ORIF - Lag screw from posterior with or without plate
1. Principles
General considerations
Hoffa fractures involve important load-bearing areas of the knee joint surface, and the principles of anatomical reduction and absolute stability of fixation apply.
In general, a buttress plate with lag screws is recommended.
However, if the fragment is small, then isolated lag screws may be the only fixation possible.
The indirect lag screw technique from anterior is not recommended as the thread will be too long and will not achieve adequate stability and compression of the fragment.
Similar principles apply if both condyles are fractured.
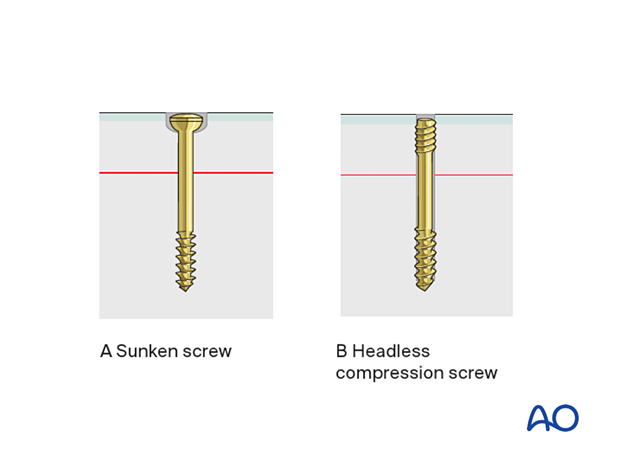
Screw types
None of the implants can project above the articular surface. This can be achieved by countersunk lag screws (A) or headless compression screws (B).
At least two screws should be used, in order to prevent fragment rotation
For this procedure, 3.5 mm cannulated headless
compression screws or standard 3.5 mm lag screws can be used. However,
different size screws can be used depending on fragment size.
2. Patient preparation and approach
Patient preparation
The procedure is performed with the patient placed supine and the knee flexed 20-30°.
Approach
For lateral Hoffa injuries, the Swashbuckler approach or the Gerdytubercle osteotomy approach is used.
For medial Hoffa injuries, the internervous medial approach is used.
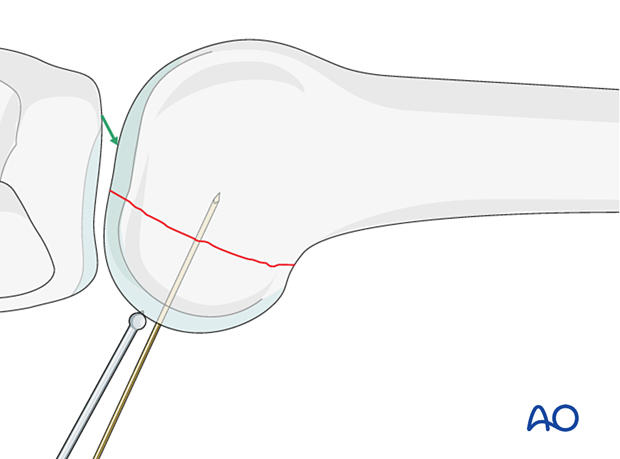
3. Reduction
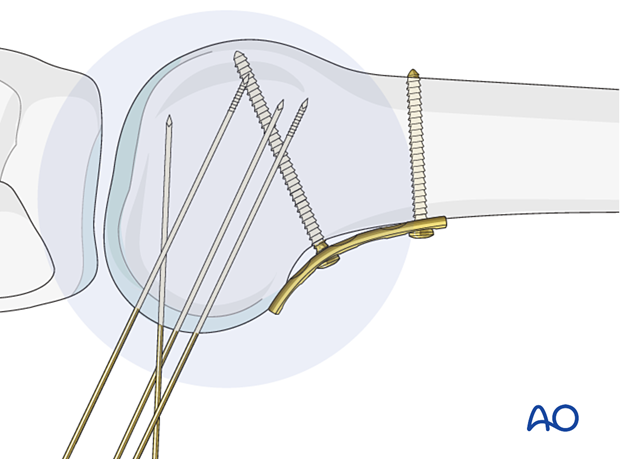
Reduce the fracture using a small ball-spiked pusher and secure it temporarily with a K-wires.
