MIO - dynamic condylar screw system (DCS)
1. Principles
Introduction
The DCS system is a versatile plate which can be applied in a bridging mode (fragmentary supracondylar fracture component) and with compression (simple supracondylar fracture component).
However, when a minimally invasive approach is used, compression is not feasible, and it is therefore not used in simple oblique or transverse supracondylar fractures.
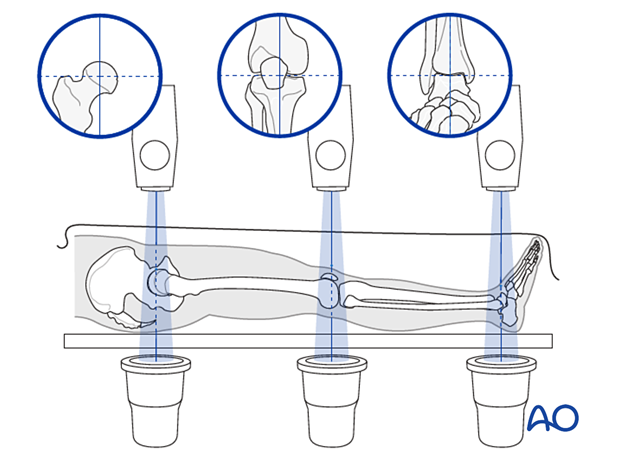
When a minimally invasive (MIO) approach is used, incisions are made proximally and distally, and the plate is inserted through a submuscular tunnel. This requires image intensifier monitoring.
Teaching video
Fixation of a C1 fracture with the dynamic condylar screw system.
Bridging mode
When used in bridging mode, the plate is an internal fixator used as an extramedullary splint, fixed to the two main fragments, leaving the intermediate fracture zone untouched. Anatomical reduction of intermediate fragments is neither sought nor necessary.
Direct manipulation of intermediate fragments would risk disturbing their blood supply. If the soft-tissue attachments to these fragments are preserved, and the fragments are generally aligned, healing is unimpaired.
Alignment of the main shaft fragments can be achieved indirectly with the use of:
- traction
- reduction tools
- the implant itself
Mechanical stability, provided by the bridging plate, is adequate for gentle functional rehabilitation and results in satisfactory indirect healing (callus formation). Occasionally, a larger wedge fragment might be approximated to the main fragments with a lag screw.
Compression mode
This implant is particularly useful for obtaining metaphyseal compression. If a fracture pattern can be reduced to a "simple" metaphyseal fracture pattern (such as an intact wedge fracture where the wedge is fixed to the main fragment), then compression can be used for the metaphyseal "simple" fracture.
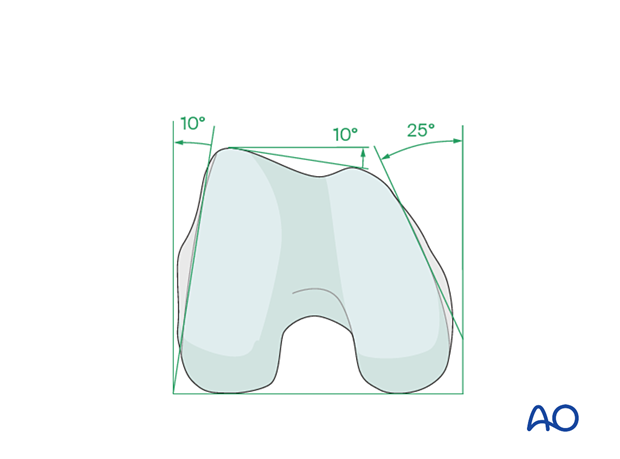
Anatomy of the distal femur
The distal femur has a unique anatomical shape. Seen from an end-on view, the lateral surface has a 10° inclination from the vertical, while the medial surface has a 20–25° slope.
A line is drawn from the anterior aspect of the lateral femoral condyle to the anterior aspect of the medial femoral condyle (patellofemoral inclination) that slopes approximately 10°. These anatomical details are important when inserting screws. In order to avoid joint penetration, these devices should be placed parallel to both the patellofemoral and femorotibial joints planes.
The muscle attachments to the distal femur are responsible for the typical displacement of the distal articular block following a supracondylar fracture, namely shortening with varus and extension deformity. Shortening is due to the pull of the quadriceps and hamstring muscles, while the varus and extension deformity is caused by the unopposed pull of the adductors and gastrocnemius, respectively.
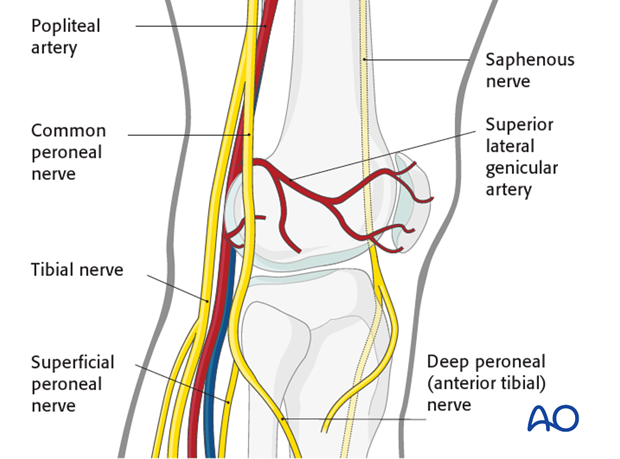
The popliteal vessels, the tibial nerve, and the common peroneal nerve lie near the posterior aspect of the distal femur. Because of this, vascular injuries occur in about 3% and nerve injuries in about 1% of fractures of the distal femur.
