricted until radiographic signs of healing appear. More intensive exercises, such as progressive resisted exercises can start thereafter. Timing of return to sport will depend on the individual patient and the nature of the sport.
Follow-up
Close postoperative follow-up is required in fractures that have been treated by means of absolute stability. Direct bone healing without callus formation is anticipated and early signs of instability with the presence of irritation callus should alert the surgeon to consider secondary interventions, such as restabilization and bone grafting.
Follow-up x-rays should be obtained according to local protocol. X-rays to assess fracture position are usually taken at 1, 2, and 4 weeks after operation. Subsequent x-rays are usually taken to assess bony healing at appropriate intervals from 6-8 weeks, depending on the fracture configuration and potential for healing.
Implant removal
In forearm shaft fractures, the issue of implant removal is controversial. As the radius and ulna are not weightbearing bones, and as removal of plates can be a demanding procedure, implant removal is not indicated as a routine. There is a high risk of nerve damage associated with procedures to remove forearm plates.
Furthermore, as there is significant risk of refracture, most surgeons prefer not to remove plates from the forearm.
The general guidelines today are:
- removal only in symptomatic patients, possibly only on the ulna where the implants are subcutaneous
- removal no earlier than 2 years after osteosynthesis
- If both bones have been plated, sequential removal of implants with a least 6 months in between is recommended (risk of refracture).
References
- Bednar DA, Grandwilewski W (1992) Complications of forearm-plate removal. Can J Surg; 35(4):428-431.
- Langkamer VG, Ackroyd CE (1990) Removal of forearm plates. A review of the complications. J Bone Joint Surg Br; 72(4):601-604.
- Rosson JW, Shearer JR (1991) Refracture after the removal of plates from the forearm. An avoidable complication. J Bone Joint Surg; 73(3): 415-417.
- Heim D, Capo JT (2007) Forearm, shaft. Rüedi TP, Buckley RE, Moran CG (eds), AO Principles of Fracture Management, Vol. 2. Stuttgart New York: Thieme-Verlag, 643-656.













