Retrograde nailing
1. General considerations
Reamed versus unreamed nailing
In general, reamed nailing allows the use of larger diameter implants and may therefore provide greater initial stability. Some studies show a tendency towards less malunion and nonunion when reaming is performed. On the other hand, fat embolization is a concern and with the solid unreamed nails, the forces required to achieve nail torsion are higher. Most centers prefer reamed nailing as the standard procedure.
For bone graft while reaming, see Frequently Asked Questions about the Reamer Irrigator Aspirator system.
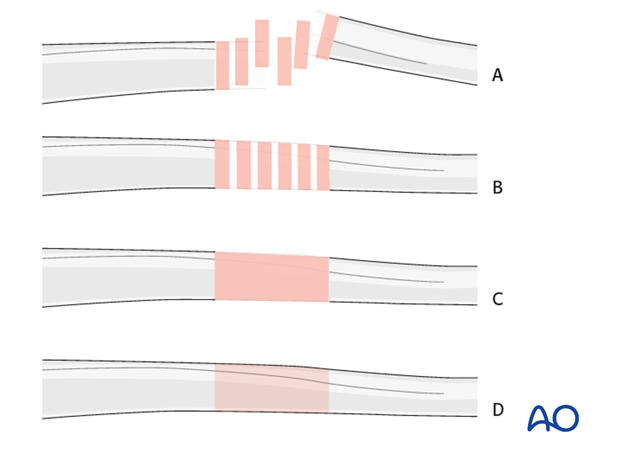
Note on illustrations
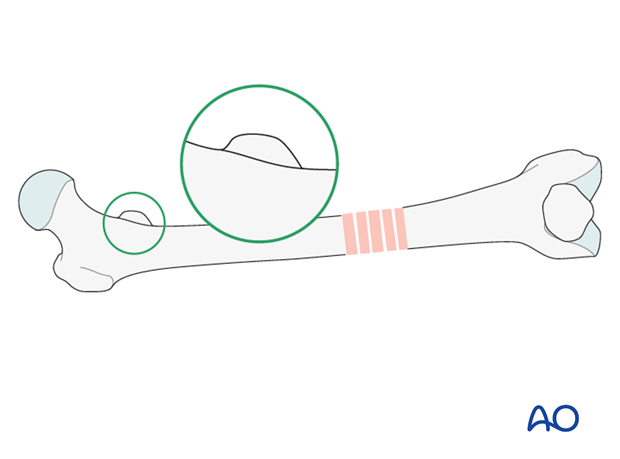
Throughout this treatment option illustrations of generic fracture patterns are shown, as four different types:
A) Unreduced fracture
B) Reduced fracture
C) Fracture reduced and fixed provisionally
D) Fracture fixed definitively
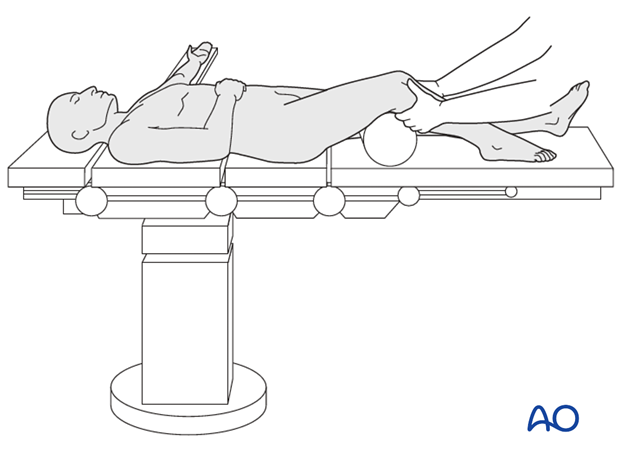
2. Patient preparation
The patient may be placed in one of the following positions:
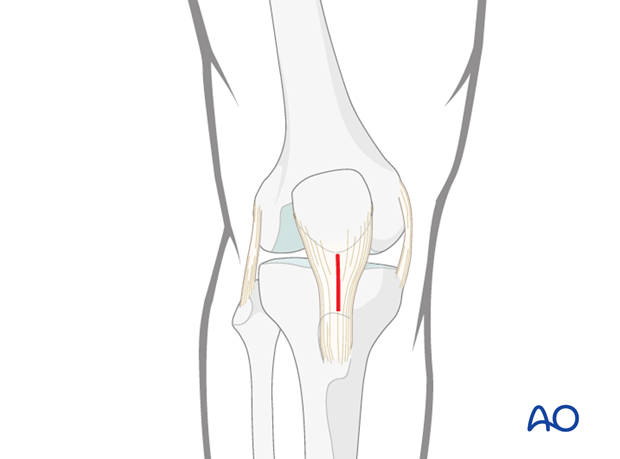
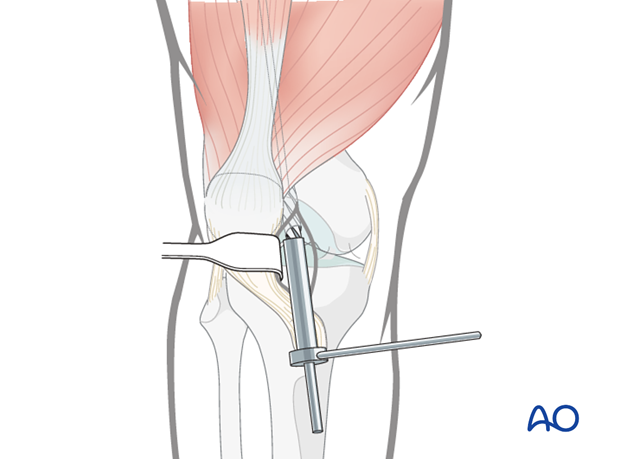
3. Retrograde nailing approach
For this procedure the retrograde nailing approach is used.
