Medial plating
1. General considerations
Introduction
Plating with precontoured periarticular locking plates provides angular-stable fixation and is the most commonly used method of distal humeral fracture fixation.
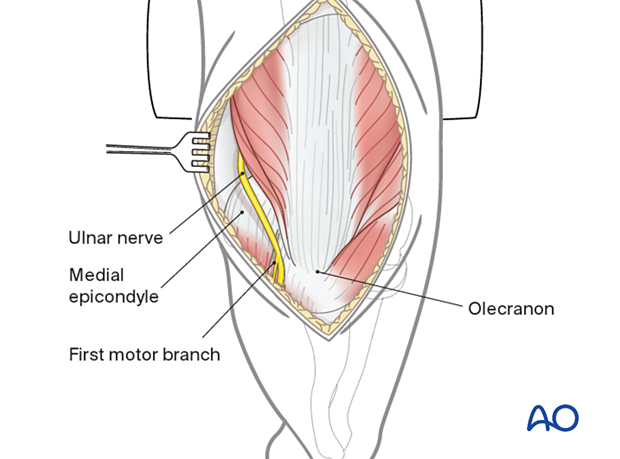
Ulnar nerve management
Take care to respect the ulnar nerve throughout the procedure.
If the nerve may be in contact with the plate at the end of the procedure, consider an ulnar nerve transposition.
The management of the ulnar nerve should be documented at the end of the operation.
See also the information about neurological protection and handling.
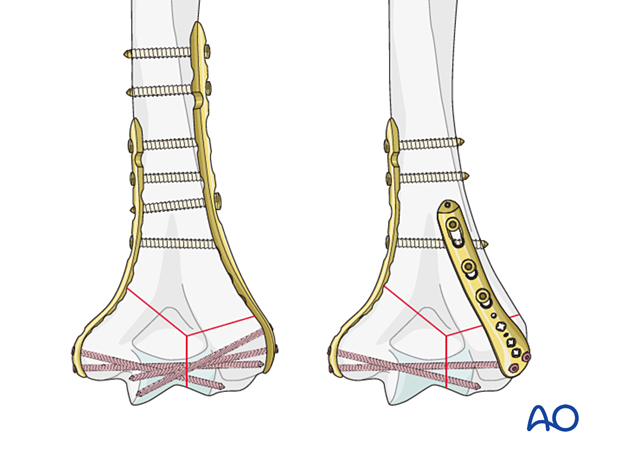
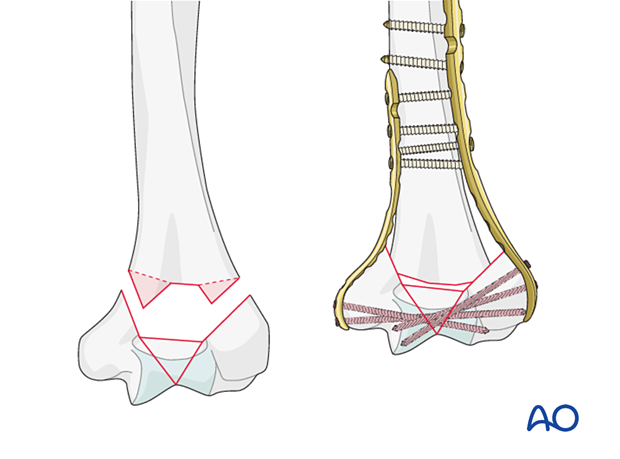
Parallel vs perpendicular plating
In conjunction with a lateral plate, a medial plate forms a parallel plating construct; with a dorsolateral, a perpendicular.
Both techniques—if applied using the correct principles—provide sufficient stability for fracture union. The decision to use either construct should be based on the fracture pattern and be individualized to each case.
If periarticular locking plates are not available and reconstruction plates need to be used, a parallel plating construct may be more appropriate than a perpendicular plating construct.
