Reconstruction plates
1. General considerations
Introduction
Reconstruction plates have been traditionally used in fractures of bones with complex 3-D geometry such as the pelvis and distal humerus.
In the distal humerus, the advent of modern precontoured anatomical periarticular locking plates has superseded the use of reconstruction plates. The following information regarding the application of reconstruction plates is only applicable to situations where more modern plates are not available.
Reconstruction vs anatomical plates
The reconstruction plate is not as stiff as an LCP or a precontoured plate. Because of the nonanatomical nature, they require extensive contouring to match the bony anatomy. This process is technically demanding and may further weaken the plate, especially if repeated contouring is performed or sharp bends are incorporated into the contouring.
The consequence of these factors is a risk of plate deformation and breakage, and loss of fracture reduction when the construct is loaded.
In fractures with metaphyseal fragmentation, at least one column (usually the lateral column) should be fixed with a small-fragment LCP in bridging mode. The other column can also be fixed with a small-fragment LCP or a reconstruction plate in bridging mode.
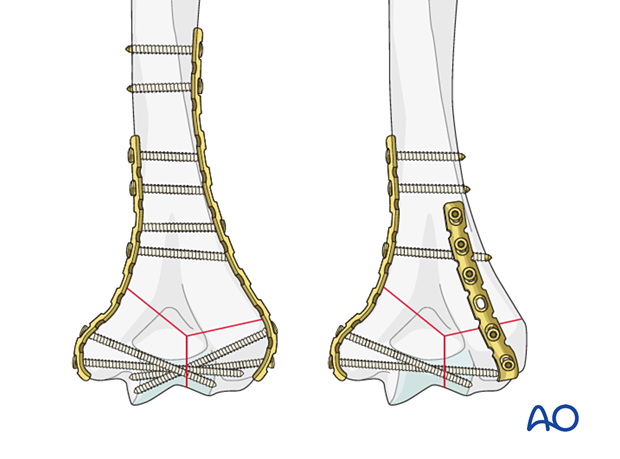
Parallel vs perpendicular plating
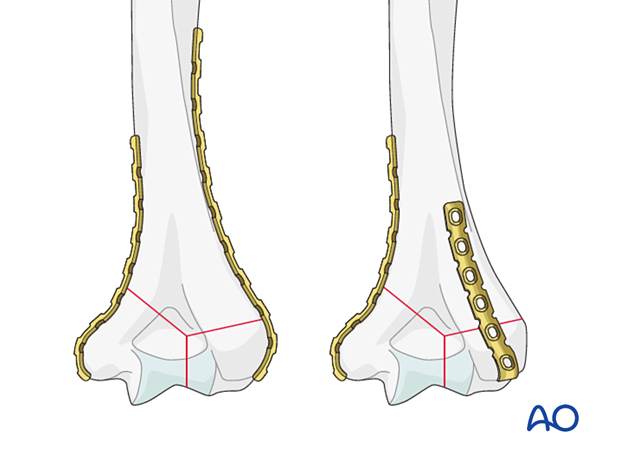
In the past, when periarticular locking plates were not available and reconstruction plates were used, it was evident that a parallel plating construct was more rigid than a perpendicular plating construct in biomechanical studies.
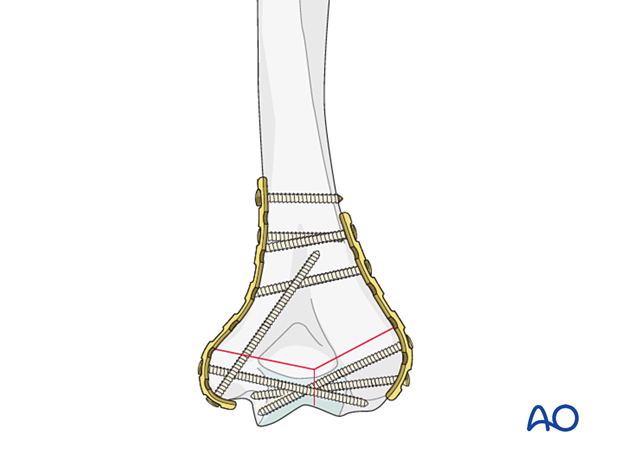
If reconstruction plates need to be used, a parallel plating technique—with a medial and lateral plate—is recommended following a principle-based technique that maximizes articular fracture fixation and supracondylar stability.