4. Reduction and guide-wire insertion
Manual reduction
The fracture reduction may be controlled by pulling traction applied to the upper tibia.
If the distal main fragment does not line up anatomically, one of the following should be considered
- Use of a Schanz screw
- Use of a bone hook
- Insertion of a poller screw (blocking screw)
A Schanz screw inserted into one of the fragments
A monocortical Schanz screw can be helpful for providing direct control of displaced main fragments. It is superior to performing an open reduction with a large skin incision.

Bone hook
Direct reduction with a bone hook may be helpful in securing anatomic alignment. Careful insertion and manipulation must be performed in order to minimize soft-tissue trauma and to prevent injury to the femoral artery.
Reduction using a bone hook with minimal incision is advised.

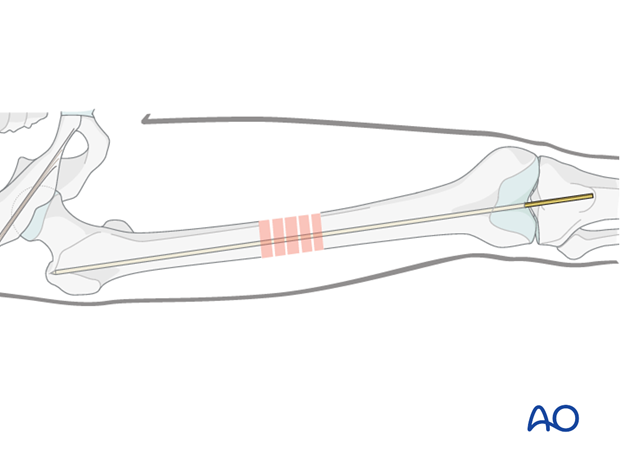
Guide wire insertion
The guide wire is gently slid through the soft tissue into the predrilled entry portal. Advancement into the proximal main fragment is usually easier than in antegrade nailing and is performed under image intensifier guidance.
The guide wire is inserted up to the area of the greater trochanter, where it should have good purchase to prevent its slipping out during reamer exchange.
5. Determine nail length and diameter
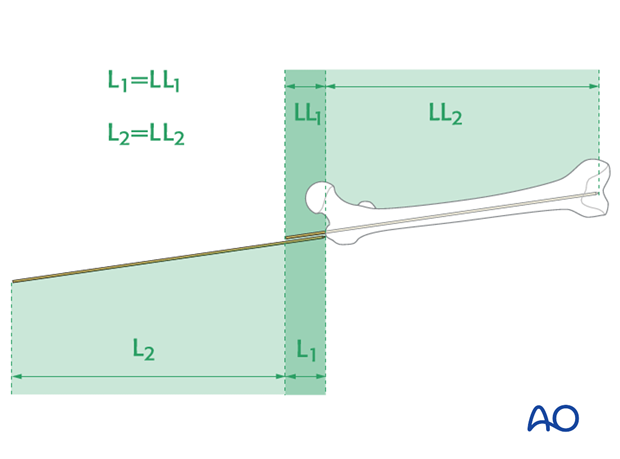
Determine nail length via guide wire
The maximal length of the nail is determined by comparing a second identical length guide wire to the one that has been inserted. The correct placement of the guide wire in the proximal canal should be assessed via image intensifier. Additionally, the second guide wire must be positioned in contact with the articular surface of the distal femur. This must be verified by image intensifier as well.
This will yield the length of nail that would reach to the tip of the greater trochanter – the clinically desirable nail length may be less, depending on the fracture level and morphology.
Alternative: radiographic ruler
Alternatively, a radiographic ruler may be used.
The tip of the ruler should be positioned at the piriformis fossa. The measurement of the nail length should be in the center of the distal end of the femur at the roof of the intercondylar notch.
It is important to visualize the fracture zone by image intensifier to carefully ensure that adequate femoral length has been maintained.