There are no significant arteries, veins, or nerves on the lateral side of the knee.
There may be bleeding from the lateral genicular arteries, which will need to be controlled using diathermy.
At the posterior aspect of the knee lie the popliteal artery, nerve, and vein. It must be borne in mind that these structures can be damaged by the injury or can be damaged by the surgeon during the reconstruction.
2. Patient preparation and approach
Positioning
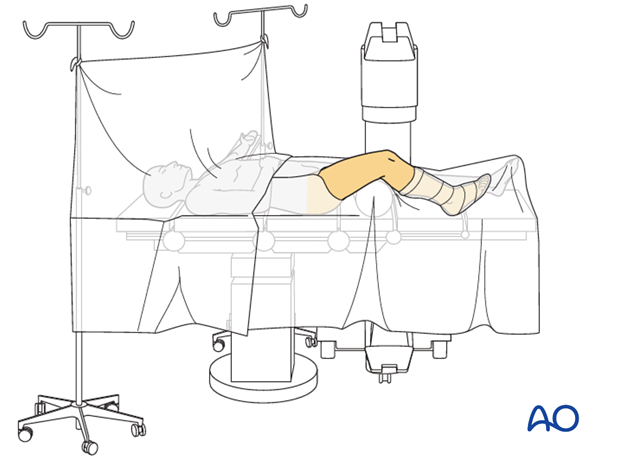
This procedure may be performed with the patient in one of the following positions:
- Supine position knee flexed 30°
- Supine position knee flexed 90°
- Lateral decubitus (particularly in obese patients)
Approach
The MIPO approach for an extra-articular fracture is simple because the articular block is intact. The small opening directly lateral over the end segment should be only as large as to allow the insertion of the implant.
Proximally small incisions on the side of the thigh laterally are used, but only enough to allow for the insertion of individual screws.
3. Reduction
Consideration must be given to fracture reduction in:
- Varus/valgus
- Flexion/extension
- Internal/external rotation
- Translation
- Lengthening/shortening
Reduction can be performed with a single reduction tool (eg, large distractor), or by combining several steps (for example fracture table +/- external fixator, +/- reduction via the implant, etc) to achieve the final reduction.
The preferred method depends on the fracture and soft-tissue injury pattern, the chosen stabilization device, and the experience and skills of the surgeon.
If a large fragment has separated from the fracture zone and impaled the adjacent muscle, direct reduction may be required.
Reduction aids
Closed reduction is aided by:
- Complete anesthetic muscle relaxation
- A bolster in the supracondylar region to reduce the hyperextension deformity of the distal femoral articular block.
- Manual traction
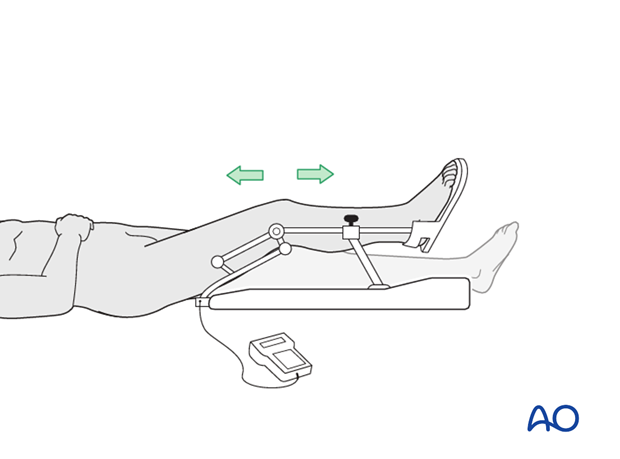
- Femoral distractor

Reduction can also be aided by:
- Use of Schanz pins inserted into the medial, or lateral, femoral articular block to correct varus or valgus angulation of the femoral block.
- Insertion of a Schanz pin from anterior to posterior in the distal femoral articular block, which can be used to correct hyperextension.
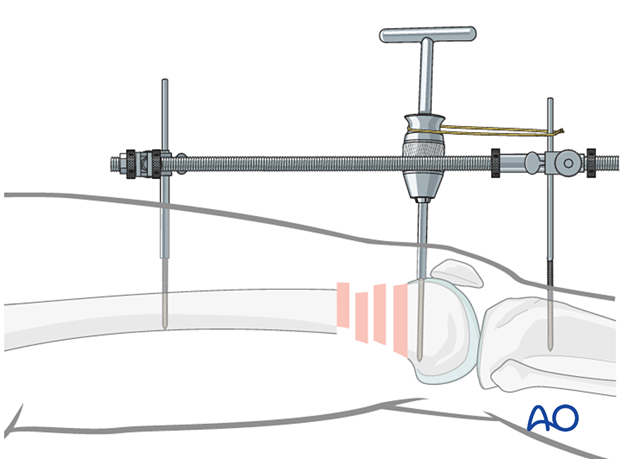
Use of external fixator/femoral distractor
Some surgeons find it useful to use an external fixator (or femoral distractor) from the proximal femur to the proximal tibia.