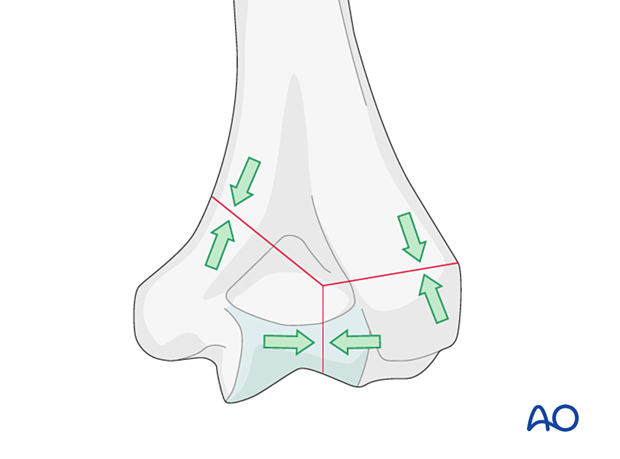
Principles of fracture compression in the distal humerus
In general, there are two sites where fracture compression should be achieved through solid bony contact across the fracture:
- In the articular block between the articular fragments
- At the supracondylar level
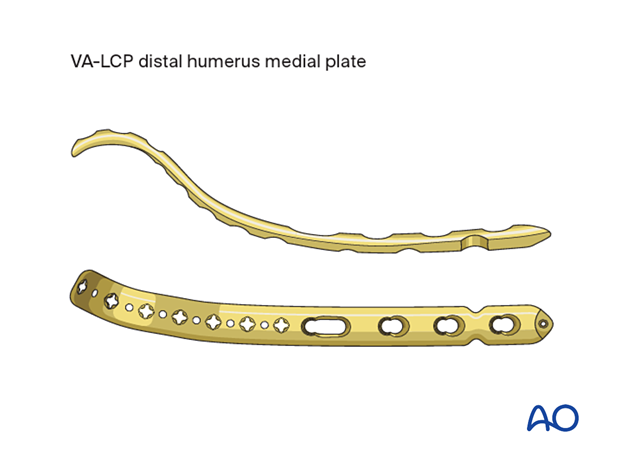
2. Plate characteristics
These plates usually have smaller locking holes in the distal part to capture the articular fragments and larger locking/nonlocking holes proximally to address the metadiaphyseal segment/fragments.
3. Screw characteristics
Screw types
For application of the plate to the bone, three screw types may be used:
- Cortical screws
- Locking screws (variable angle or fixed angle)
- Metaphyseal screws

Combination of different screw types
If compression across a fracture segment is to be applied, this should be performed before adding locking screws in the same segment.
Recommended literature:
- Perren S, Babst R, Lambert S, et al. The issue of mixing principles in internal fixation. Pros and cons. ICUC Newsletter. 2015 Nov;3. Available at: www.icuc.net/static/media/9.563f04cf.pdf. Accessed November 3, 2020.
4. Plate length
The plate length should allow placement of at least three screws proximal to the most proximal fracture line.
If there is metaphyseal fracture comminution, a longer plate should be selected for bridge plating.
Select a plate long enough so that the resulting construct respects the principle of balanced fixation. This includes considerations of screw type, screw density and direction, and plate working length.
Recommended literature:
- Perren SM, Lambert S, Regazzoni P, et al. “Balanced fixation” in the surgical treatment of long bone fractures. ICUC One-Page Paper. 2015 Oct. Available at: https://www.icuc.net/static/media/8.97c978c2.pdf. Accessed February 16, 2021.
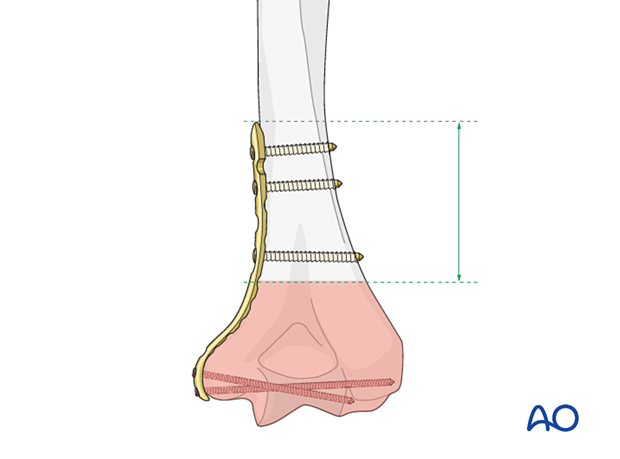
When using two plates, it is preferable to end the plates at different levels to avoid a stress riser.
