Observation
1. Indication
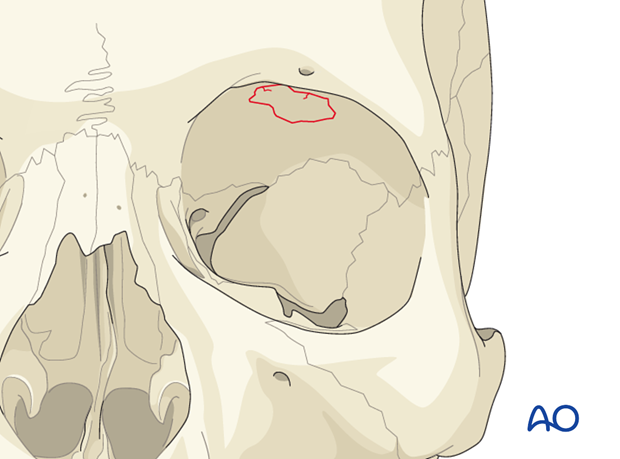
Observation is often indicated, especially if there is no effect on the orbital shape and volume, or displacement of the globe. Depending on accompanying lesions (eg, CSF leak, injury to the dura) of the adjacent tissues, specific treatment of these accompanying lesions may be necessary and should be addressed.
The decision to observe or to perform surgery is based on thorough evaluation because correction of a potential secondary deformity is challenging.
2. Follow-up
Due to displacement of the orbital roof and periorbital edema following trauma, the majority of patients may initially present with proptosis and inferior displacement of the globe.
The patient needs to be examined and reassessed regularly and often. Additionally, ophthalmological, and neurological/neurosurgical examination is recommended. If any clinical signs of meningitis or changes in mental status develop, professional help has to be sought quickly. A regular follow-up CT scan is recommended 3–6 months after the trauma to assure proper pneumatization of the sinuses (especially mucocele formation has to be ruled out), sealing of the skull base, and stability of fragment position.
Note: Posttrauma meningitis may occur even decades after trauma.
Information on retrobulbar hemmorage can be found here.
3. Aftercare
For aftercare and rehabilitation following observation please refer to your local protocol.