Due to the pull of the gastrocnemius muscle, the distal fragment tends to be displaced into extension at the metaphyseal fracture area, when distraction is applied.
To avoid this, the knee is brought into full extension, and the distal femoral fragment is stabilized in this position to the tibia. A Schanz screw is inserted in the distal femoral articular block and used to counter the pull of the gastrocnemius. When reduced, a temporary cerclage wire is used to lock the position of the Schanz screw relative to the distractor.
Insert the proximal and distal fixator (distractor) pins carefully in order not to conflict with the later plating procedure. Safe positions would be anterolateral or anterior on the femur.
Verification of successful reduction
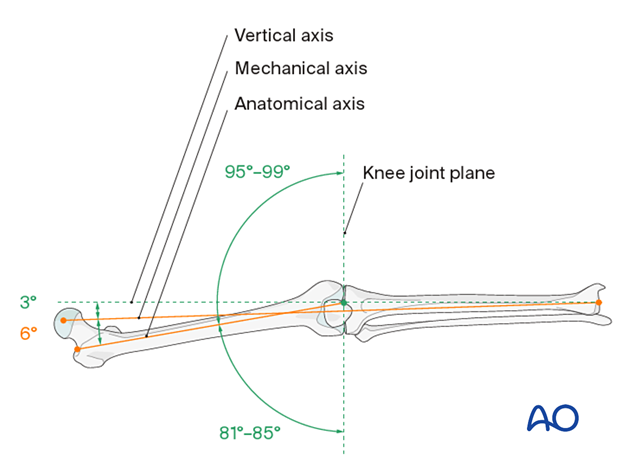
It is very important to restore the biomechanical axis of the lower limb. The normal biomechanical axis follows a line from the center of the femoral head, through the center of the proximal tibia and then through the center of the ankle joint. This axis can be checked intraoperatively by using a piece of cable, such as the diathermy cord. The cord is stretched from the iliac spine across the patella to the cleft between the first and second toes.
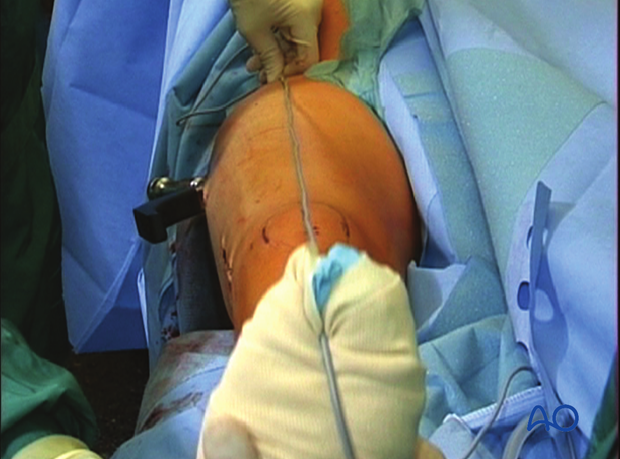
If rotation is correct, this cord will pass over the midline of the patella, and slightly medial to the tibial eminence. The radiological landmarks of the center of the femoral head, the center of the knee and the center of the ankle joint should all be in line if the mechanical axis of the femur is correct.
Another method of assessing rotational reduction is to compare the cortical thickness above and below the fracture. If a shaft fracture is multifragmentary, the image intensifier cannot be used to compare cortical diameters on each side of the fracture.
Not only must the biomechanical axis be restored, but care should be taken to ensure that there is no malrotation of the distal femur on the proximal femur.
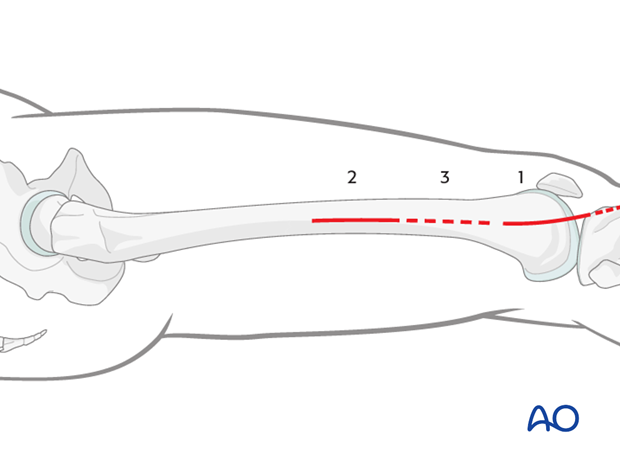
This illustration shows the longitudinal axes of the lower limb.
