Minimally-invasive (semi-closed) treatment
1. Principles
In rare situations, a simple noncomminuted zygomatic complex fracture can snap into a perfect reduction with closed manipulation and appear to be very stable. In such circumstances, a surgeon may choose to omit fixation. In these cases, intraoperative imaging must be used to confirm correct anatomical reduction.
2. Computer assisted surgery
Computer assisted surgery (CAS) has greatly improved the management of craniomaxillofacial trauma. Whenever an intraoperative CT scanner is available, an intraoperative scan should be obtained for intraoperative evaluation of the reduction.
Read more about CAS here.
3. Zygoma reduction methods
A percutaneous hook is placed through a small incision in the skin.
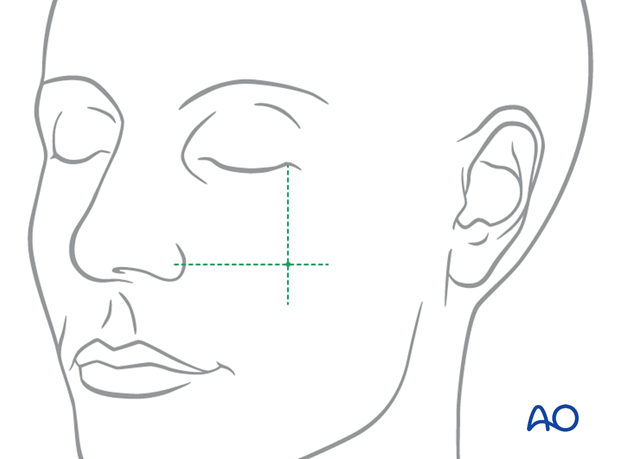
Two intersecting lines are drawn on the face to determine the proper location for applying the bone hook. The first line is vertical, dropped down from the lateral cantus of the eye (on the involved fracture side).
The second line is horizontal, drawn laterally from the ala of the nose.
The zygomatic complex fracture may be reduced using a percutaneous technique.
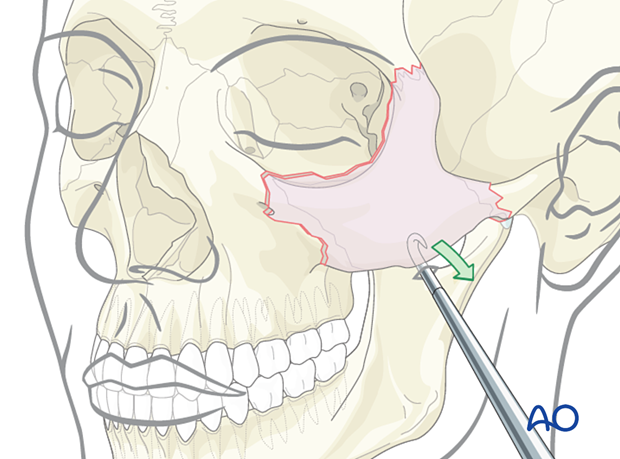
The zygomatic complex fracture may also be reduced with an intraoral approach using an elevator placed underneath the malar eminence. The force should be directed anteriorly and laterally.
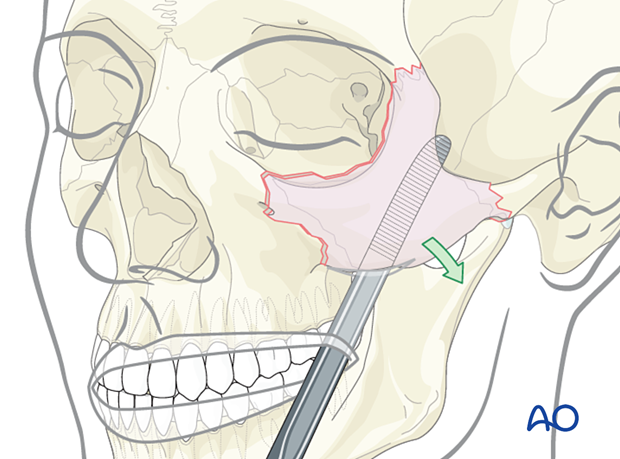
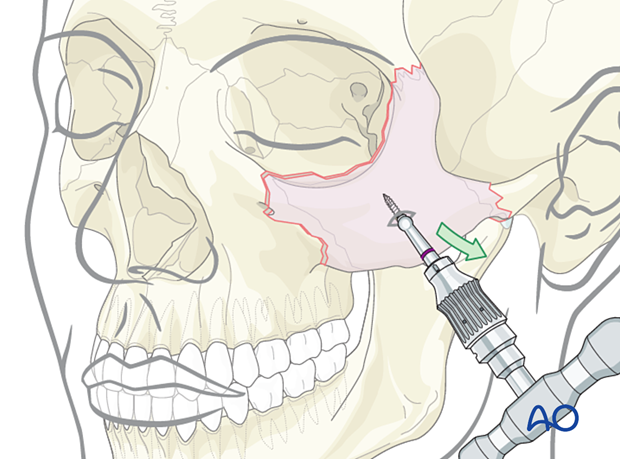
Screw and traction
A percutaneous or intraoral approach may be used to place a screw into the zygomatic body. The screw will help to manipulate the segment using a heavy needle holder.