Some medial plates wrap around the medial epicondyle and are particularly useful for low transcondylar fractures.
This allows a higher variation of screw trajectories, especially an ascending screw insertion.
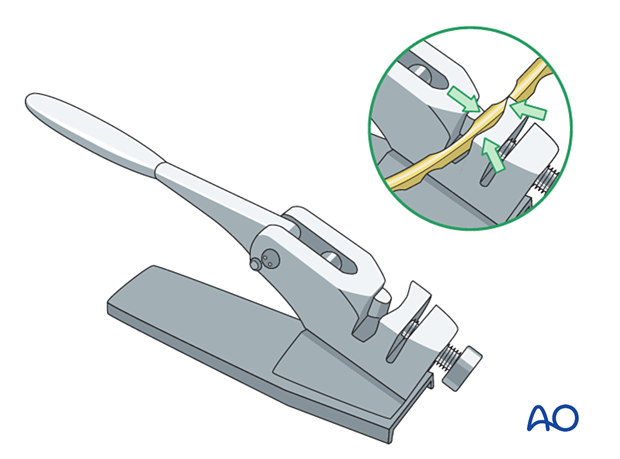
5. Plate contouring
Modern anatomical periarticular plates are designed to match the anatomy of most patients. Therefore, contouring is not usually required.
If the plates do not fit the distal humerus following reduction, confirm first that the reduction is anatomical under image intensification.
In some instances, contouring may still be required.
Avoid bending the plate through screw holes as this will weaken the plate and deform locking holes, which may hinder screw locking.
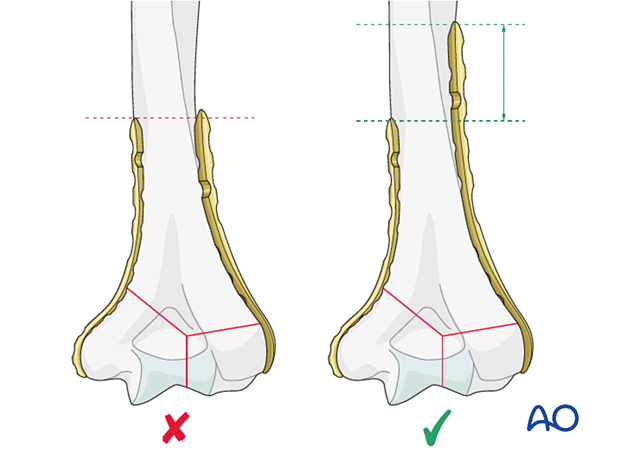
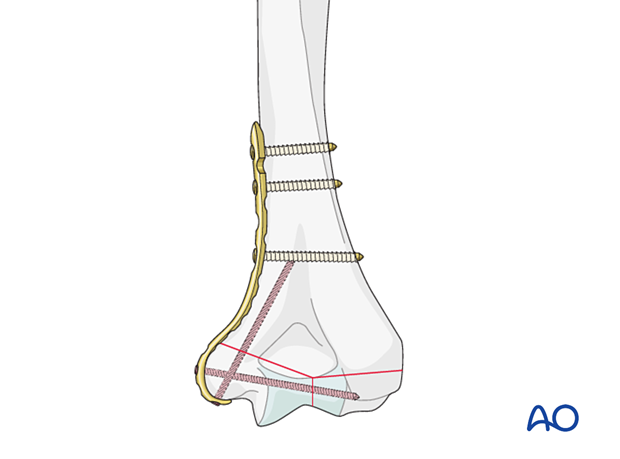
6. Plate positioning
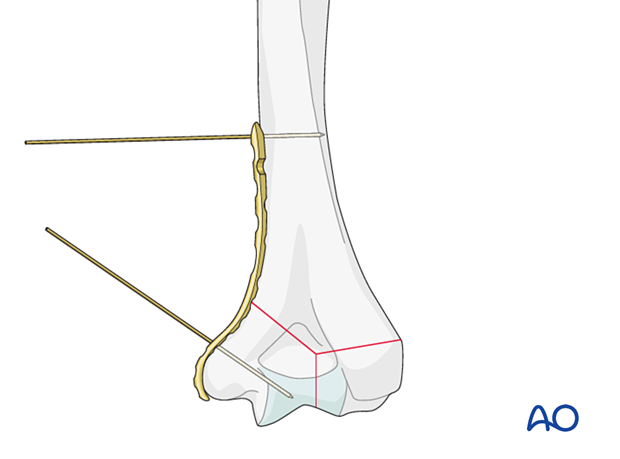
Dissect and protect the ulnar nerve throughout the whole procedure.