Confirmation of length
To ensure that femoral length has been restored, many options exist:
- One option involves reducing the fracture fragments anatomically, either directly or indirectly with fluoroscopic control.
- Even in multifragmentary fractures, there are usually a few main fracture segments that can assist the surgeon in ensuring that the appropriate length has been obtained.
- Another option involves taking radiographic images of the contralateral distal femur for comparison.
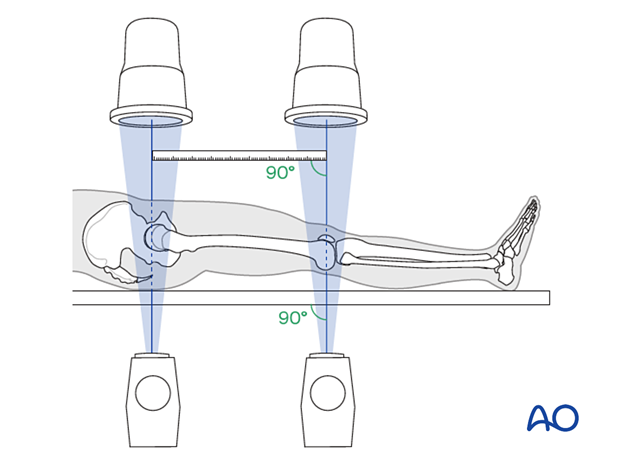
- A radiographic ruler can be used to measure the length of both femora. In this technique, it is important that the x-ray beams are perpendicular to the OR table and that the ruler is parallel to the OR table.
4. DCS fixation to the distal fragment
Preparation for correct positioning
Determine the correct position for the DCS with the help of guide wires around the joint. Under image intensifier control, pass one guide wire lateral to medial along the tibio-femoral joint line (red). Pass a second guide wire over the anterior surface of the knee to indicate the plane of the patello-femoral condyles (green).
The ideal position of the DCS is shown by the yellow wire. Note that it is inserted parallel to both the red wire in the frontal plane and is parallel to the green line on the end-on view on the femur. This latter orientation ensures that the plate comes to lie flush with the lateral cortex.
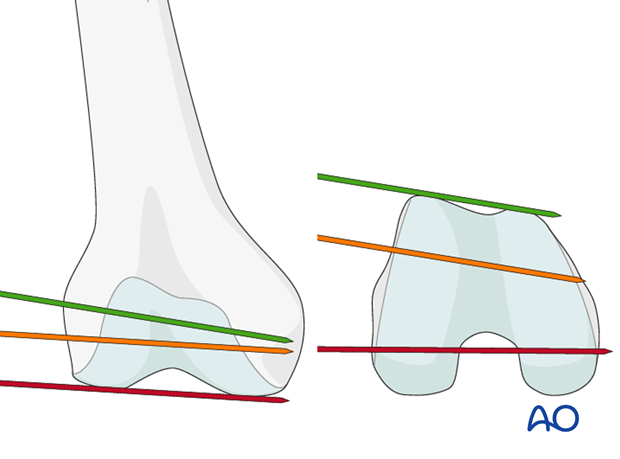
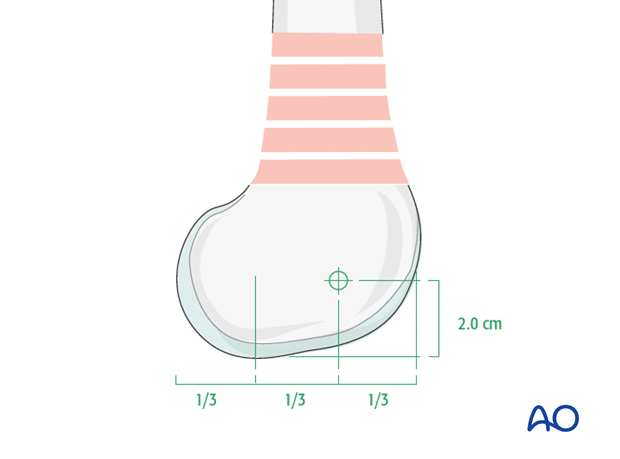
The ideal entry point for the DCS is shown on the diagram. The guide wire for the DCS is positioned at 2 cm proximal to the distal end of femur. On the lateral view, the distal femur is divided into thirds and the DCS entry site is located at the junction of the anterior and middle thirds.
Insert the guide wire at the chosen entry site of the DCS. Insert the guide wire under image intensifier control all the way across the femur. Check the position of the guide wire carefully to ensure it has been correctly positioned, with the parallelism already described.
