Antegrade screw fixation of a scaphoid fracture
1. General considerations
Introduction
For the fixation of waist or proximal pole fractures of the scaphoid, headless compression screws (2.4 or 3.0 mm) may be used in an antegrade fashion.
In this basic technique, associated bony and ligamentous injuries are not shown for clarity.
Choice of implant
If the proximal pole fragment is larger than 5 mm, a cannulated, headless, self-compressing screw (2.4 or 3.0 mm) is the implant of choice.
For smaller proximal pole fragments, the use of a mini headless bone screw is advisable.
K-wires may be a better option for fixation of very small fragments (flakes).
Scapholunate ligament reattachment
If a bony avulsion fracture of the scapholunate ligament from the scaphoid is present, fixing the fragment, either with K-wires, or a small screw (1.5 mm), is necessary.
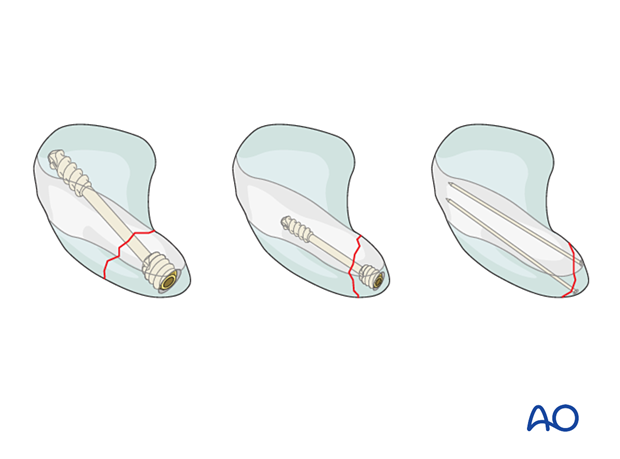
Comminuted scaphoid fractures
Unlike the treatment of an isolated comminuted scaphoid fracture, an associated scaphoid fracture should be approached through the same dorsal approach as the other injuries.
In such a case, adding a K-wire or a second screw may help improve fracture stabilization.
Anatomical considerations
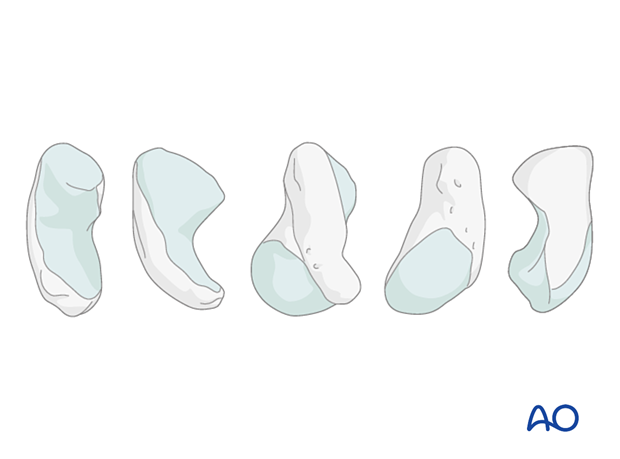
80% of the surface of the scaphoid is covered with articular cartilage. This greatly limits potential points of entry for fixation devices.
An additional constraint is the curved shape of the scaphoid.
This means that a wire or fixation device along the true central axis of the scaphoid is not possible from a palmar approach. Occasionally, access to a distal entry point for a device can only be gained by a limited excavation of the edge of the trapezium.
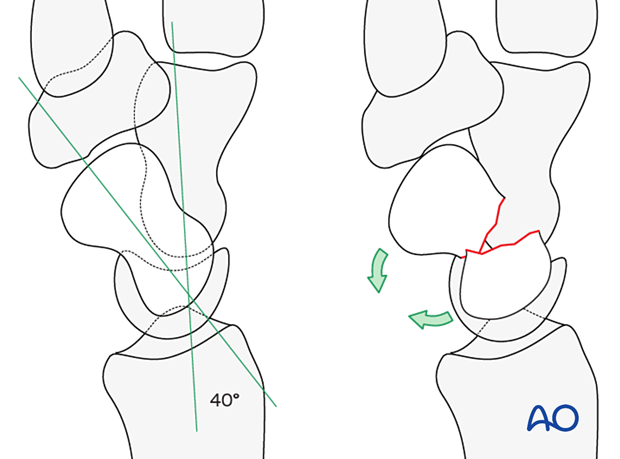
Fracture displacement forces
In displaced fractures of the waist of the scaphoid, the distal pole tends to rotate into flexion in relation to the proximal pole, the lunate, and the triquetrum, which lie in extension. This can create a rotational and angular deformity at the fracture site – the so-called “humpback deformity.”