See also:
- Sanchez-Sotelo J, Torchia ME, O’Driscoll SW. Complex distal humeral fractures: internal fixation with a principle-based parallel-plate technique. Surgical technique. J Bone Joint Surg Am. 2008 Mar;90 Suppl 2 Pt 1:31–46.
A dorsolateral plate, instead of a lateral one, may be more appropriate in coronal shear fractures, or a third dorsolateral plate can be added in addition to a lateral plate when required. However, the blood supply to the fragments should be respected.

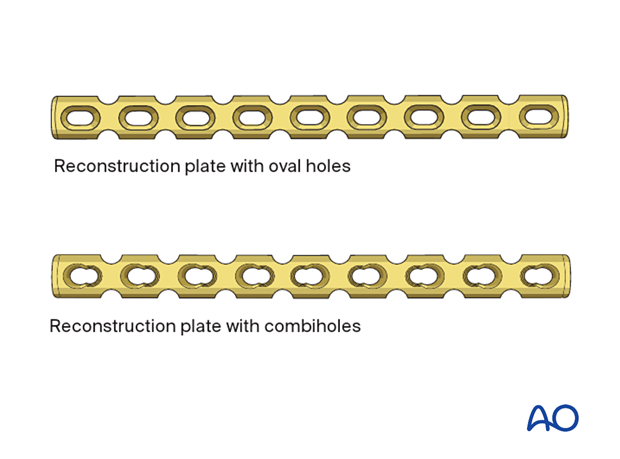
2. Plate characteristics
Reconstruction plates have deep notches on the edge of the plate. These notches are situated between the holes and allow contouring of the plate in all planes.
Three plate sizes are available for use with 2.7, 3.5, and 4.5 cortex screws.
The holes are oval to allow dynamic compression. They may have combiholes for dynamic compression and insertion of locking head screws.
3. Screw characteristics
Screw types
For application of the plate to the bone, three screw types may be used:
- Cortical screws
- Locking screws (fixed angle)
- Metaphyseal screws
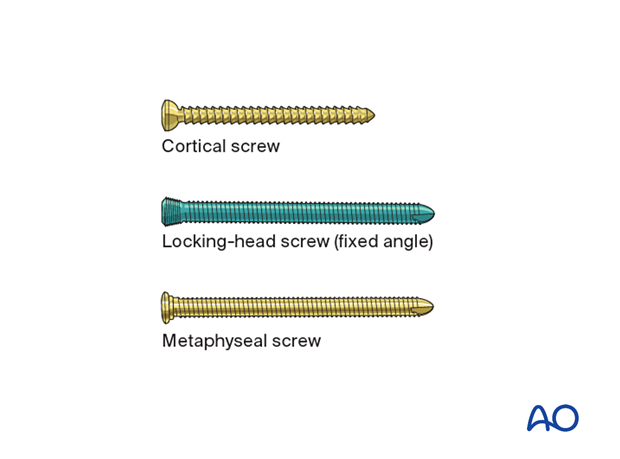
Combination of different screw types
If compression across a fracture segment is to be applied, this should be performed before adding locking screws in the same segment.
Recommended literature:
- Perren S, Babst R, Lambert S, et al. The issue of mixing principles in internal fixation. Pros and cons. ICUC Newsletter. 2015 Nov;3. Available at: www.icuc.net/static/media/9.563f04cf.pdf. Accessed November 3, 2020.