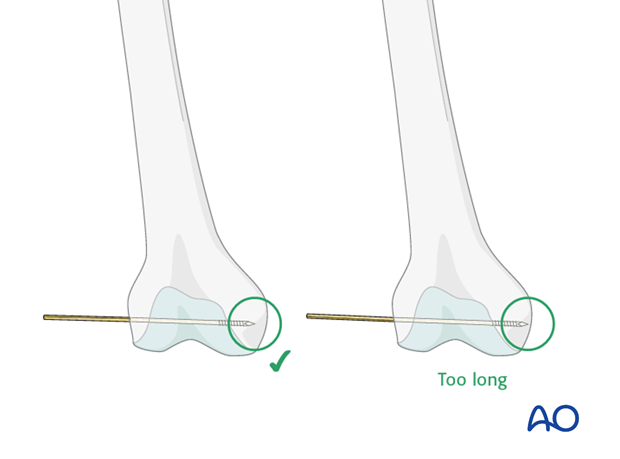
Correct depth of guide-wire insertion
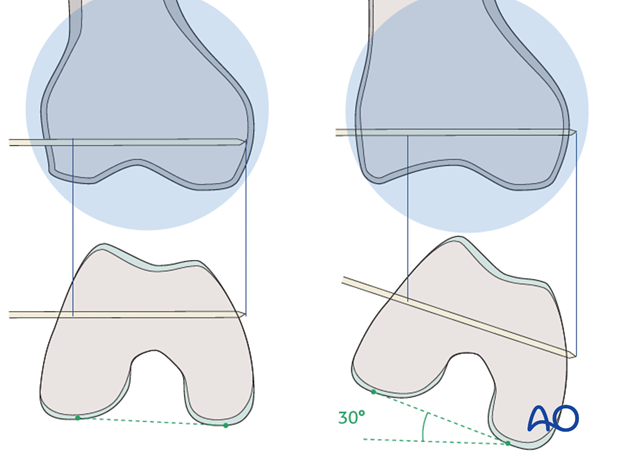
The depth of guide-wire insertion is crucial. Remember that the cross section of the distal femoral condylar mass is trapezoidal and slopes markedly on the medial side. The tip of the guide wire should just engage the medial cortex, and so will appear short of the medial condylar cortex on the AP intensifier image.
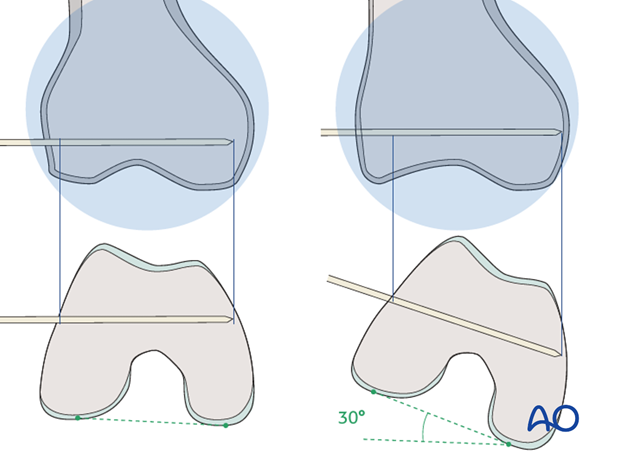
In this illustration, internal rotation by 30° reveals that the guide wire length was chosen inappropriately.
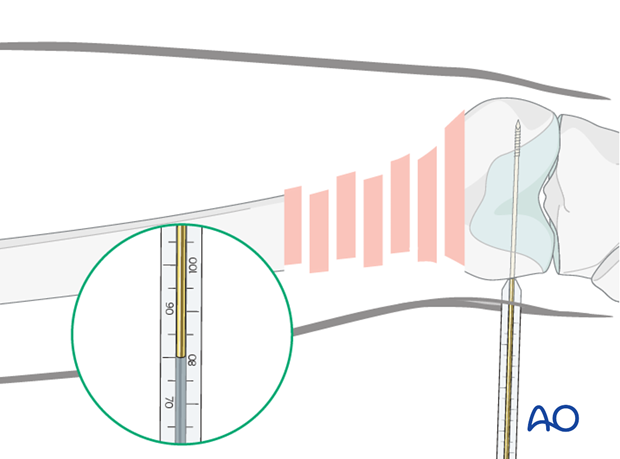
Screw length measurement
Next, slide the direct measuring device over the guide wire and determine guide-wire insertion depth and, thereby, the length of the DCS required.
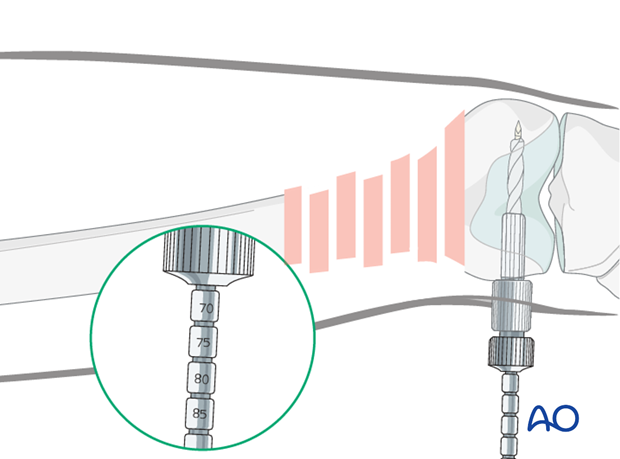
Reaming
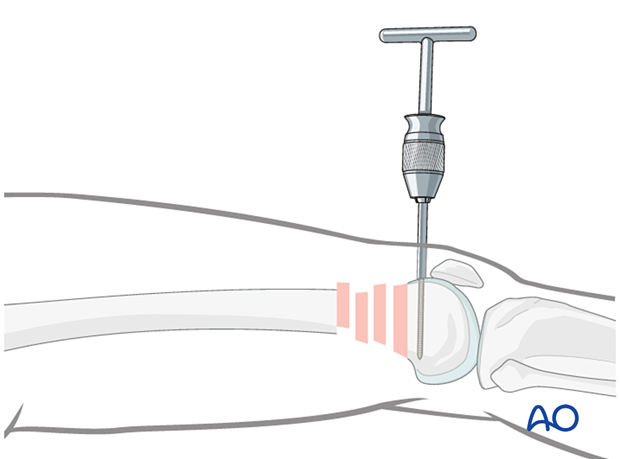
After assembling the DCS triple reamer and setting the reamer to the correct depth, ream the hole for the DCS over the guide wire.