Release the intermuscular septum from the medial ridge of the distal humerus to allow for plate application.
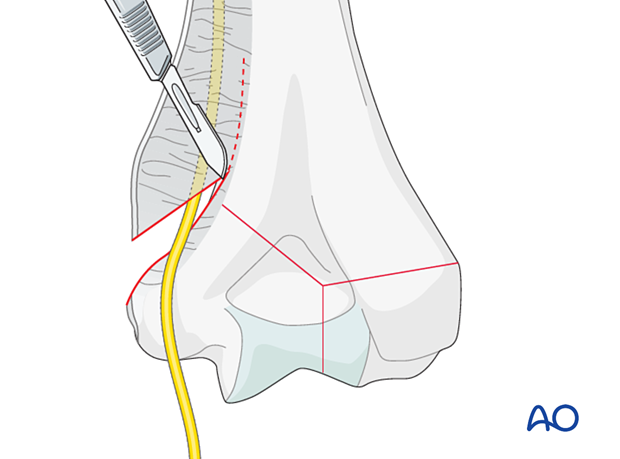
Place the plate to the medial aspect of the distal humerus, distally on top of the soft tissues.
Provisionally fix the plate to the bone with a forceps or K-wires.
7. Insertion of first proximal screw
Provisionally fix the plate to the bone with a cortical position screw through one of the combiholes proximal to the fracture zone.
8. Insertion of distal screws
Introduction
The distal screws can be locking or metaphyseal screws.
Locking screws are typically used to provide angular-stable fixation.
Metaphyseal screws are used to provide intraarticular fracture compression.
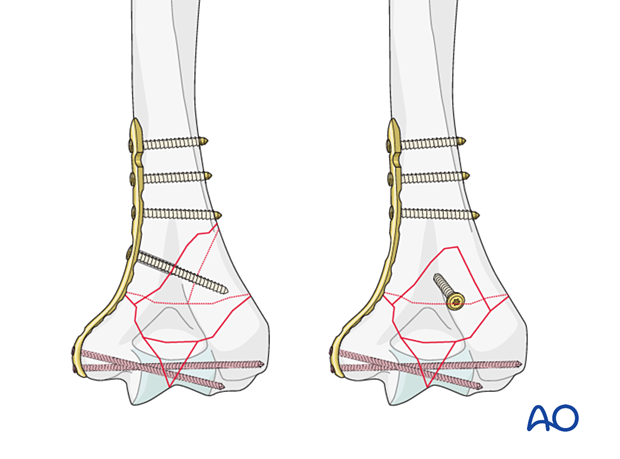
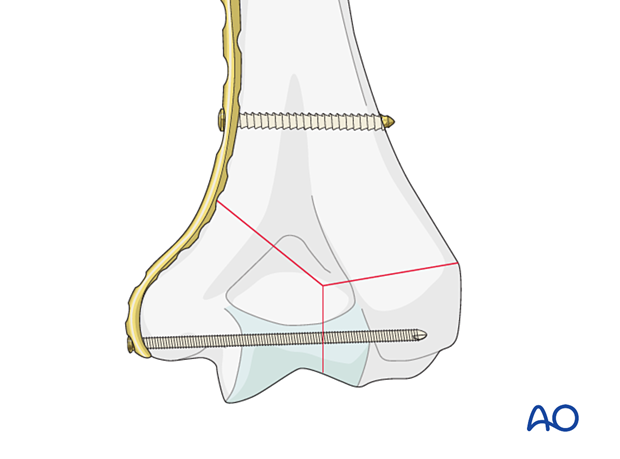
Variable angle locking screws
The distal screws are locking screws. They form a fixed angle construct with the plate.
Insert these screws in a fixed or variable angle mode depending on the fracture pattern.