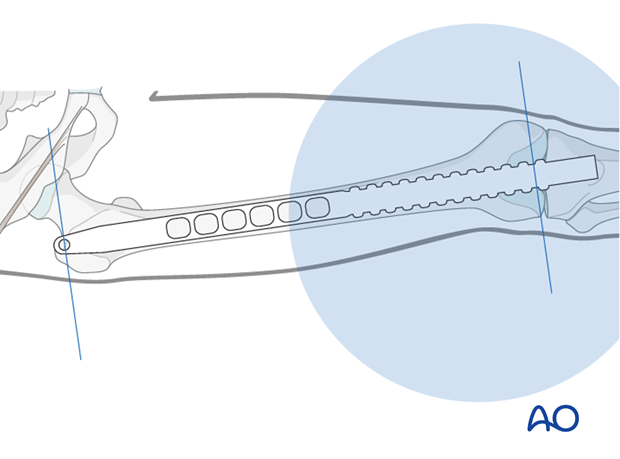
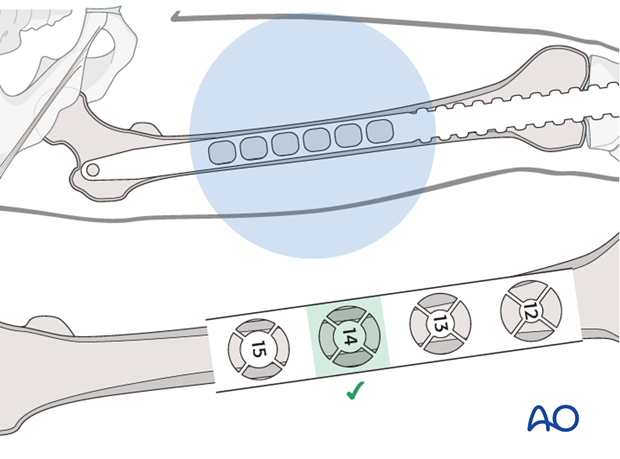
Nail diameter
It is important to measure the medullary diameter at the mid portion of the femur, which represents the narrowest segment of the medullary canal.
The inner cortical edge should touch with the inner numbered disk of the ruler aperture. In the illustration an inner cortical diameter of 14 mm is shown.
Consideration for special situations
In multifragmentary fractures, or in open fractures with bone loss, it is safer to perform preoperative planning on the uninjured leg. In bilateral femoral fractures, the less comminuted side should be used to determine the length and diameter of the nail.
6. Poller screw (blocking screw)
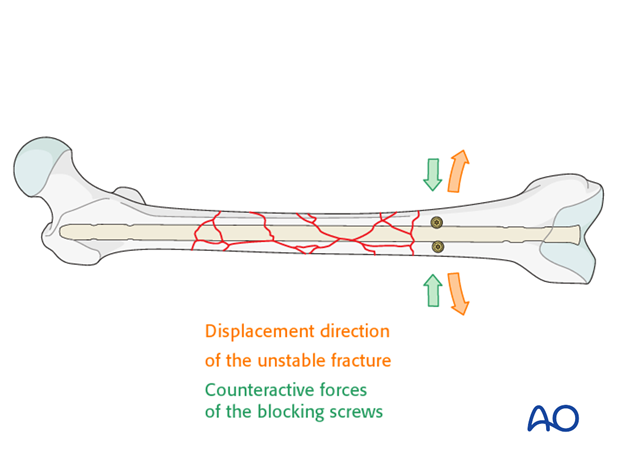
General considerations
The concept of a poller screw is based on the principle that the malalignment induced by oblique, proximal and distal fractures can be counteracted by the nail-directing effect of the screw. Therefore, its position should aim to counteract the displacement of the fracture. Most often it is therefore placed in the short side in the distal fragment. If there is a wide canal, two screws can be placed on either side of the path of the nail.
It is advisable to insert the poller screw prior to reaming, and in case of unreamed nailing, prior to nail insertion, in order to provide adequate contact between the nail and the screw. If the poller screw is inserted after reaming, the path of the nail is already set and the poller screw may not work. A small fracture screw or a locking screw can be used as a poller screw, depending on the local anatomy.
The reaming process in the presence of the poller screw must be performed very carefully in order not to harm the reamer tip.
The most frequent indication for poller screws is a proximal or distal oblique fracture which tends to shift when the axial knee blow technique is used to close any fracture gap, or when the patient is mobilized.
In these cases, prophylactic poller screws are very helpful.
See also:
Stedtfeld HW, Mittlmeier T, Landgraf P et al. The Logic and Clinical Applications of Blocking Screws. J. Bone Joint Surg. Am. 2004; 86-A Suppl 2:17-25.
Midshaft comminuted fractures
Poller screws are used according to the initial displacement and the size of the canal. In general, midshaft fractures tend to align better than more proximal or distal fractures and, therefore, the indication for poller screws is uncommon.
7. Reaming
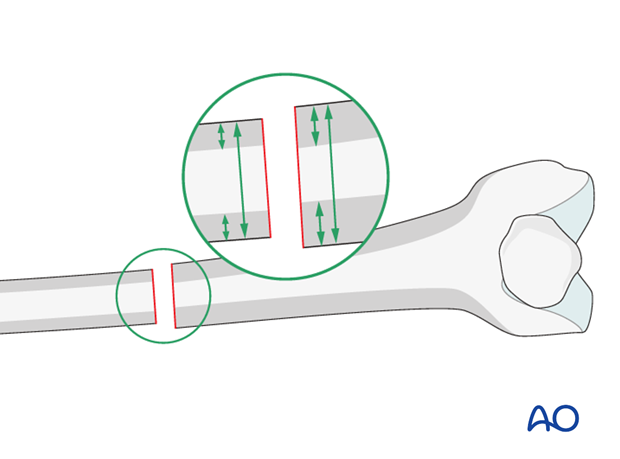
Sequential reamer size increase
After the tissue protector has been introduced, the reamer shaft, fitted with the initial reamer head is inserted over the guide wire. Usually reaming begins with a 9 mm medullary reamer.