DCS insertion
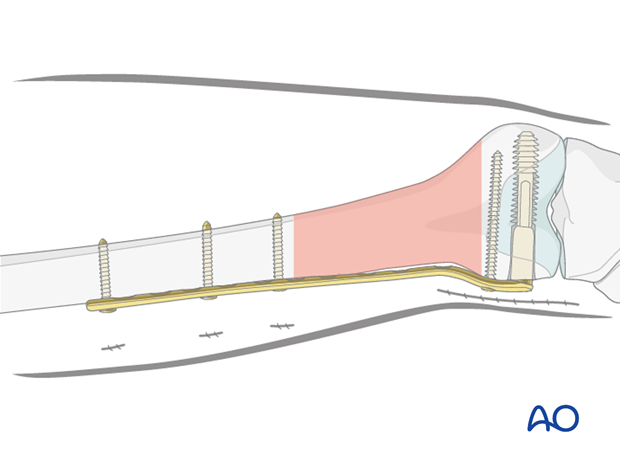
After tapping, insert the DCS over the guidewire, so that its outer end is still visible 2-3 mm outside the lateral cortex of the distal femur.
For the plate barrel to slide over the screw, the T-handle should be parallel, on the lateral view, to the long axis of the distal fragment.
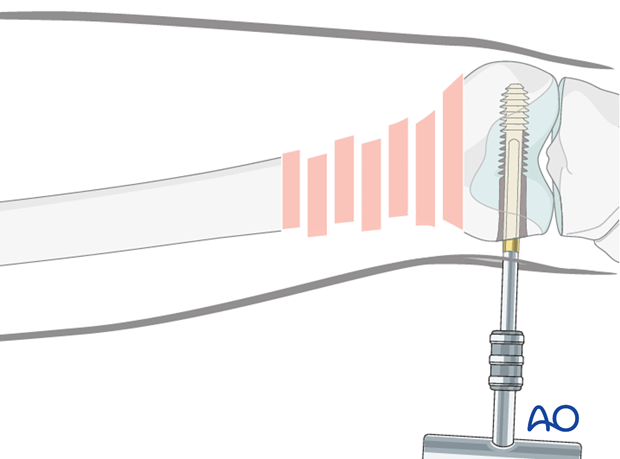
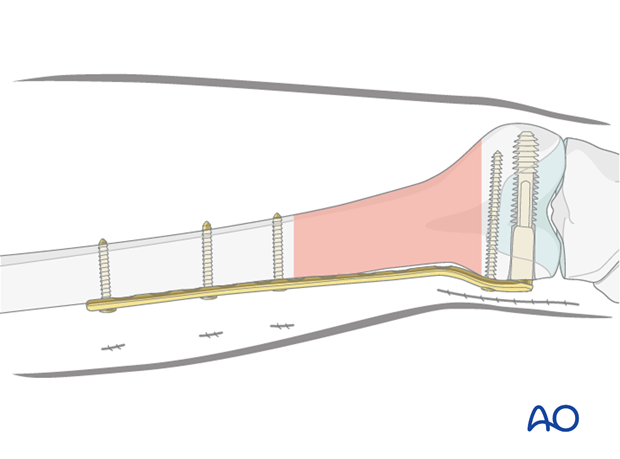
Plate insertion
Detach the T-handle and pass the plate barrel over the screw shank.
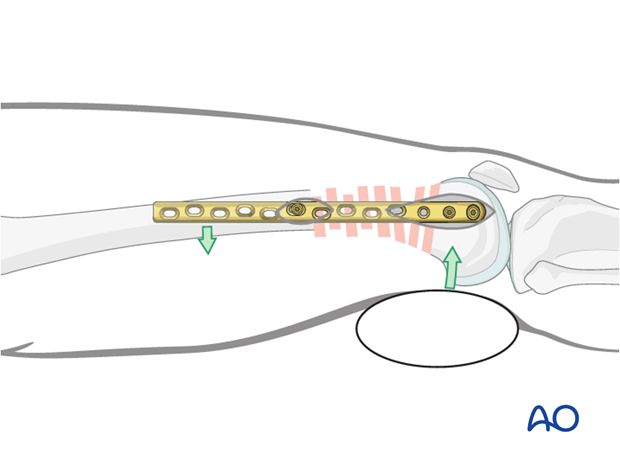
The plate is pushed from distal to proximal beneath the vastus lateralis. If there is a continuous contact of the plate tip with the bone while pushing it proximally, there is no need preliminarily to create a tunnel.