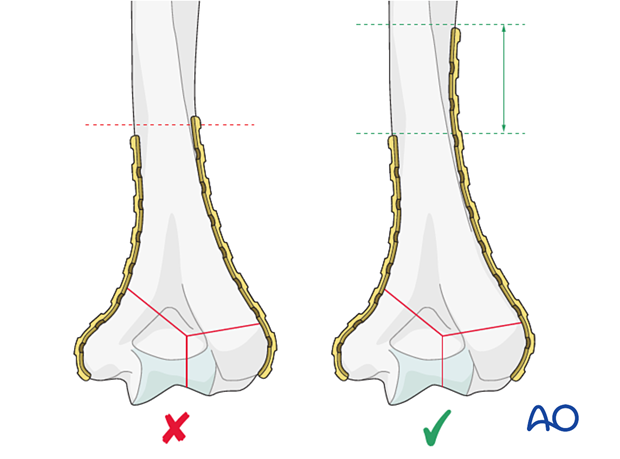
4. Plate length
The plate should extend distally enough to engage all articular fracture fragments and proximally enough so that three cortical screws engage both cortices of the proximal (shaft) fragment.
Select a plate long enough so that the resulting construct respects the principle of balanced fixation. This includes considerations of screw type, screw density and direction, and plate working length.
Recommended literature:
- Perren SM, Lambert S, Regazzoni P, et al. “Balanced fixation” in the surgical treatment of long bone fractures. ICUC One-Page Paper. 2015 Oct. Available at: https://www.icuc.net/static/media/8.97c978c2.pdf. Accessed February 16, 2021.
When using two plates, it is preferable to end the plates at different levels to avoid a stress riser.
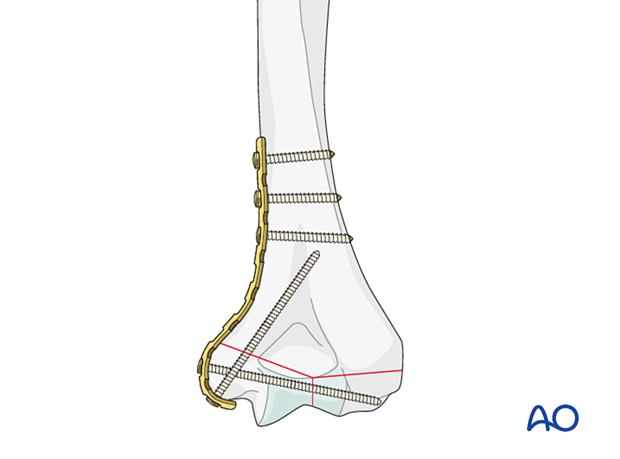
If the fracture exits low on the medial side, bend the plate around the epicondyle. This allows for an ascending screw for additional stability.
5. Plate contouring
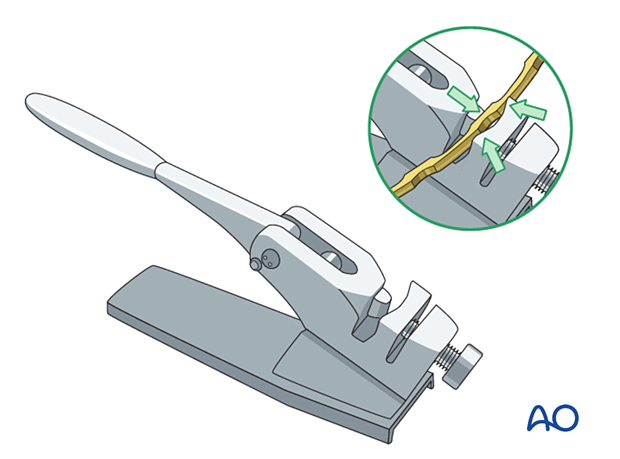
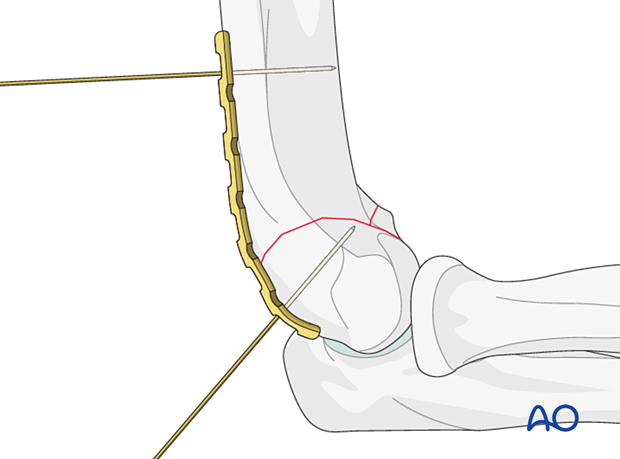
Use malleable templates to facilitate contouring.
