Amputation
1. Introduction
Amputations are usually performed due to irreparable soft tissue damage. The lesser digits tolerate amputation better than the hallux.
Amputations are usually performed at the level of the PIP or the MTP joint.
2. Patient preparation
Patient preparation
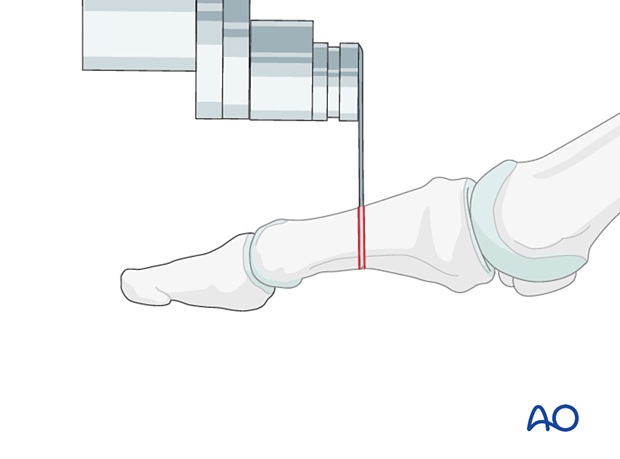
This procedure is typically performed with the patient placed supine and the knee flexed 90°.

3. Amputation
Amputation with extended plantar flap for reconstruction
A tourniquet helps improve visualization.
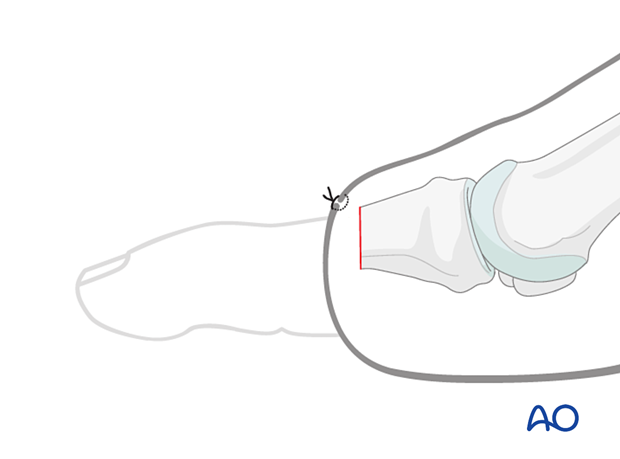
If an extended plantar flap is selected, the surgeon should use more plantar than dorsal skin for the closure.
The length of the plantar flap will need to be at least the diameter of the wound at the level of the amputation.
The digital neurovascular bundle is identified, ligated (cauterized), and transected.
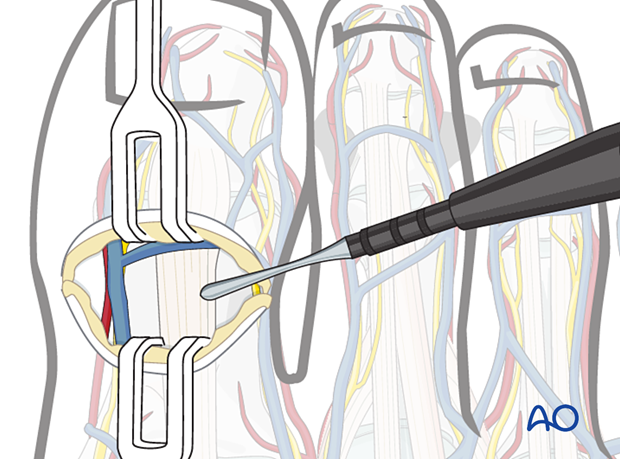
The extensor tendon is transected.
