Closed treatment
1. Splint application
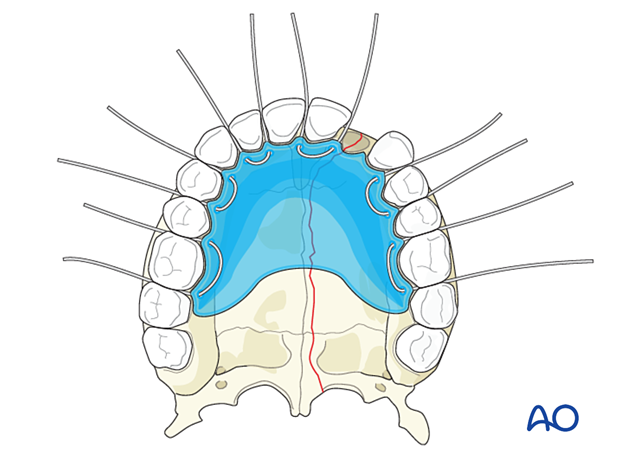
In complex (comminuted) palatal fractures where the tooth-bone units are relatively intact, most surgeons consider it essential to utilize a palatal splint. In these cases, different creation options exist:
- From dental impressions
- From CT DICOM data and intraoral scanners
- Using a complete digital flow
Reduction of a palatal fracture can be made with or without the use of a palatal splint. If the tooth-bone units are severely damaged or comminuted, a palatal splint alone may be insufficient.
The final objective is to get an accurate model from the patient’s maxillary and mandibular arches to perform model surgery and fabricate a palatal splint.
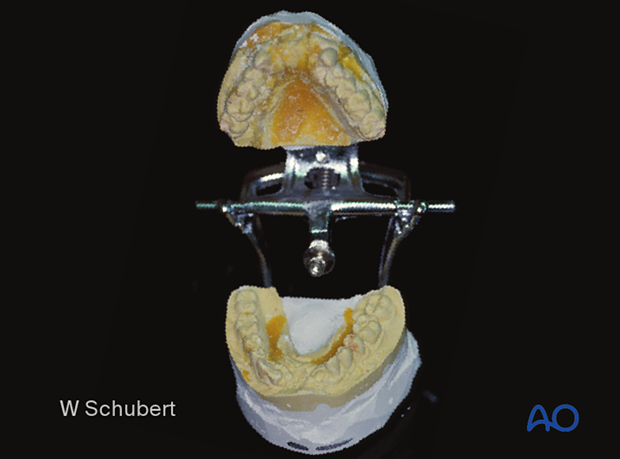
Dental impression
In the photographs, dental impressions have been taken, and gypsum models have been made.
This procedure is not a simple task; it is painful and challenging to get a dental impression from a traumatized patient.
The impression is usually still in malposition and must be sectioned with model surgery and repositioned in an anatomically correct alignment.
Dental model scans taken with an extraoral (tabletop) scanner
A cast model is obtained from an upper jaw impression.
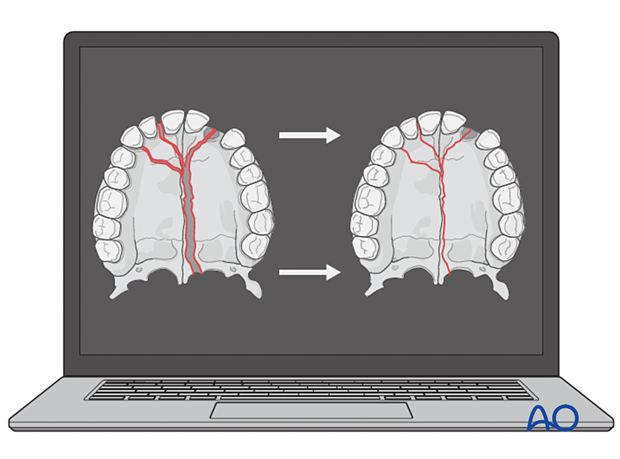
An extraoral tabletop scan is performed and imported into special software to manipulate it.