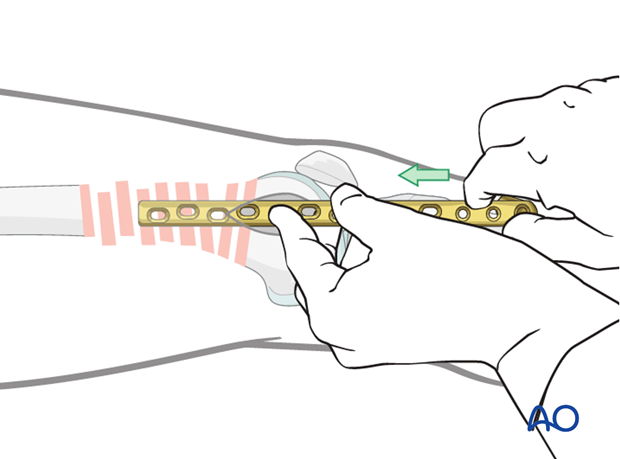
Plate and screw combination
Insert the T-handle through the barrel of the plate and reconnect it to the screw. This can be challenging and may temporarily tilt the distal femoral articular block. It may be helpful to make an incision over the proximal end of the plate at this point to gain control of both ends of the plate. This will allow for easier connection of the plate to the screw.
For the barrel to slide over the screw the T-handle should be parallel, on the lateral view, to the long axis of the distal fragment.
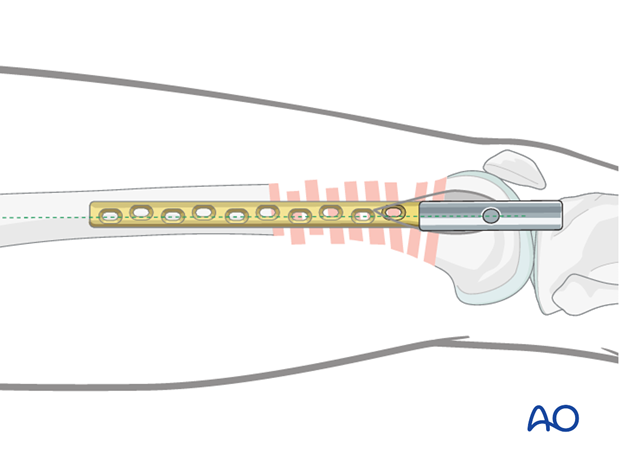
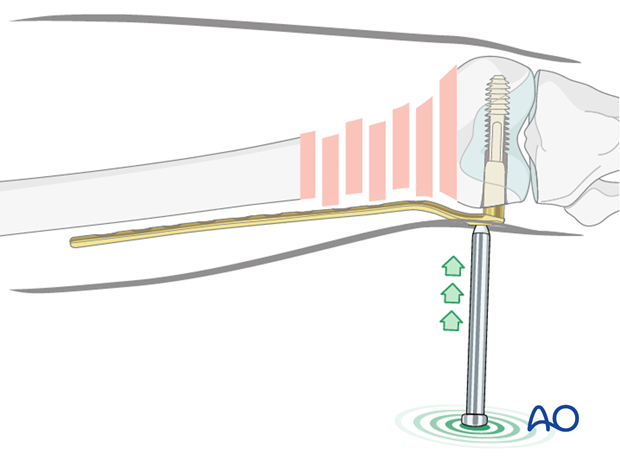
Plate impaction
Disconnect the T-handle from the screw.
Use the impactor to bring the plate down to the bone with the barrel sliding over the screw shank.
The compression screw may be used to couple the DCS to the plate.
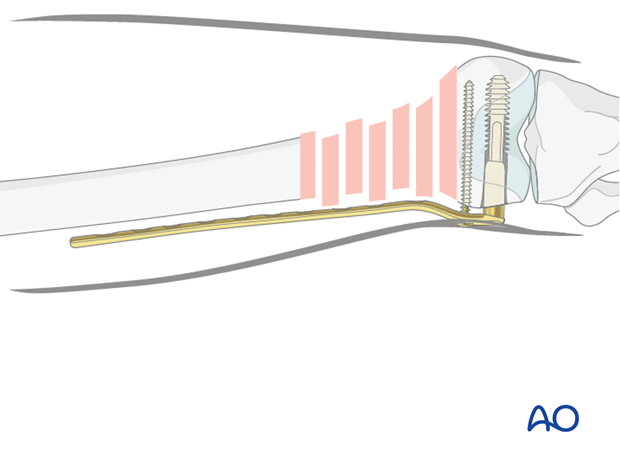
Final screw placement in distal fragment
A cancellous screw can then be inserted into the most distal screw hole of the plate to prevent rotation of the distal femoral articular block around the axis of the DCS.