Make sure that the K-wires does not conflict with the planned plate position and screw track.
4. Fixation
Principle
To enhance the stability and to avoid axial load on the fracture (especially in the osteoporotic bone), a buttress plate is needed to prevent cranial displacement of the fragment.
The plate needs to be placed according to the position of the unstable fracture fragment. Occasionally this fracture fragment is lateral.
A wide range of plates can be utilized and as an example, we will here use a simple slightly under-contoured 3.5 mm narrow plate.
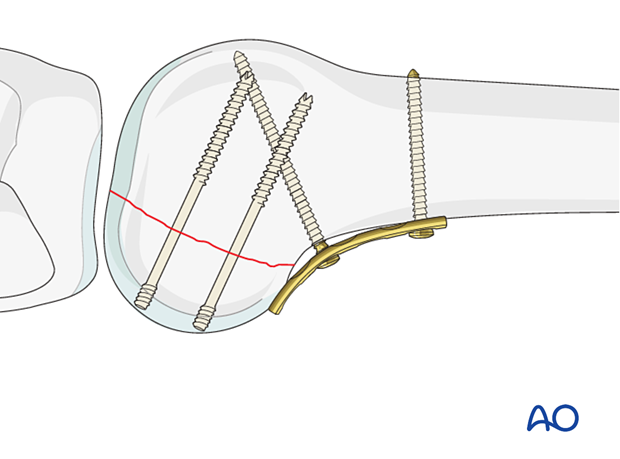
Plate application
Apply the plate to the posterior aspect of the distal femur. This plate will need to be positioned as far distal as possible without affecting the articular surface. To press the under-contoured plate firmly to the femur, insert a standard cortical screw just proximal to the fracture line in neutral mode.
Secure the plate with one or more bicortical cortical screws proximal to the first screw.
Additional screws can be inserted in the distal aspect of the plate if they fit on the non-articular surface.
All these screws are inserted in neutral mode.
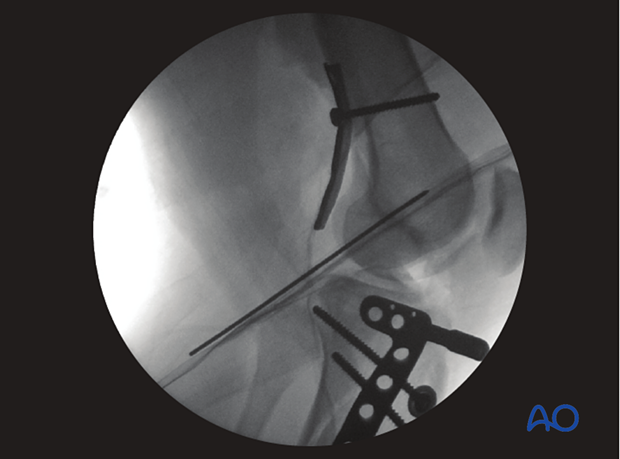
This intraoperative image demonstrates an operation
where the posterior Hoffa has been reduced and held temporarily with a K-wire
and buttressed with a posterior plate.
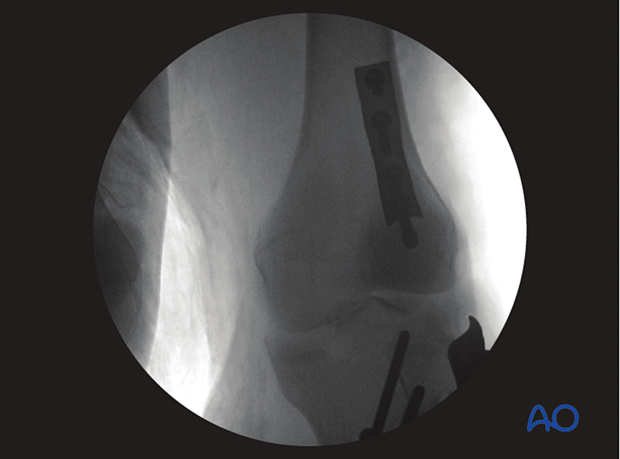
Postoperative image with posterior buttress plate in place.