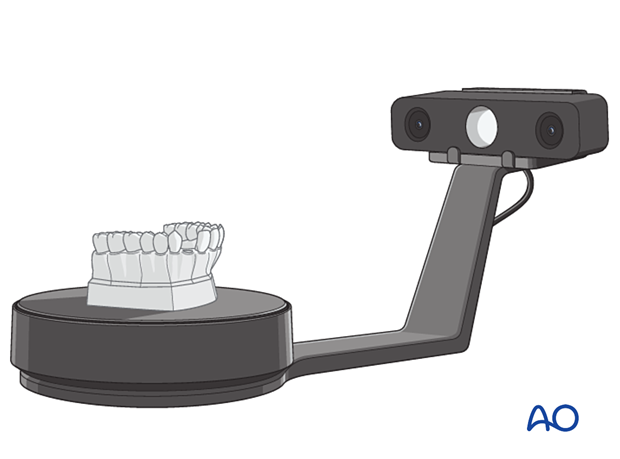
The virtual surgery is performed, realigning the segments, and checking the maxilla and its relationship with the mandibular dentition.
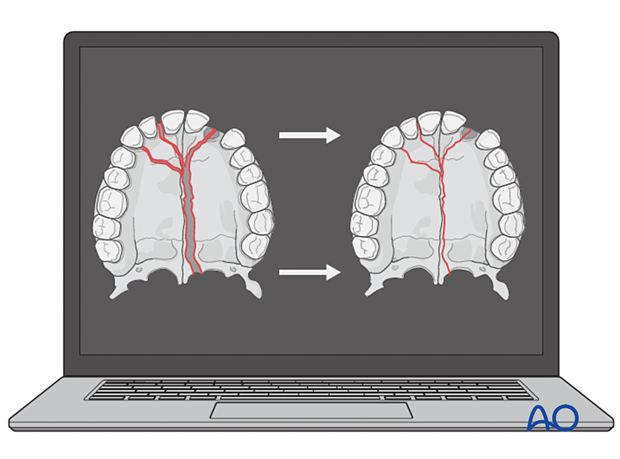
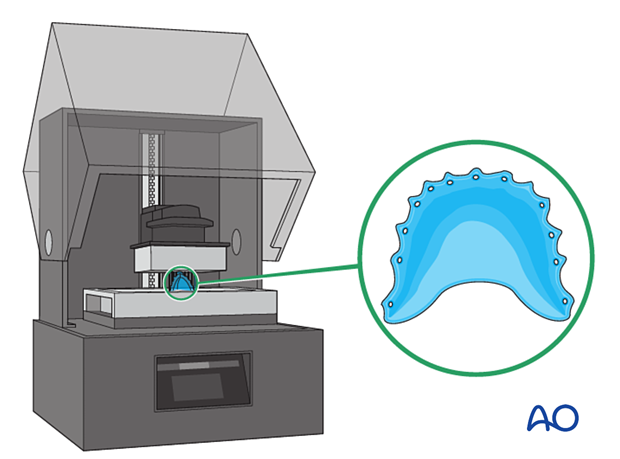
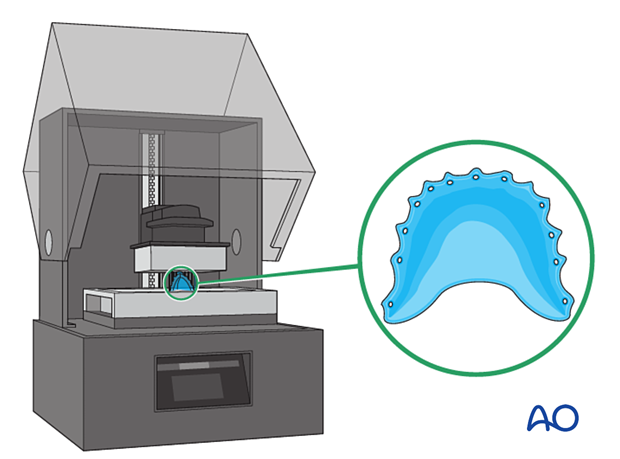
A palatal splint is designed (CADCAM) and printed with a 3D printer.
Complete digital flow
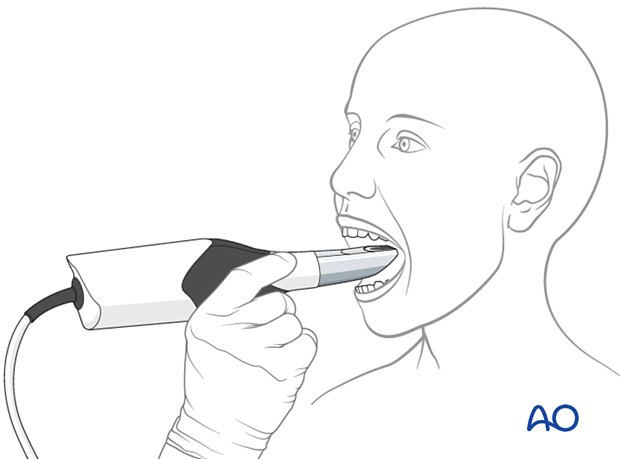
The virtual surgery is performed by realigning the segments and checking the maxilla and its relationship to the mandibular dentition.