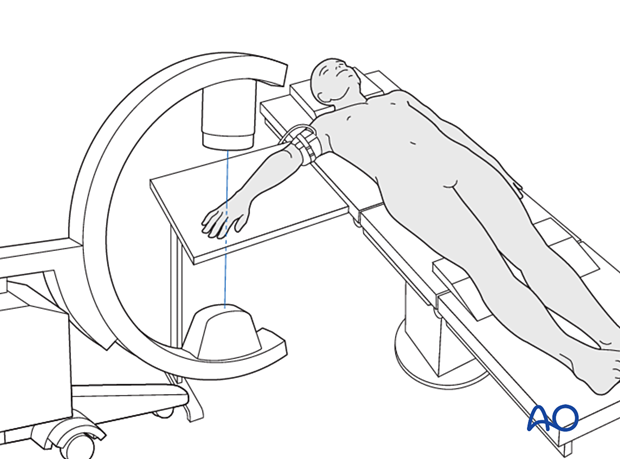
Preoperative planning
Conventional radiographs do not adequately demonstrate the complete fracture configuration. A CT scan is recommended to reveal the degree of displacement.
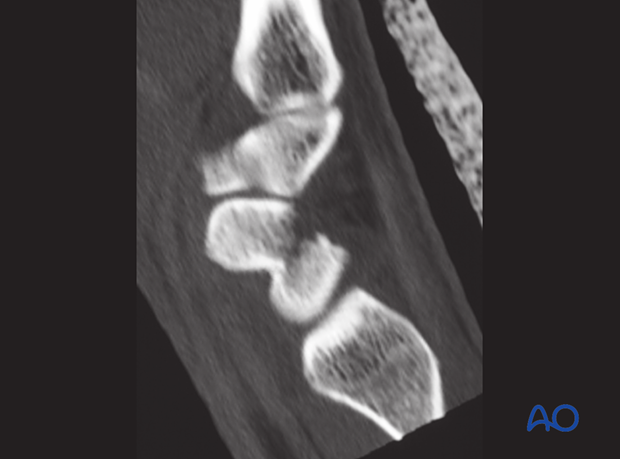
Before starting the surgical procedure, reexamine the fracture pattern under the image intensifier. Ensure the fracture is suitable for a percutaneous technique and that no secondary displacement has occurred. This is especially indicated for displaced or oblique fractures.
2. Reduction
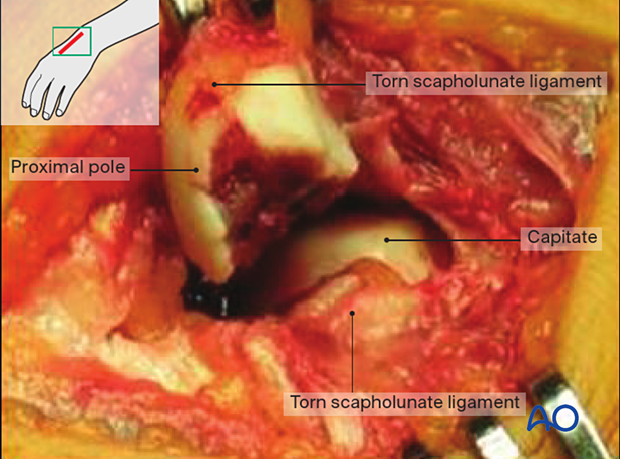
Inspection of the fracture
Look for additional lesions, especially scapholunate ligament ruptures.