Contour the plate with bending pliers and/or a bending press to fit the distal humerus anatomy.
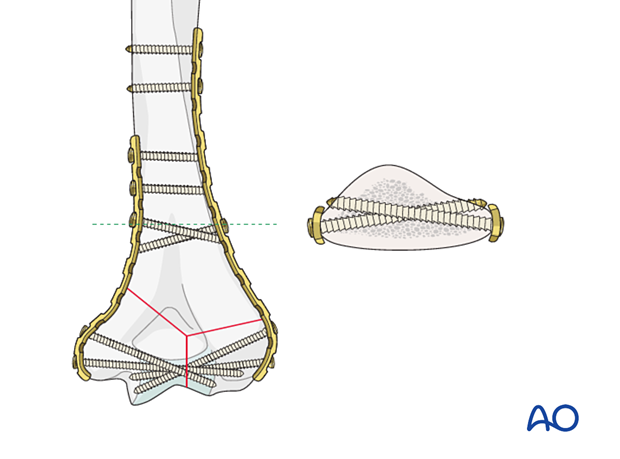
Slight undercontouring provides supplementary compression at the supracondylar level.
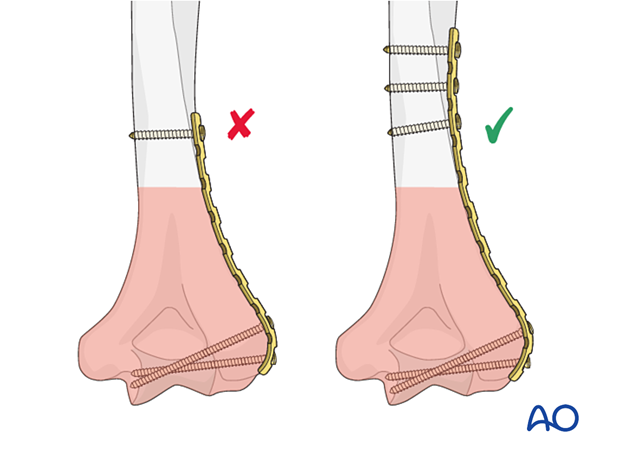
6. Plate positioning
Place a medial plate on the medial supracondylar ridge and usually slightly posteriorly on top of the soft tissues.
Place a lateral plate directly lateral and usually slightly posteriorly on top of the soft tissues.
Place a dorsolateral plate posteriorly on the lateral column on top of the soft tissues.
Do not strip the soft tissues from the corresponding column.
Provisionally fix the plate to the bone with forceps or K-wires.
The dorsolateral plate may curve around the capitellum, which has a nonarticular surface posteriorly.
In distal fractures, the reconstruction plate can be bent all the way to the edge of the articular surface. It will not interfere with the radial head during extension of the joint. The more bone is covered by the plate, the more stability that can be achieved.
7. Plating techniques
Compression plating (medial and lateral plating)
When there is bone contact between the articular and proximal fragments and the fracture is stable after reduction, apply compression, one column at a time:
- Insert the distal screws in the articular block. Use multiple long screws that engage in the far fragment.