A palatal splint is designed (CADCAM) and printed with a 3D printer.
A 3D printed model of the patient’s maxilla can also be printed to visualize all the structures that need to be fixed.
Palatal splint
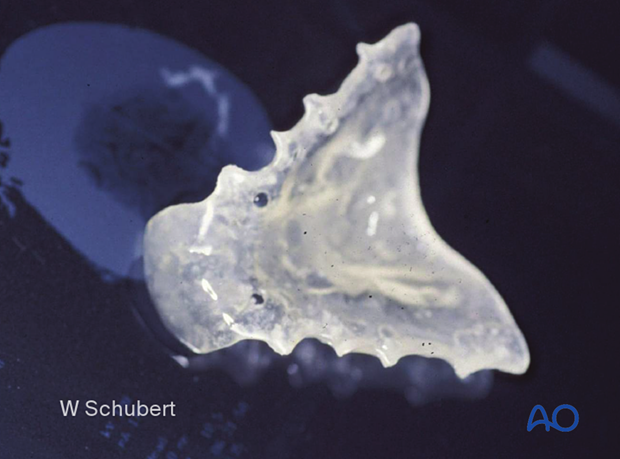
A palatal splint can be fabricated in plastic (methyl methacrylate (MMA)) material or 3D printed using a sterilizable polymer.
2. Palatal splint fixation and reduction
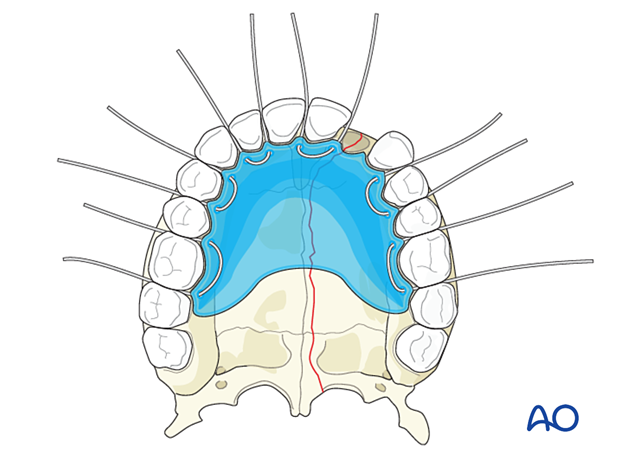
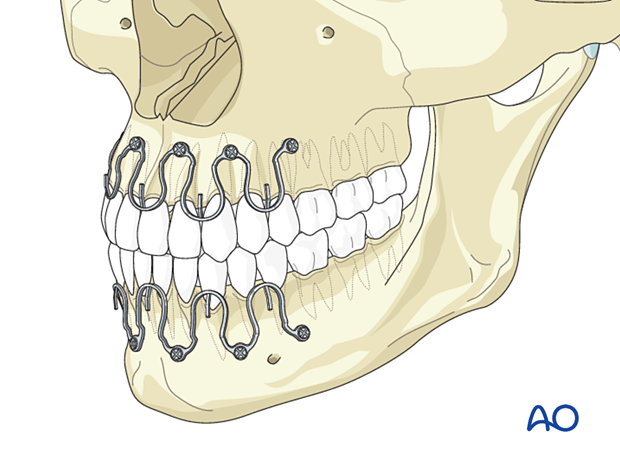
The palatal splint is then wired to the patient's dentition using circumdental wiring, possibly also using arch bars.
The surgeon may choose to leave the patient in postoperative MMF depending on the palatal unit’s stability, the postoperative airway status, or any complicating issues of other midface fractures.
Closed treatment of complex palatoalveolar injuries preserves the blood supply of the comminuted segments.
Perform reduction by applying pressure laterally on the two maxillary segments to reduce the splayed fracture. The maneuver needs to be performed while the palatal splint is in place, as it offers the best guide to verify adequate reduction. It may be necessary to continue this pressure while applying the arch bars.
Depending on the degree of dentoalveolar trauma, one may not be able to use a palatal splint.