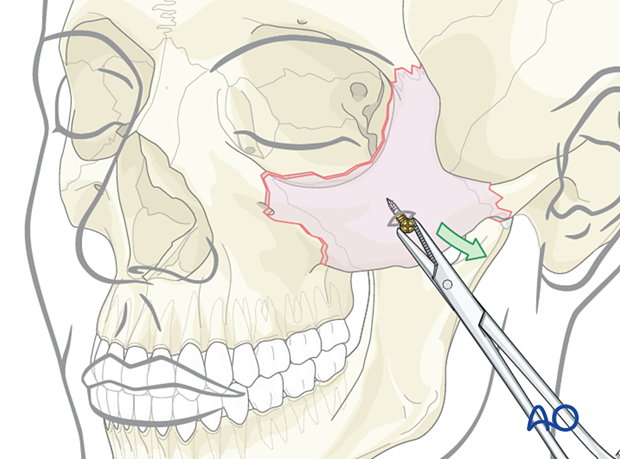
Threaded reduction tool
A threaded reduction tool (Carroll-Girard screw) is inserted either percutaneously or intraorally into the body of the zygoma and used for reduction.
4. Aftercare
Patient vision is evaluated after awakening from anesthesia and then at appropriate intervals.
A swinging flashlight test may serve the same function in the unconscious or noncooperative patient. In some centers, an electrophysiological examination can be utilized if the appropriate equipment is available (VEP).
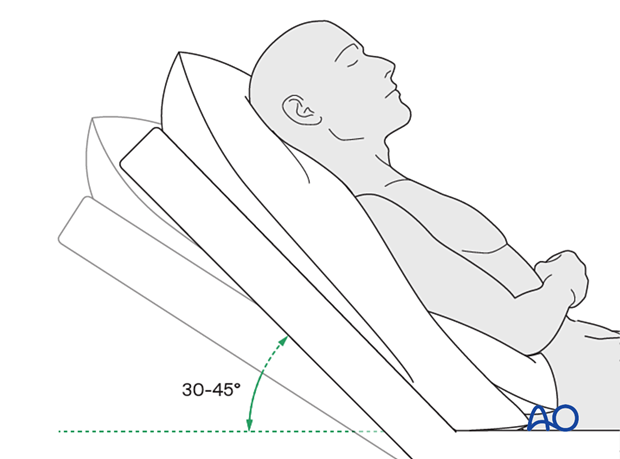
Postoperative positioning
Keeping the patient’s head in a raised position both preoperatively and postoperatively may significantly reduce edema and pain.
The patient is instructed to protect the zygomatic reduction from excessive pressure or further injury for at least 2–3 weeks postoperatively. This applies to fractures that have been reduced but not stabilized with fixation. A convenient method is to put two pillows beside the patient so that displacement of the reduced fracture can be prevented.

Nose blowing
Nose blowing should not involve pressing on the sides of the nose to increase intranasal pressure. Finger pressure on the nose should not accompany nose blowing for at least two weeks following orbital fracture repair to minimize the chance of orbital emphysema.
Medication
The use of the following perioperative medication is controversial. There is little evidence to make strong recommendations for postoperative care.
- No aspirin or nonsteroidal anti-inflammatory drugs (NSAIDs) for seven days
- Analgesia as necessary
- Antibiotics (Many surgeons use perioperative antibiotics. There is no clear advantage beyond perioperative antibiotics, unless fracture repair has been delayed and there is maxillary sinus obstruction. Here the duration of treatment is dependent upon the circumstances.)
- Regular perioral and oral wound care must include disinfectant mouth rinse, lip care, etc.
Ophthalmological examination
Postoperative examination by an ophthalmologist may be requested if indicated. The following signs and symptoms are usually evaluated:
- Vision
- Extraocular motion (motility)
- Diplopia
- Globe position
- Perimetric examination
- Lid position
- If the patient complains of epiphora (tear overflow), the lacrimal duct must be checked
Postoperative imaging
Postoperative imaging should be performed within the first days after surgery. 3D imaging (CT, cone beam) is recommended to assess complex fracture reductions. An exception may be made for centers capable of intraoperative imaging.
Diet
Diet depends on the fracture pattern.
A soft diet can be taken as tolerated until there has been adequate healing of the maxillary vestibular incision.
Nasogastric feeding may be considered in cases with oral bone exposure and soft-tissue defects.
Patients in MMF will remain on a liquid diet until the MMF is released.
Clinical follow-up
Routine clinical follow-up should be performed.
Issues to consider are:
- Facial deformity (including asymmetry)
- Sensory nerve compromise
- Problems of scar formation
Oral hygiene
Tooth brushing and mouth washes should be prescribed and used at least twice a day to help sanitize the mouth. Gently brushing the teeth occurs with a soft toothbrush (dipped in warm water to make the bristles softer).