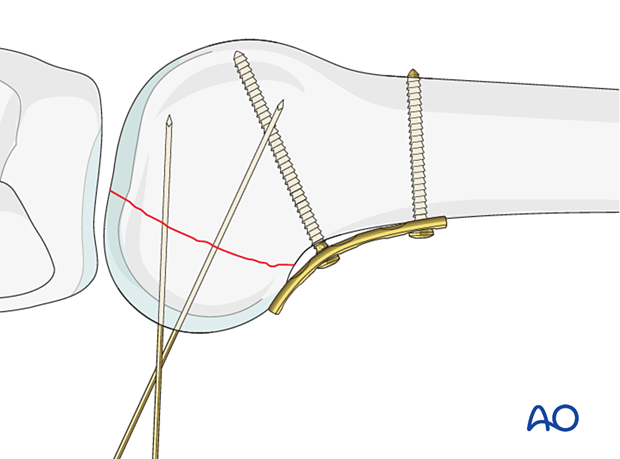
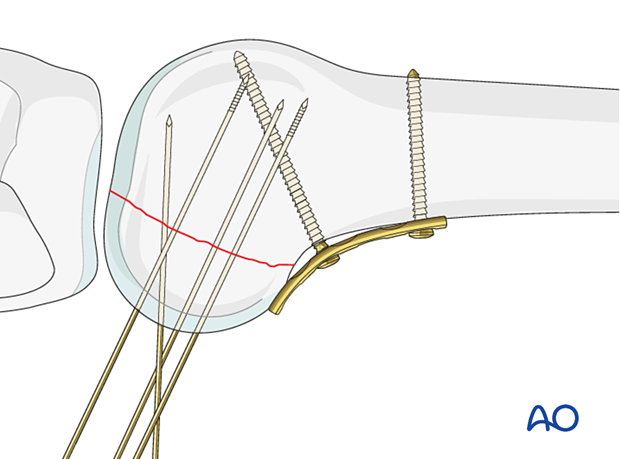
Guide-wire insertion
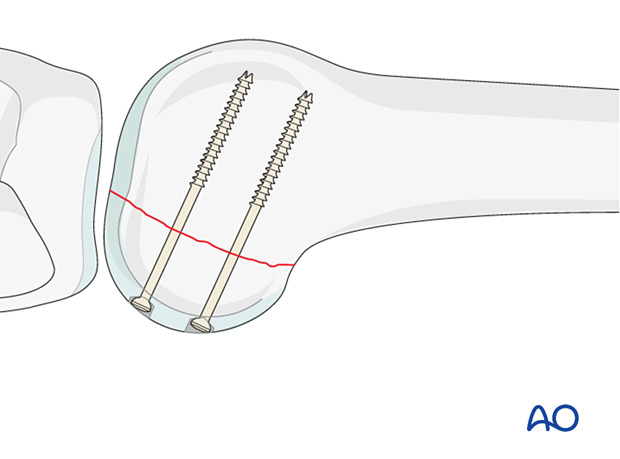
Insert two guide wires perpendicular to the fracture
plane. Make sure not to penetrate the far cortex.
Check guide-wire insertion
Check the guide-wire position under image intensifier control, in the lateral and oblique views.