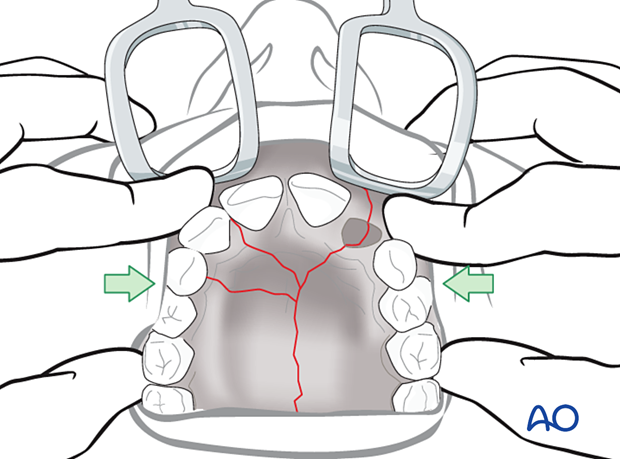
In this photograph, the palatal splint has been inserted and secured to the dentition using circumdental wires and an arch bar.
Existing dental models from previous treatments may be helpful in reestablishing the pre-injury anatomy.

Option: hybrid arch bars
You can choose between traditional arch bars or hybrid arch bars.
Hybrid arch bars use a screw to fix the arch bar to the bone, making the procedure faster.
When choosing to use hybrid arch bars the palatal splint is secured using circumdental wire independent of the hybrid arch bar.
3. Aftercare
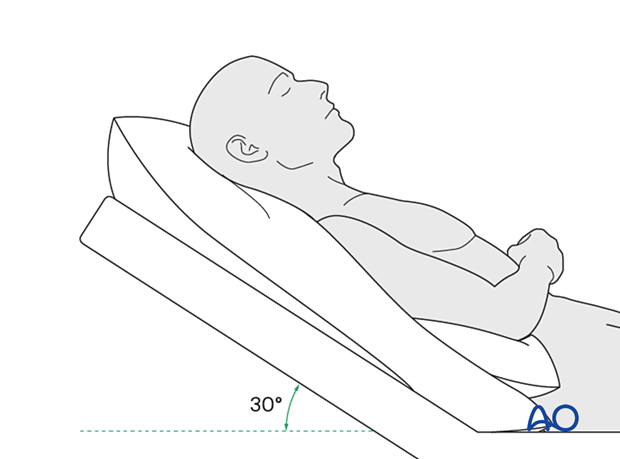
Postoperative positioning
Keeping the patient’s head in an upright position both preoperatively and postoperatively may significantly reduce periorbital edema and pain.
Medication
The following medications may be used:
- Analgesia as necessary (no aspirin or nonsteroidal anti-inflammatory drugs (NSAIDs) for seven days)
- In case of an open wound or exposed bone antibiotic coverage is indicated
- Regular perioral and oral wound care should include disinfectant mouth rinse, lip care, etc.
Postoperative imaging
Postoperative imaging should be performed within the first days after surgery. 3D imaging (CT, cone beam) is recommended to assess complex fracture reductions.
In fractures involving the alveolar area, orthopantomograms (OPG) are helpful.
Diet
Diet depends on the fracture pattern.
A soft (non-chew) diet can be taken as tolerated until there has been adequate healing (usually 4–6 weeks).
Patients in MMF will remain on a liquid diet until the MMF is released.
Clinical follow-up
Clinical follow-up depends on the complexity of the surgery and whether the patient has any postoperative problems.
Issues to consider with palatal fractures and alveolar ridge fractures include:
- Problems with dentition and dental sensation
- Problems with occlusion
- Problems with the temporomandibular joint (TMJ), such as reduced range of motion and pain
MMF
The need for and duration of MMF are very much dependent on:
- Fracture morphology
- Type and stability of fixation (including palatal splints)
- Dentition
- Coexistence of mandibular fractures
- Premorbid occlusion
Oral hygiene
Patients with arch bars, intraoral incisions, or wounds must be instructed about appropriate oral hygiene procedures. The presence of arch bars or elastics makes oral hygiene more complicated. A soft toothbrush (dipped in warm water to make it softer) should be used to clean the teeth and arch bars. Elastics are removed during oral hygiene procedures. Disinfectant mouth rinses (Chlorhexidine) should be prescribed and used at least three times a day to help sanitize the mouth.
For larger debris, a 1:1 mixture of hydrogen peroxide/Chlorhexidine can be used. The effervescent action of the hydrogen peroxide helps remove debris. A jet irrigator, (eg, Waterpik) is a handy tool to help remove debris from the wires. If used, care should be taken not to directly point the jet stream over intraoral incisions, which may lead to wound dehiscence.