The reaming is performed in sequential steps with increments of 0.5 mm each.
As soon as chatter from cancellous bone can be felt and heard, the inner cortex has been reached. This may not be the case in segmental fractures, or when severe comminution is present.
Reaming must be performed one or two increments beyond the planned nail diameter in order to allow a smooth nail insertion. For example, for a nail diameter of 10 mm, drill bits of up to 10.5 or 11 mm diameter are used. If a very tight fit of the reamer can be felt before the desired reaming size is reached, one should consider a smaller diameter nail than previously planned.
Pitfall 1: Eccentric reaming
Eccentric reaming can cause weakening of the adjacent cortex which may interfere with healing or even cause a fatigue fracture.
Pitfall 2: Trapping of reamer by slow spinning
If the reamer becomes trapped while reaming, it must be gently removed by the most senior surgeon, because breakage of the reamer tip in this situation can be a devastating complication.
Pitfall 3: Heat necrosis by overaggressive reaming
Overaggressive reaming should be avoided because it may cause heat necrosis of the femoral canal. This applies especially for narrow midshaft canals (9 mm or less in diameter).
Pitfall 4: Rapid thrusting/systemic fat embolization
Care should be taken to use sharp reamers, to advance the reamers slowly, and to allow sufficient time between reaming steps in order for the intramedullary pressure to normalize. Rapid thrusting of the reamer may worsen the intramedullary pressure increase that is observed during nailing. This image demonstrates fat extrusion in a human cadaver specimen with a window in the proximal section.
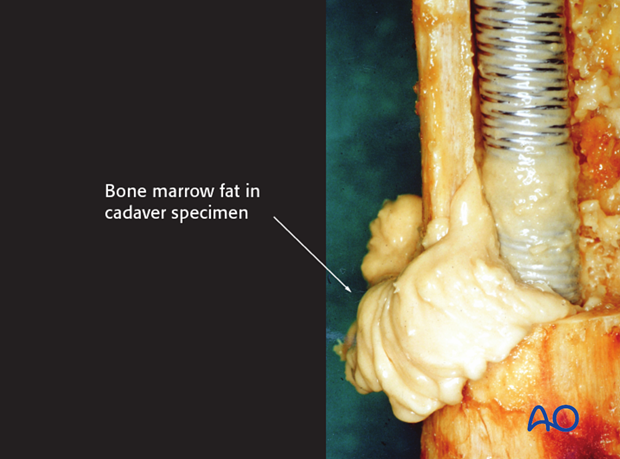
This may cause pulmonary embolization of medullary fat, which in turn may lead to pulmonary dysfunction (lower image in the enlarged view shows an example of fat embolization through the right atrium).

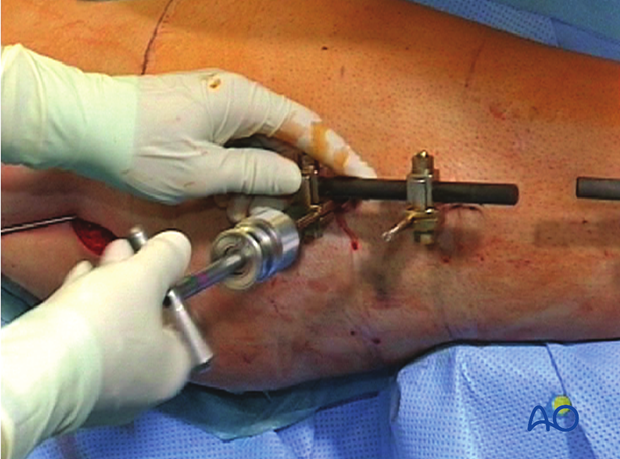
Special situation: conversion from an external fixator to an intramedullary nail
Because the external fixator is still in place, the Schanz screws must be partially withdrawn to allow the guide wire, the reamers, and later the nail, to pass through. The external fixator is held in place by monocortical purchase to assure that the fracture remains stable. The external fixator also acts as a joystick for the reduction.
8. Nail insertion
General considerations
During insertion of the nail, it is important that the assistant applies traction to the lower extremity to prevent shortening and/or angulation of the distal main fragment. In order to prevent this complication, which is very difficult to correct, repeated image intensifier assessments are required.