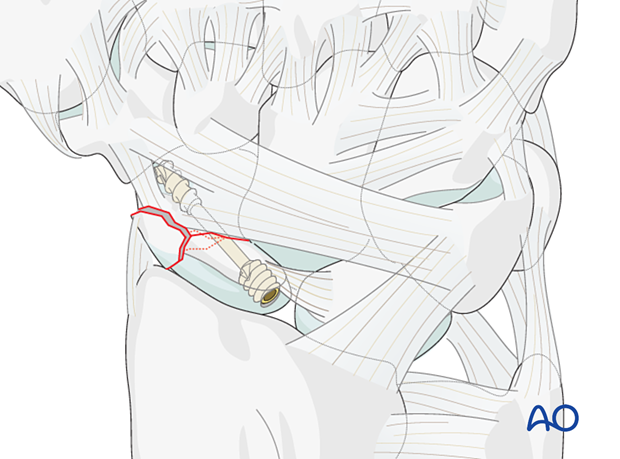
The picture shows a proximal pole fracture combined with a complete scapholunate rupture. The head of the capitate is visible deeper in the wound. The proximal pole fragment has been delivered into the wound and has no soft-tissue attachments to the remaining carpus. Its vitality is therefore in question.
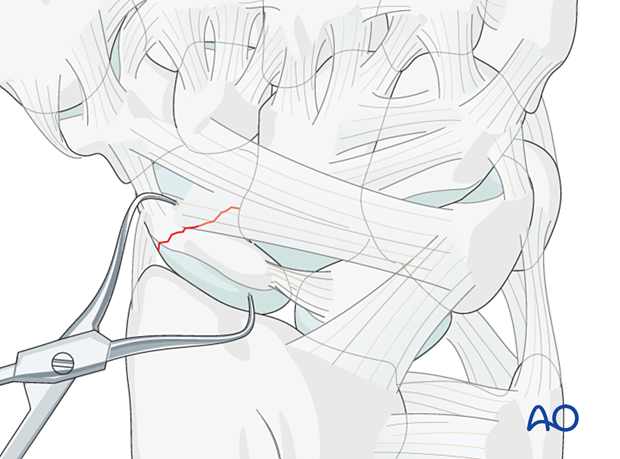
Reduction
If the fracture is displaced, reduce it with small pointed reduction forceps.
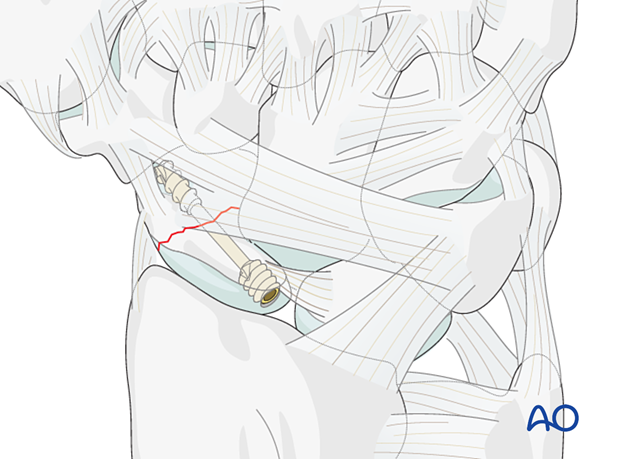
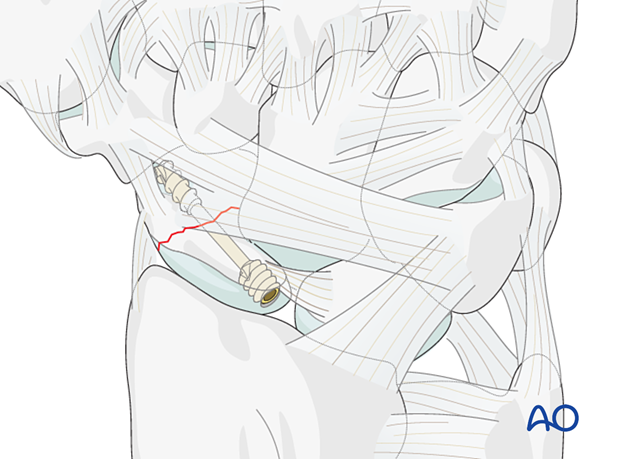
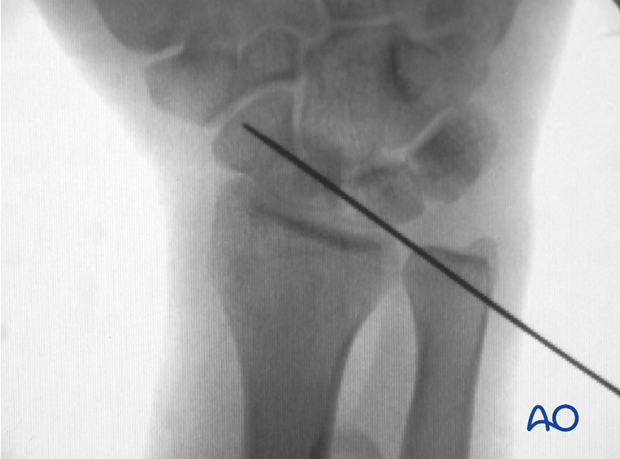
3. Guide-wire insertion
The entry point is at the proximal pole, directly adjacent to the scapholunate ligament insertion.