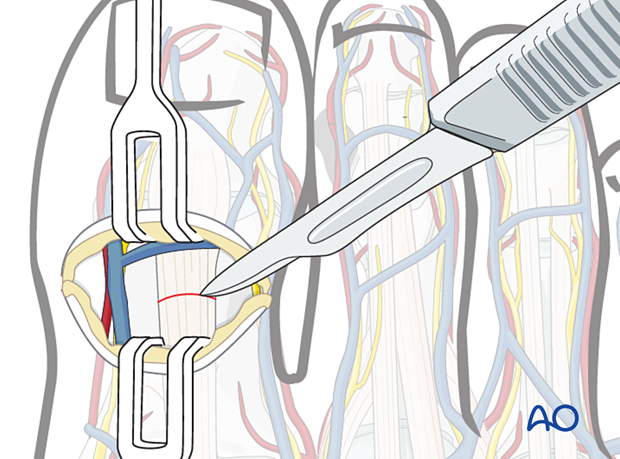
A small oscillating saw is used to amputate through the proximal phalanx.
The plantar plate, flexor tendon(s), and skin are divided, preserving an adequate plantar flap.
The divided flexor tendon is tenodesed to the intact plantar plate or allowed to retract.
Remove the digit.
Irrigate the area and confirm hemostasis.
The wound is closed in layers. Resorbable sutures may be used in the deep dermal tissues, followed by skin sutures.

Technique variation - Guillotine amputation
A tourniquet is helpful to improve visualization.
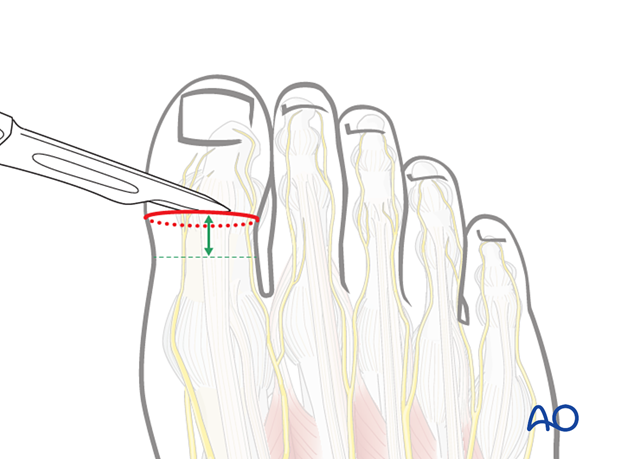
If the surgeon chooses a guillotine amputation, a circumferential skin incision is made distally to the site of disarticulation.
Measure the digit diameter at the level of disarticulation.
A circumferential incision is ideally made at least 0.5 toe-diameter distal to the disarticulation site to ensure sufficient soft tissue for tension-free closure.
Tension-free closure may be difficult to achieve with distal injuries because of the nail or the lack of viable soft tissue. In this case, the nail must be removed before closure, or the amputation will need to be performed at the next proximal joint.
4. Aftercare
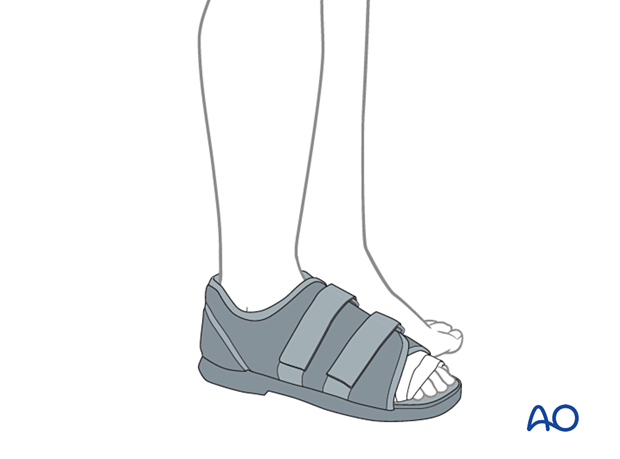
The amputation site must be protected until the soft tissues are healed. We recommend a flat, rigid sole shoe.
The patient may be weight bearing as tolerated.
Sutures are typically removed after 2–3 weeks.