Screws should be long enough to engage fragments on the opposite side to the plate.
The goal is to insert at least two screws (locking or metaphyseal) long enough to engage the fragments on the opposite side.
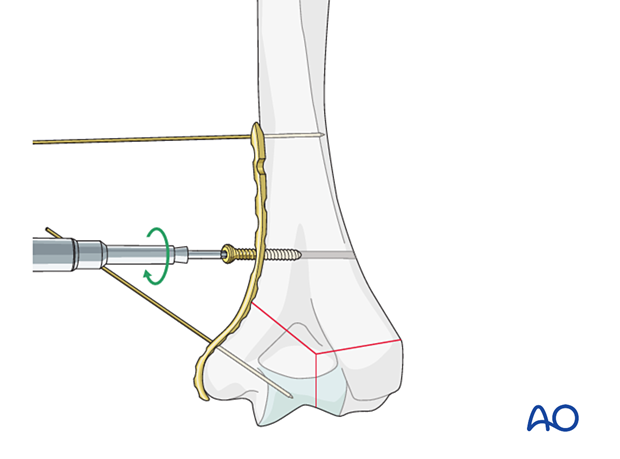
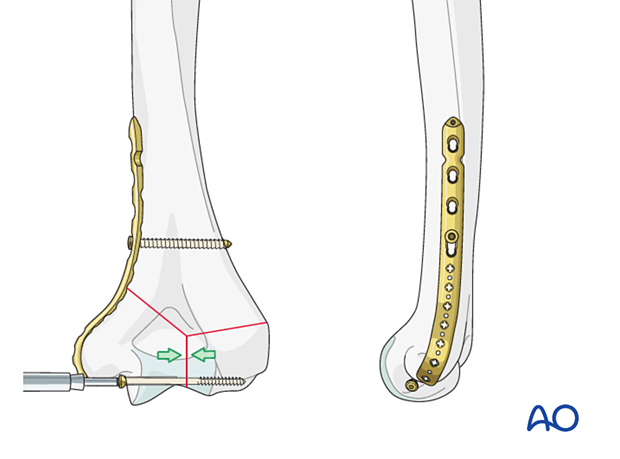
Metaphyseal screw
A metaphyseal screw is a 2.7 mm screw with high pitch and low thread amplitude, designed to recess into the locking holes of the distal plate without providing angular stability. It allows for direct stabilization of the articular fracture to the plate.
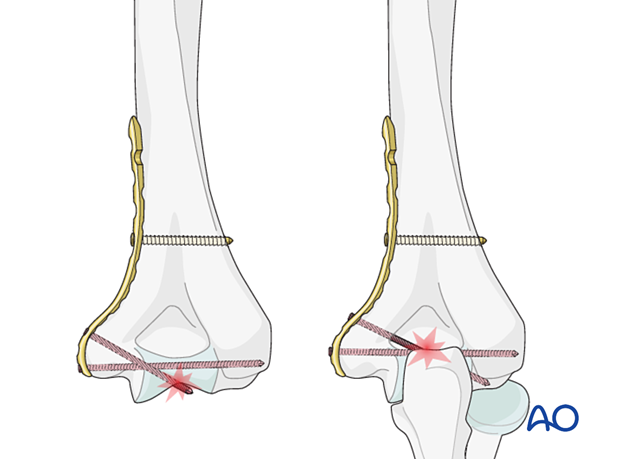
Pitfalls: articular penetration of screws
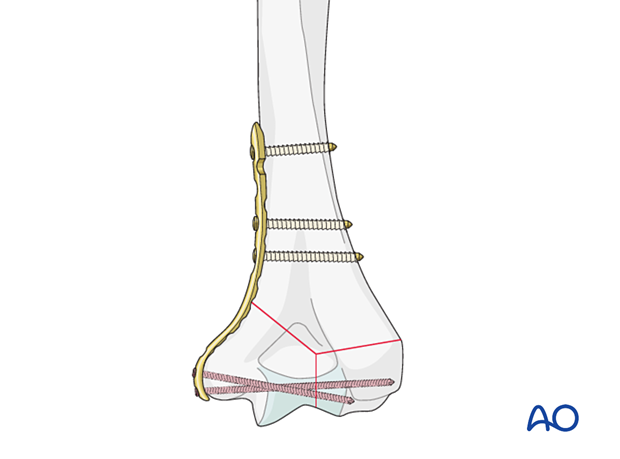
9. Fixation of articular block
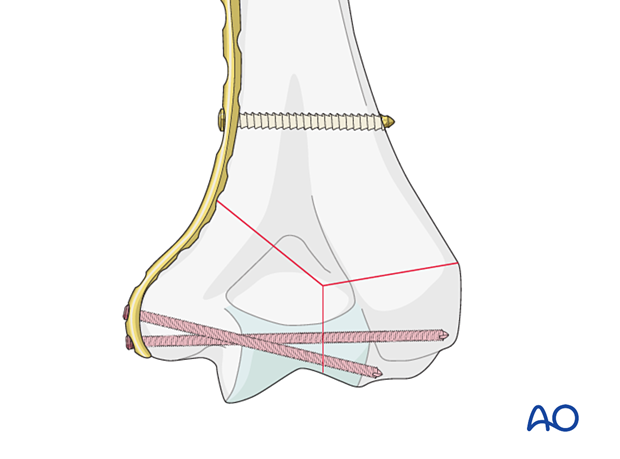
Interfragmentary compression of simple articular fracture