5. Plate fixation to the proximal fragment
Final reduction of metaphysis
Fragmentary fracturesPrior to plate fixation to the proximal fragment, restore the mechanical axis of the femur in all planes using the previously discussed techniques.
Anatomical reduction of all fracture segments is not desired. If the mechanical axis is restored this should be adequate in most situations.
Under image intensifier control, the preliminary reduction is checked again with respect to axial alignment, length and, rotation.

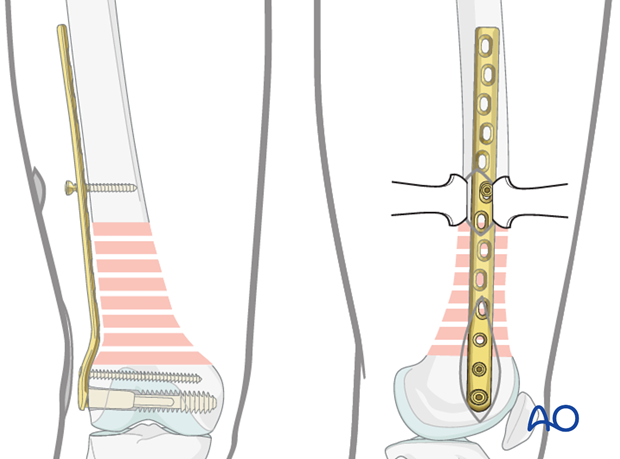
Insertion of first screw into proximal fragment
Make stab incisions over the proximal fragment according to the planned final screw placement.
Control the mid-lateral plate position using two blunt Hohmann retractors placed ventrally and dorsally around the femoral shaft.
If the overall reduction is found to be satisfactory, insert the first cortical screw in the distal part of the proximal main fragment, without fully tightening. This still allows for the plate position to be finely tuned.
If the lateral position prior to the insertion of the second screw is inadequate, use sterile bolsters to aid correction.
Be cautious not to malalign the articular block as this will make application of the plate to the proximal femur difficult.
Insertion of second screw into proximal fragment
Confirm the mid-lateral plate position using two Hohmann retractors introduced through a second incision over the proximal plate portion, or by palpation.
Once the most proximal screw is fully inserted, the more distal screw in the proximal fragment is finally tightened.
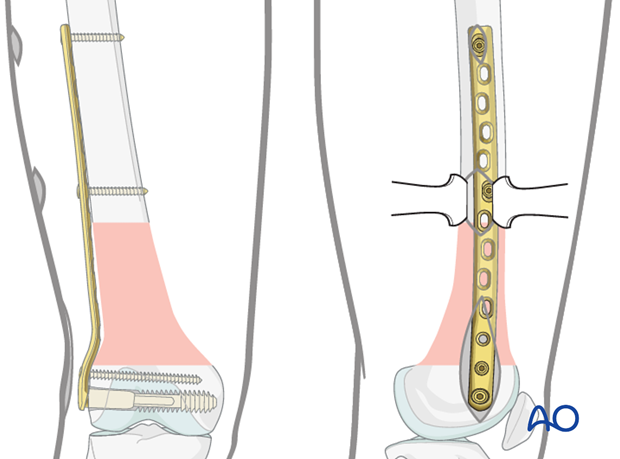
Further insertion of proximal screws
According to preoperative planning, insert additional screws into the distal and proximal main fragments.
6. Aftercare
Impediments to the restoration of full knee function after distal femoral fracture are fibrosis and adhesion of injured soft tissues around the metaphyseal fracture zone, joint capsular scarring, intra-articular adhesions, and muscle weakness.
Early range of motion helps restore movement in the early postoperative phase. With stable fracture fixation, the surgeon and the physical therapy staff will design an individual program of progressive rehabilitation for each patient.
The regimens suggested here are for guidance only and not to be regarded as prescriptive.
Functional treatment
Unless there are other injuries or complications, knee mobilization may be started immediately postoperatively. Both active and passive motion of the knee and hip can be initiated immediately postoperatively. Emphasis should be placed on progressive quadriceps strengthening and straight leg raises. Static cycling without load, as well as firm passive range of motion exercises of the knee, allow the patient to regain optimal range of motion.
Weight bearing
Touch-down weight-bearing (10-15 kg) may be performed immediately with crutches, or a walker. This will be continued for 6-10 weeks postoperatively. This is mostly to protect the articular component of the injury, rather than the shaft injury. Touch-down weight-bearing progresses to full weight-bearing gradually, over a period of 2 to 3 weeks (beginning at 6–10 weeks postoperatively). Ideally, patients are fully weight-bearing, without devices (e.g., cane) by 12 weeks.
Follow-up
Wound healing should be assessed at two to three weeks postoperatively. Subsequently 6-week, 12-week, 6-month, and 12-month follow-ups are usually made. Serial x-rays allow the surgeon to assess the healing of the fracture.
Implant removal
Implant removal is not essential but should be discussed with the patient if there are implant-related symptoms after consolidated fracture healing.
Thrombo-embolic prophylaxis
Thrombo-prophylaxis should be given according to local treatment guidelines.