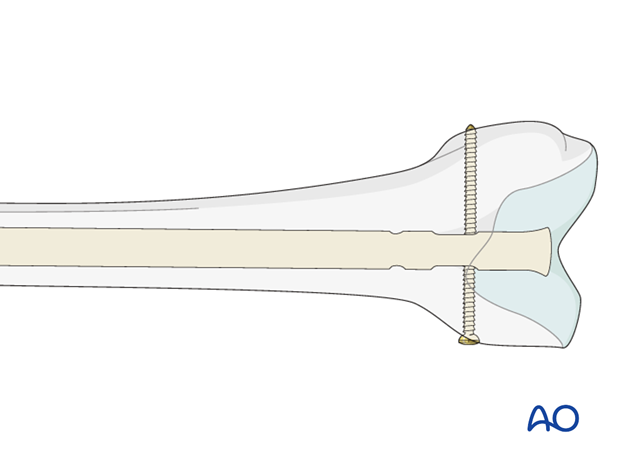
The correct nail placement is important in terms of adequate seating in the distal main fragment. The nail must never be too long and protrude into the knee joint because of the risk of damage to the articular cartilage of the patella. If the nail is sunk more than 2 cm deep to the cortex at the entry point, the placement of the locking screws will be too proximal. Also, it would be difficult remove the hardware, should this be required at a later stage.
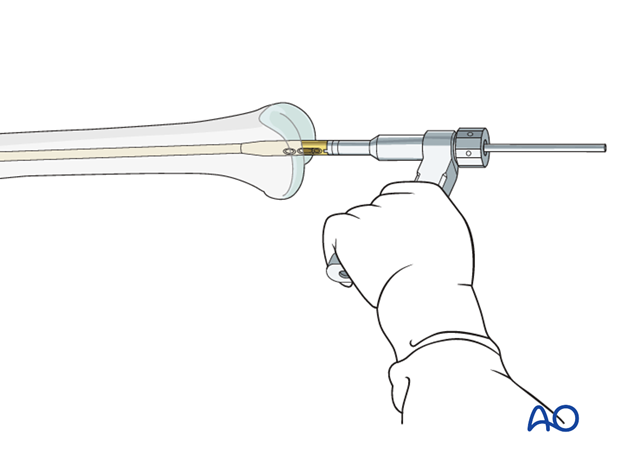
The nail is gently driven into the proximal fragment. This can often be performed manually. If required, gentle hammer taps are usually sufficient to ensure proper advancement.
9. Locking sequence and locking type
Distal locking first
It is important to do the distal locking first. If proximal locking is done first, the surgeon will no longer be able to perform final corrections to length and rotation.
Distal locking is performed by using the aiming device attached to the insertion handle.
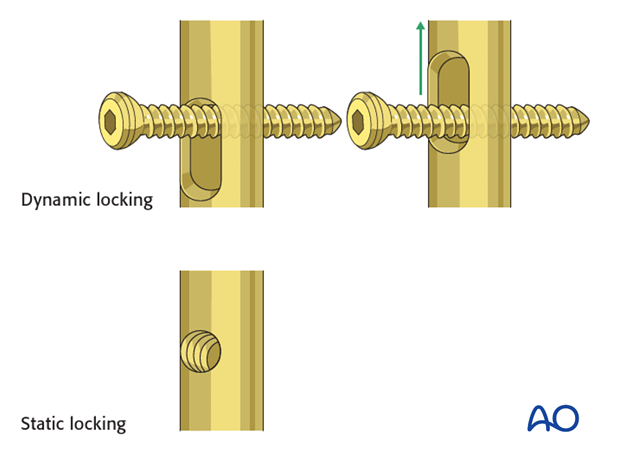
Dynamic or static locking
Simple transverse non-comminuted fractures are stable and fracture healing may be enhanced by dynamic locking. Comminuted fractures require a length stable construct so stable locking is mandatory. Slotted locking holes can be used for dynamic locking while small circular holes are used for static locking.
10. Distal locking
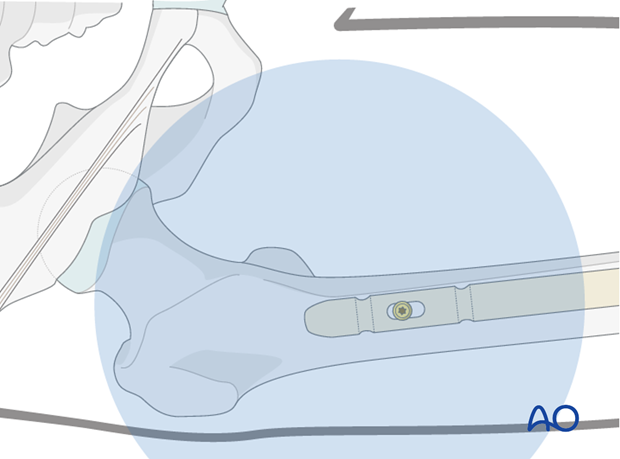
Distal aiming device
After verifying the correct position of the distal end of the nail under the image intensifier, the distal aiming device may be attached to the insertion handle.
For correct measurements through the drill sleeve it must be kept at the bone at all times.
The contralateral thumb can be used to keep the contact.