If there is a simple fracture of the articular block, apply extrinsic or intrinsic compression by one of the following options.
- Extrinsic compression applied by a forceps and maintained with a locking screw through the plate
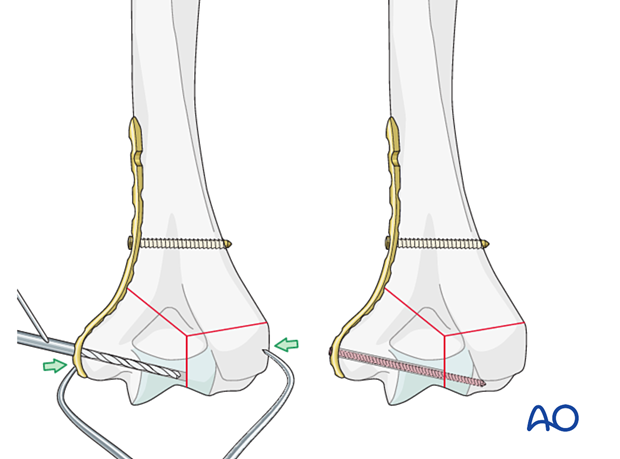
- Intrinsic compression applied by insertion of a transverse lag screw separate to the plate. The screw may be a partial threaded cancellous screw or an overdrilled fully threaded cortical screw. ...
... Add a locking screw through the articular block.
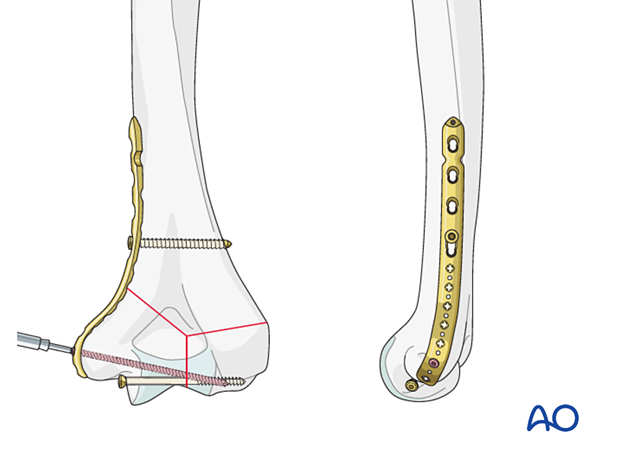
- Intrinsic compression applied by insertion of a metaphyseal lag screw through the plate
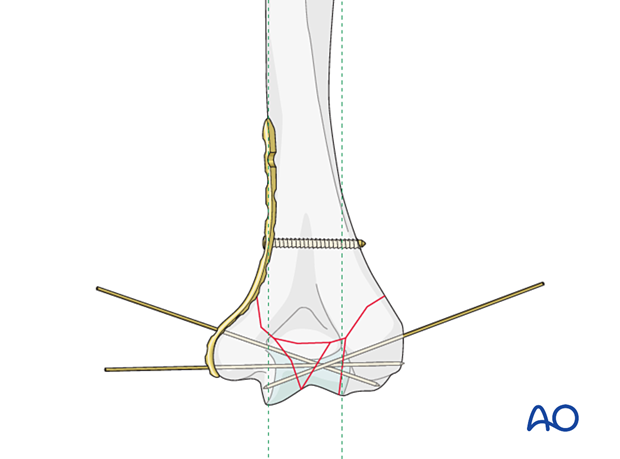
Fixation of multifragmentary articular fractures
Reconstruct the articular block with K-wires.