- Compress with pointed reduction forceps and an eccentrically placed bicortical load screw in the hole proximal to the fracture line.
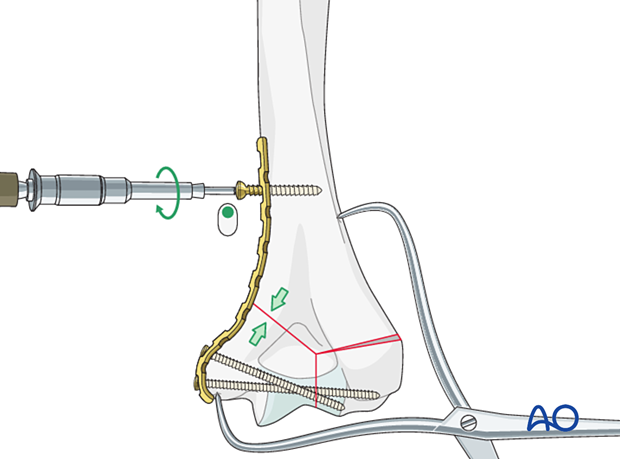
Bridge plating (medial and lateral plating)
When one column is comminuted, it should be bridged:
- Insert the distal screws in the articular block. Use multiple long screws that engage the fragments opposite to the plate.
- Reduce the fracture and insert a bicortical screw in a neutral mode in the hole proximal to the fracture plane.
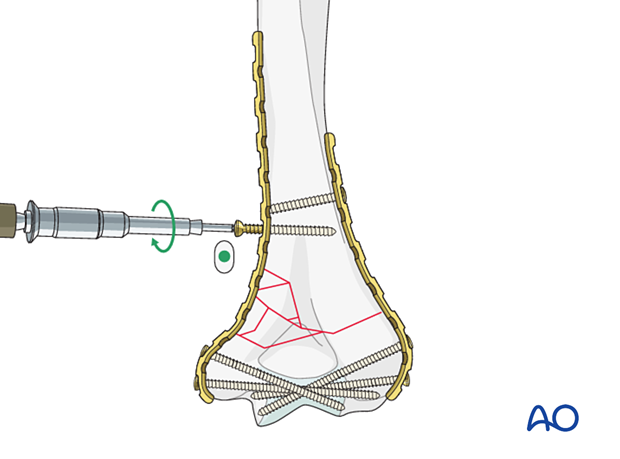
Insertion of remaining screws
Insert the remaining screws in the proximal fragment.
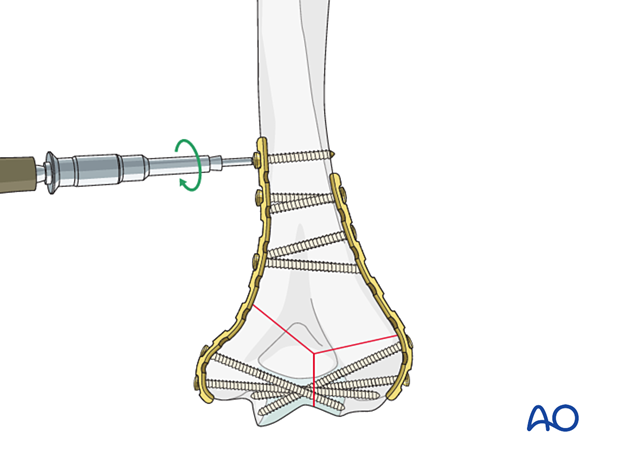
When the reassembled condylar mass is short and nonlocking plates are used, enhance the stability of the fixation with long, distal-to-proximal, 3.5 mm column screws.
Neutralization plating
A neutralization plate protects lag screw fixation of a simple metaphyseal or simple partial articular fracture.
The lag screw may be placed independently or through the plate, depending on the fracture configuration and the chosen plate.
A longer plate using a near-far plate screw insertion is recommended to balance the load distribution.
The plate screws are usually inserted in neutral mode.