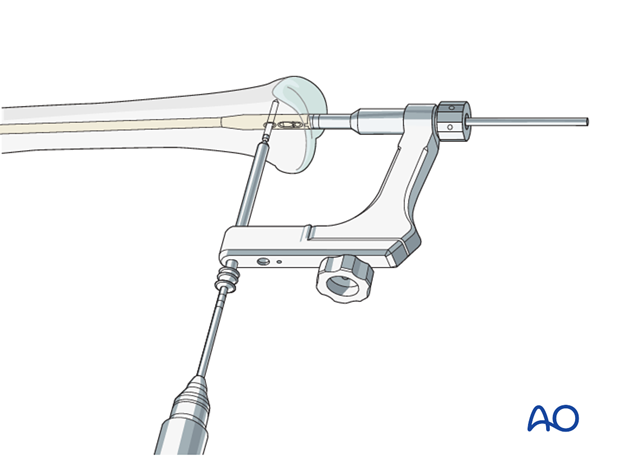
Screw insertion
The sites of the skin and fascial incisions for the drill bit and the distal locking screws may be determined after the drill sleeve assembly has been inserted in the holes of the aiming device. The length of the locking screws is read from the calibrated drill bit. The correct length is confirmed antero-posteriorly under the image intensifier. The insertion handle is now removed.
Drill sleeve to bone contact
The drill sleeve must remain in close contact with the bone at all times since it is important for the measurement of the locking screws. Close contact is maintained by pressing on the sleeve with the contralateral thumb.

Verification of locking screw placement
Final x-rays in two planes should be obtained in all cases in order to check on the exact locking screw placement.
Pitfall: locking screw too long
It is important to remember that the distal femur tapers from the posterior to the anterior. Therefore, if a straight AP view is obtained, the locking screws appear to be inside the bone. If they appear to be outside the bone, they are most likely too long and will invariably cause pain and possibly heterotopic ossification. In order to assess the exact length of the locking screws an AP view can be obtained with 30° internal rotation of the lower extremity and with 20 degrees of external rotation of the lower extremity.
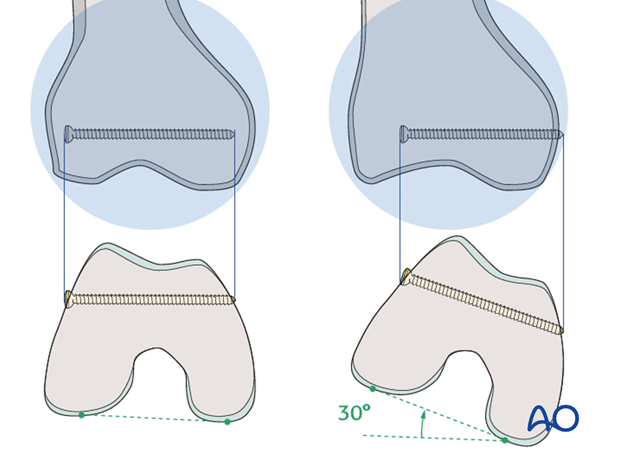
Internal rotation by 30° reveals that the screw length was chosen inappropriately.

11. Intraoperative radiological assessment
Assessment of rotation
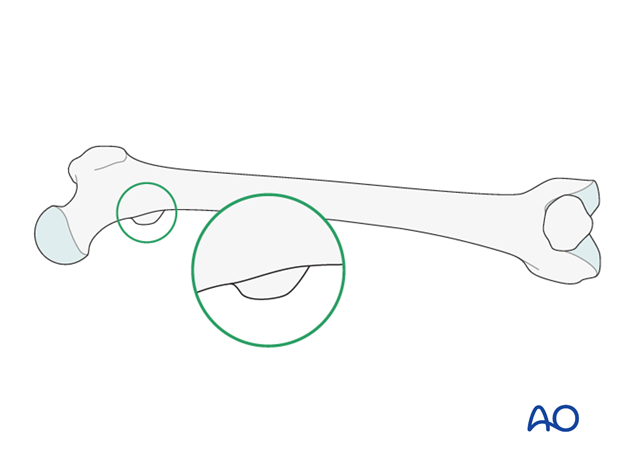
The profile of the lesser trochanter is compared with that of the contralateral leg (lesser trochanter shape sign).
Before positioning the patient, the profile of the lesser trochanter of the intact opposite side (patella facing anterior) is stored in the image intensifier.
The illustration shows the lesser trochanter of the intact opposite side.
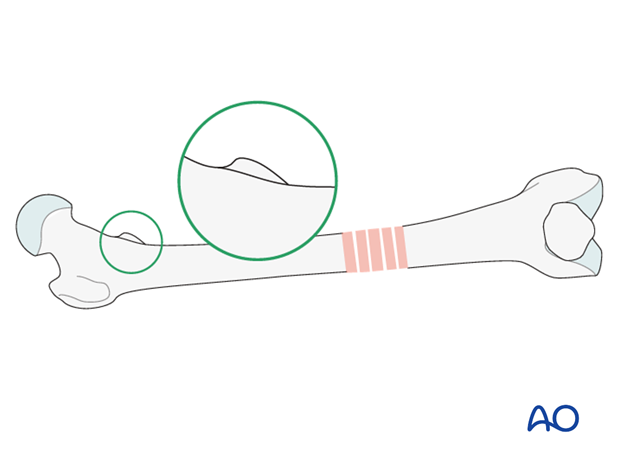
Malrotation
In cases of malrotation, the lesser trochanter is of different profile when compared to that of the contralateral leg.