Place locking screws through the plate into the articular block to maintain reduction without applying excessive compression with forceps. The locking screws are used as positioning screws to maintain reduction.
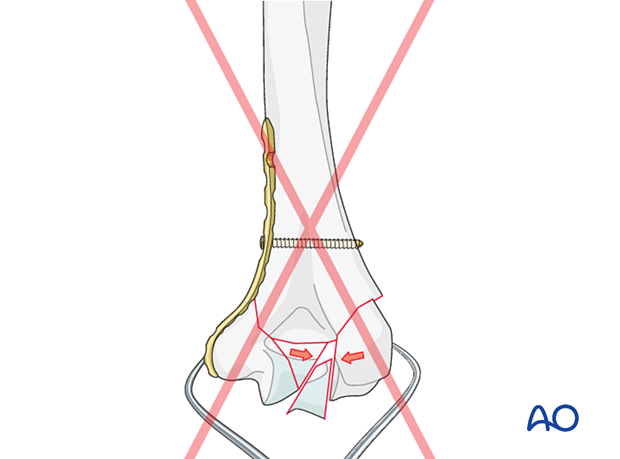
Pitfall: overcompression
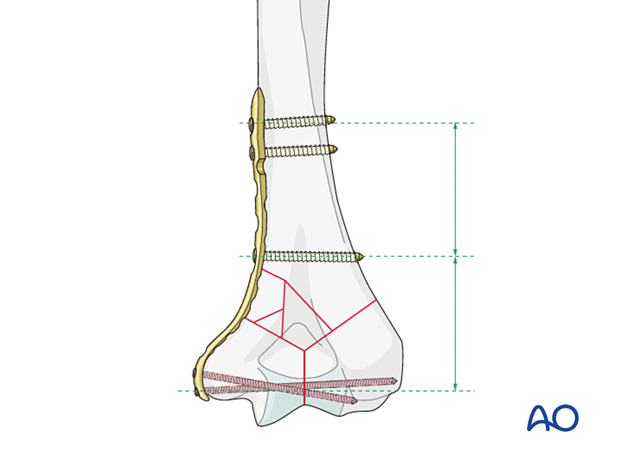
10. Fixation of supracondylar fracture
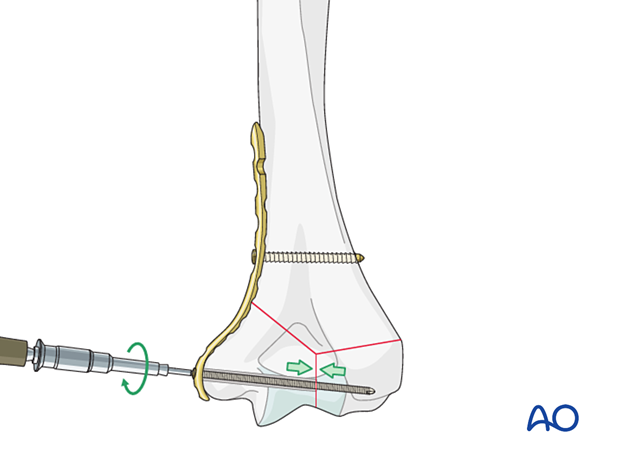
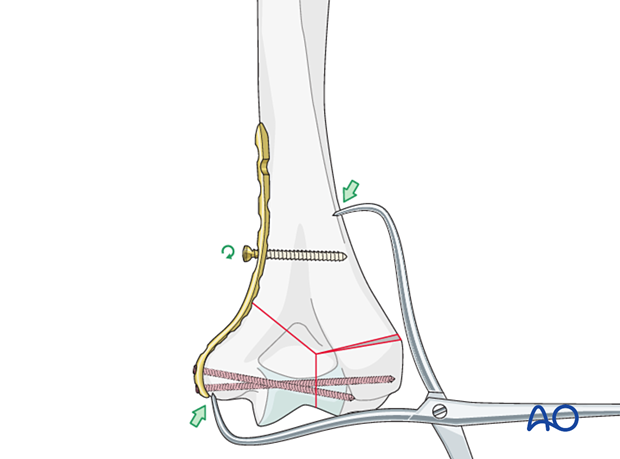
Supracondylar compression
When the metaphyseal component of the fracture is simple, compression may be applied between the articular block and the humeral shaft.