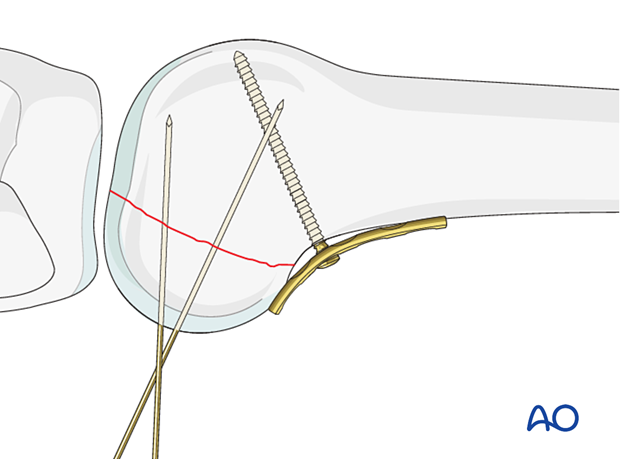
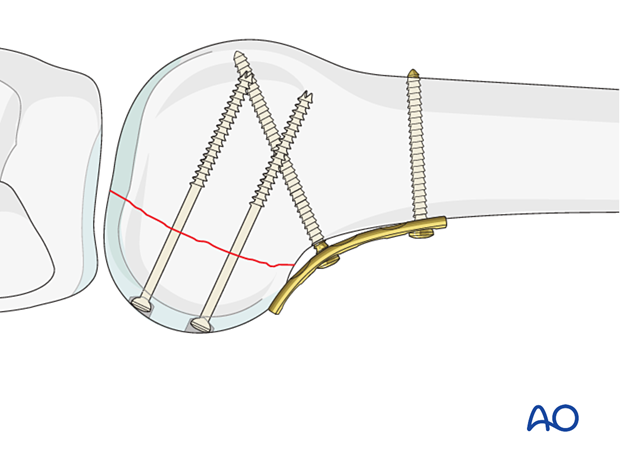
Headless compression screw insertion
Insert headless compression screws, using the cannulated screwdriver, and check under image intensifier control in the lateral view that the screw length was chosen appropriately.
Alternative: Standard screws
The lag screws are inserted according to the standard technique for cancellous lag screws under image intensifier control. Care is taken to countersink in order to prevent protruding screw heads.
5. Case

6. Aftercare
Impediments to the restoration of full knee function after distal femoral fracture are fibrosis and adhesion of injured soft tissues around the metaphyseal fracture zone, joint capsular scarring, intra-articular adhesions, and muscle weakness.
Early range of motion helps restore movement in the early postoperative phase. With stable fracture fixation, the surgeon and the physical therapy staff will design an individual program of progressive rehabilitation for each patient.
The regimens suggested here are for guidance only and not to be regarded as prescriptive.
Functional treatment
Unless there are other injuries or complications, knee mobilization may be started immediately postoperatively. Both active and passive motion of the knee and hip can be initiated immediately postoperatively. Emphasis should be placed on progressive quadriceps strengthening and straight leg raises. Static cycling without load, as well as firm passive range of motion exercises of the knee, allow the patient to regain optimal range of motion.
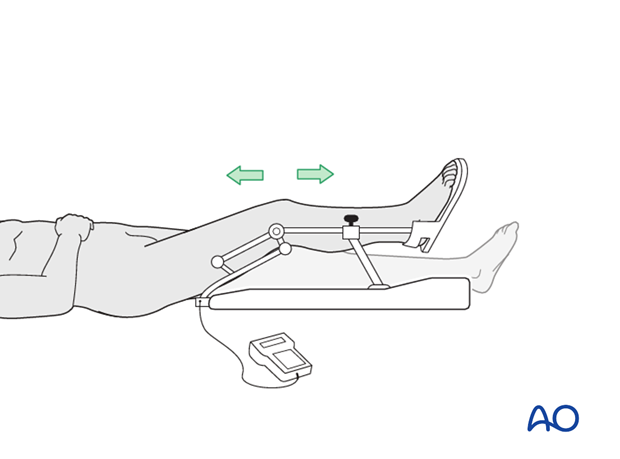
Weight bearing
Touch-down weight-bearing (10-15 kg) may be performed immediately with crutches, or a walker. This will be continued for 6-10 weeks postoperatively. This is mostly to protect the articular component of the injury, rather than the shaft injury. Touch-down weight-bearing progresses to full weight-bearing gradually, over a period of 2 to 3 weeks (beginning at 6–10 weeks postoperatively). Ideally, patients are fully weight-bearing, without devices (e.g., cane) by 12 weeks.
Follow-up
Wound healing should be assessed at two to three weeks postoperatively. Subsequently 6-week, 12-week, 6-month, and 12-month follow-ups are usually made. Serial x-rays allow the surgeon to assess the healing of the fracture.
Implant removal
Implant removal is not essential but should be discussed with the patient if there are implant-related symptoms after consolidated fracture healing.
Thrombo-embolic prophylaxis
Thrombo-prophylaxis should be given according to local treatment guidelines.