Care should be taken to assess rotation with the patella facing directly forwards.
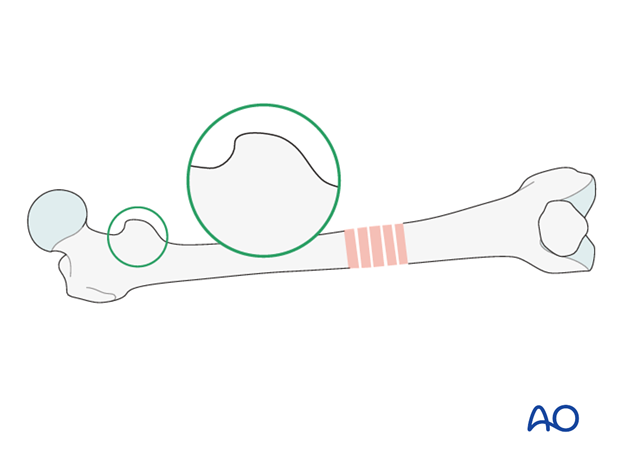
Matching of the lesser trochanter shape
After distal locking, the correction is achieved by using the handle of the nail insertion device. Thereby the distal main fragment can be rotated in relation to the proximal main fragment.
Cortical step sign and diameter difference sign
The presence of considerable rotational deformity may be diagnosed by the difference in thickness of the cortices above and below the fracture zone.
The diameter difference sign is of use at levels where the bone cross section is oval rather than round. In cases of malrotation, the proximal and distal main fragments will appear to be of different diameters.
12. Proximal locking
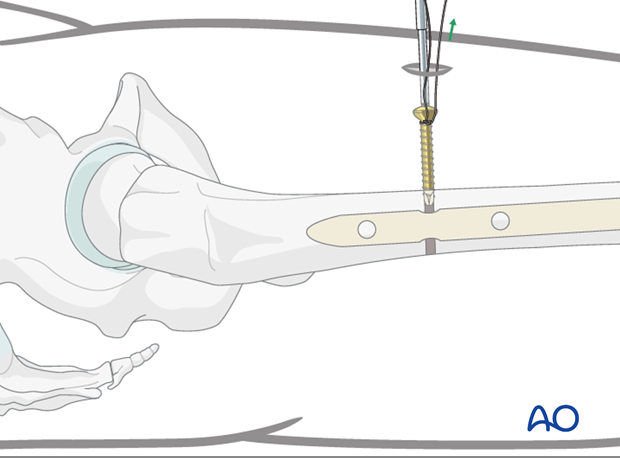
Drilling of screw hole
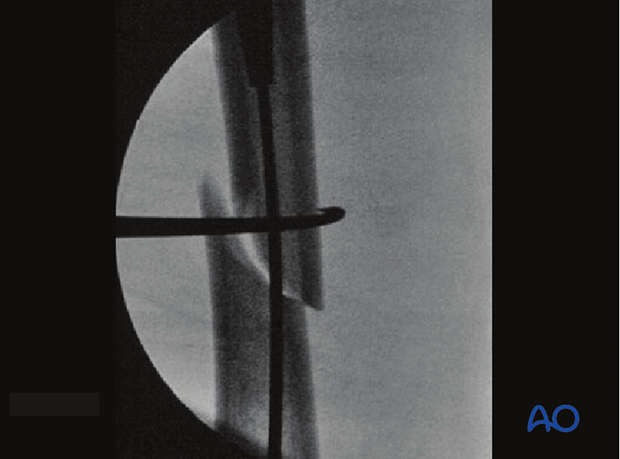
Proximal AP locking has to be performed by the freestyle method. After verifying the correct position of the distal end of the nail under the image intensifier, the proximal locking hole must be visualized by image intensification.
The image intensifier is brought into a strict AP position of 90 degrees. The distal hole must project a perfect circle and the tip of a scalpel is projected into the center of the hole.
This guides the stab incision of the skin. The hole is deepened through the muscle by blunt dissection and the hole is drilled perpendicular to the nail, using the radiolucent drill. This is then followed by measurement with a depth gauge and insertion of the locking screw. Care should be taken to prevent an oblique insertion of a locking screw because it can become trapped between the firm cortical proximal femoral bone and the nail. Depending on the fracture pattern, either one or two proximal locking screws are used.
Maintaining lower extremity position
While the locking hole is drilled, the assisting surgeon must prevent the leg from moving in order not to miss the target hole.
Locking screw insertion technique
The length of the locking screw is determined, using the appropriate depth gauge. Then the locking screw is inserted.
If a radiolucent drive is unavailable, the projection of the tip of the drill bit should be placed as centered as possible (see illustration). Start drilling but assess the position of the tip of the drill bit repeatedly, with the drill temporarily uncoupled.
Pearl: If the contact between the screw driver and the locking screw is lost, the screw may move within the soft tissue and become extremely hard to capture. To prevent this time-consuming complication, the locking screw should be lassoed with a strong absorbable suture.
Second locking screw
The question as to whether a second locking screw should be used must be decided by the surgeon on a case-to-case basis.