Loosen the initially placed cortical screw.
Use forceps applied between the articular block and the metadiaphyseal segment to achieve compression.
Retighten the screw.
Insert further cortical or locking head screws into the proximal plate holes as needed.
Compression may also be achieved by inserting a further proximal cortical screw eccentrically in a combihole.
Before tightening this screw, loosen the first bicortical one so the plate may slide for compression of the fracture.
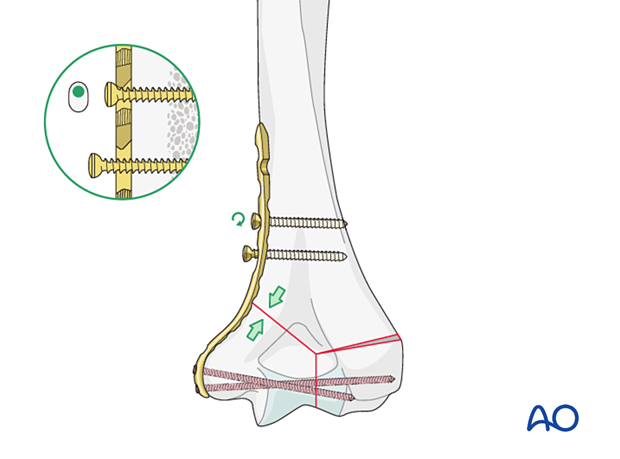
Insert further bicortical and/or locking screws as necessary to stabilize the fracture.
Two proximal screws may be sufficient in good-quality bone. The second screw should then be inserted in the most proximal plate hole for a near-far solution.
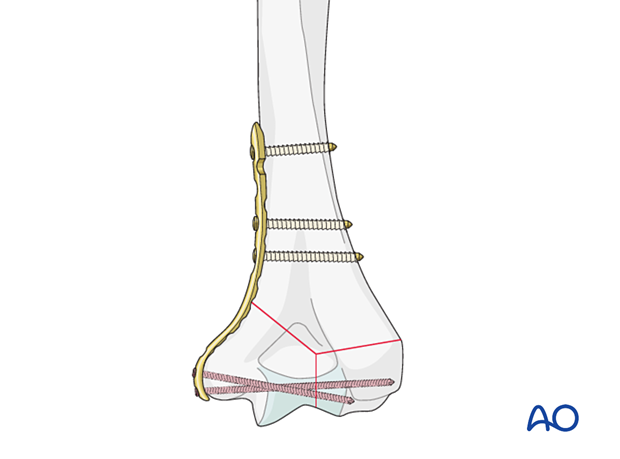
Bridge plating
When the metaphyseal component of the fracture is complex, it may not be possible to achieve compression.
In this case, the metaphyseal segment should be bridged.
If this is performed, a longer plate using a near-far screw insertion is recommended to balance the load distribution.
If the first proximal screw is placed close to the fracture zone, insert the second bicortical screw in the most proximal plate hole.
Neutralization plating
A neutralization plate protects lag screw fixation of a simple metaphyseal or simple partial articular fracture.
The lag screw may be placed independently or through the plate, depending on the fracture configuration and the chosen plate.
A longer plate using a near-far plate screw insertion is recommended to balance the load distribution.
The plate screws are usually inserted in neutral mode.
Pearl: managing metaphyseal comminution or bone loss

Option: lag screw
Some simple metaphyseal fractures may be amenable to lag screw compression outside or through the plate depending on the fracture plane and respecting soft-tissue attachments.
A normal lag screw technique may be used to add compression and stability to the overall fixation.