Insert the guide wire in the axis of the shaft of the first metacarpal, in radial abduction.
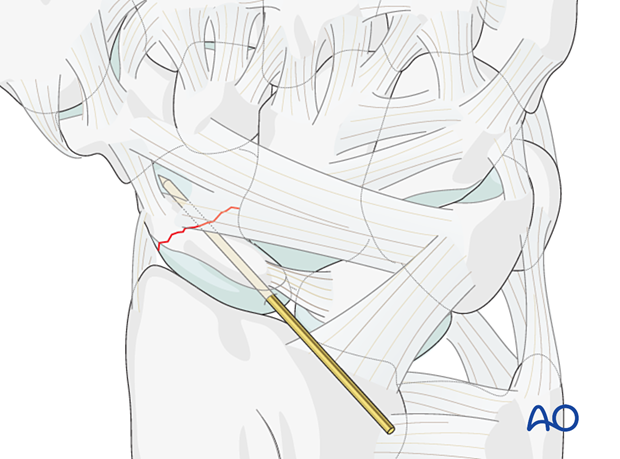
Confirm accurate advancement of the guide wire in the scaphoid axis with an image intensifier in at least two planes and perpendicular to the fracture plane.
Do not penetrate the scaphotrapezial joint with the guide wire.
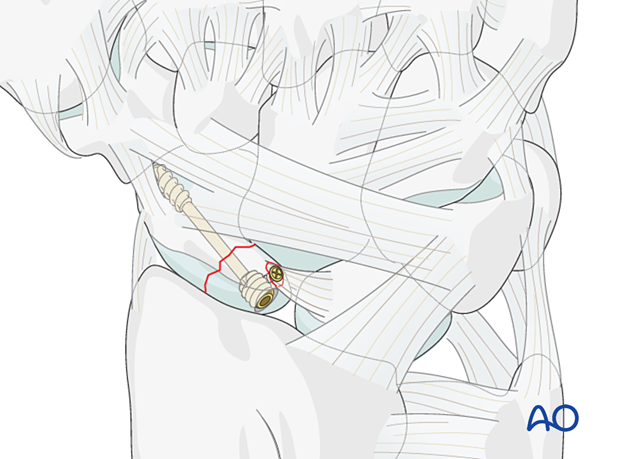
4. Screw insertion
Insert the headless compression screw in a standard manner.
Select a screw 2–4 mm shorter than the measured length with the appropriate thread length. In most cases, a 16–20 mm cannulated screw is the appropriate length.
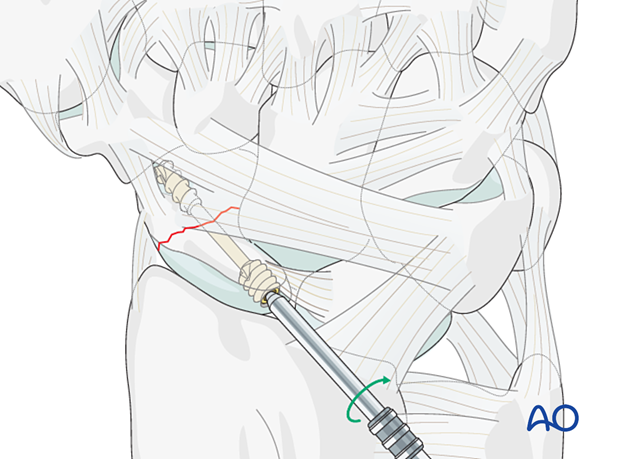
Confirming screw position
Check the final position of the screw and the scaphoid stability with an image intensifier.