13. Insertion of the end cap
Insertion of the end cap: conventional way
An end cap may be used, depending on the final relationship of the nail end to the intercondylar notch of the distal femur.
The distance between the distal end of the nail and the articular surface determines the appropriate length of the end cap, which ranges between zero and 20 mm in 5mm increments. By no means should the end cap be more distal than the subchondral region.
The end cap is introduced in the conventional way, using a hexagonal screwdriver.
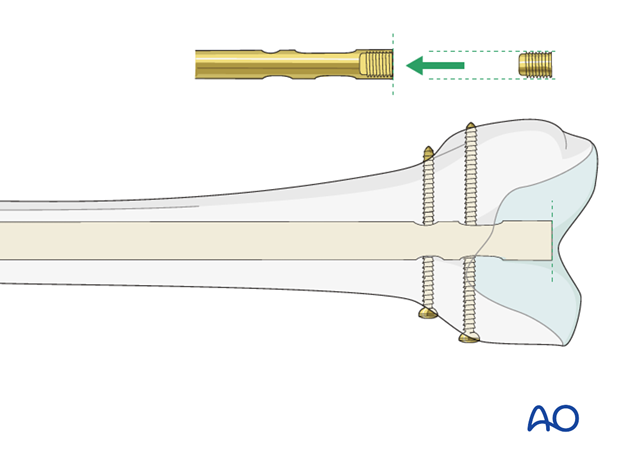
Insertion of the end cap: by guide wire with hook
So as not to lose the end cap, the specifically modified guide wire with hook is used. It fixes the end cap to the screwdriver and assures that they remain connected.
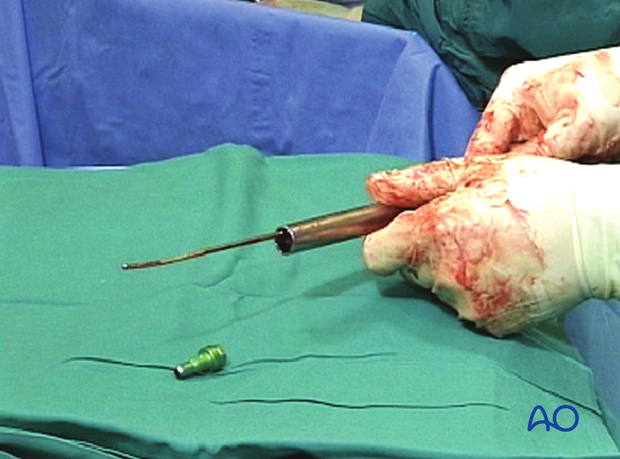
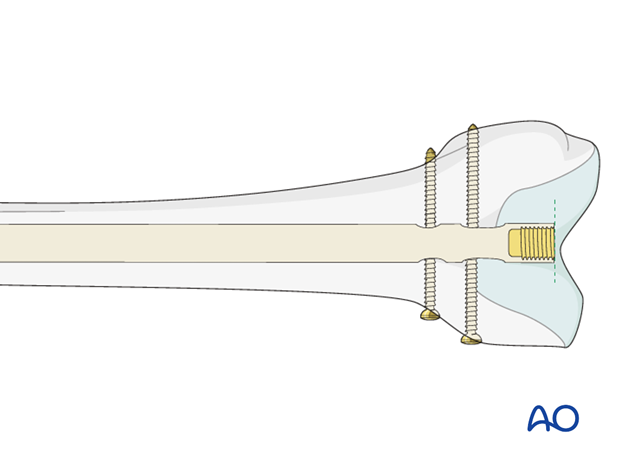
Verification of end cap placement
The cannulated end cap is tightened with the 11 mm ratchet wrench. Verification by the image intensifier shows that the end cap has been properly inserted into the nail.
14. Wound closure and assessment of alignment
Wound closure
The procedure ends with the closure of the fascia and the skin as separate layers.

Assessment of alignment
Before the patient is moved from the fracture table, rotation of the leg is observed clinically and compared to the contralateral leg.
With the femur now stable, it is possible to perform a thorough examination of the knee joint to rule out additional ligamentous injuries.

15. Aftercare
Compartment syndrome and nerve injury
Close monitoring of the femoral muscle compartments should be carried out especially during the first 48 hours, in order to rule out compartment syndrome.
Postoperative assessment
In all cases in which radiological control has not been used during the procedure, a check x-ray to determine the correct placement of the implant and fracture reduction should be taken within 24 hours.
Functional treatment
Unless there are other injuries or complications, mobilization may be started on postoperative day 1. Static quadriceps exercises with passive range of motion of the knee should be encouraged. If a continuous passive motion device is used, this must be discontinued at regular intervals for the essential static muscle exercises. Afterwards special emphasis should be placed on active knee and hip movement.
Weight bearing
Full weight bearing may be performed with crutches or a walker.
Follow-up
Wound healing should be assessed regularly within the first two weeks. Subsequently a 6 and 12 week clinical and radiological follow-up is usually made. A longer period may be required if the fracture healing is delayed.
Implant removal
Implant removal is not mandatory and should be discussed with the patient, if there are implant-related symptoms after consolidated fracture healing.













