Nasal septal hematoma drainage
1. General considerations
Trauma to the nasal septum may result in the development of a hematoma. The mucoperichondrium provides the vascular supply to the septal cartilage. Bleeding may lift the mucoperichondrium from the cartilage, creating a hematoma. Since the hematoma lifts the mucoperichondrium, the cartilage is deprived of the blood supply. If left untreated, this may result in cartilage necrosis with subsequent nasal dorsum depression (“saddle nose” deformity), or septal perforation.
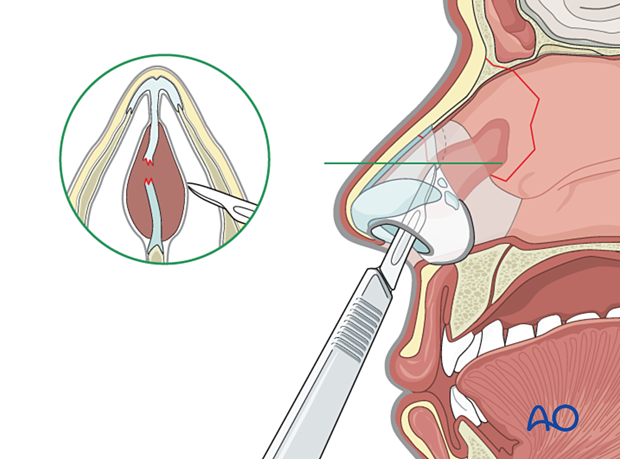
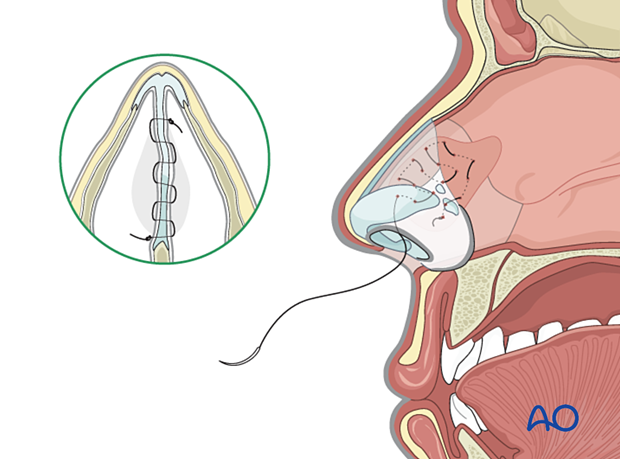
Treatment of septal hematoma is performed via small incisions through the mucoperichondrium to evacuate the blood. After the drainage, the nose is packed, or quilting stitches are placed. Silicone stents (Doyle) can also be used to prevent re-accumulation of the hematoma.
The quilting stitch is a running absorbable suture that goes back and forth across the septum to assure that the mucoperichondrium is pressed against the cartilage, thereby preventing the re-accumulation of blood.
Nasal packing is optional.
Alternative method: aspiration
The hematoma may be aspirated in the office using a needle and a syringe. If adequate drainage is accomplished, the nose is packed for a few days and rechecked at the time of package removal.
2. Aftercare
Postoperative positioning
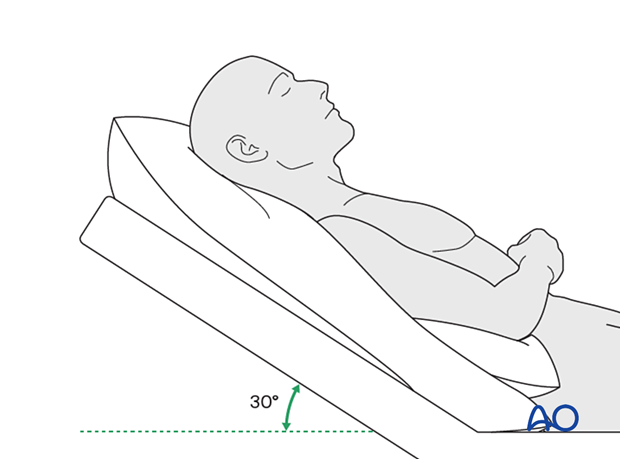
Keeping the patient’s head in a raised position both preoperatively and postoperatively may significantly reduce edema and pain.
Nose blowing
Nose blowing should be avoided for at least ten days following fracture repair to prevent orbital emphysema.
Medication
The use of the following perioperative medication is controversial. There is little evidence to make strong recommendations for postoperative care.
- No aspirin for seven days (nonsteroidal anti-inflammatory drugs (NSAIDs) use is controversial).
- Analgesia as necessary.
- Antibiotic ointment may be smeared over the Doyle splint or intranasal packing to retard infection.
- Oral antibiotics given as long as nasal packing is in place. Sepsis has occurred from tight nasal packing.
- A nasal decongestant may be helpful for symptomatic improvement in some patients.
Postoperative imaging
For nasal fractures, postoperative CT imaging is usually not necessary except in severely comminuted fractures.
Wound care
Ice packs are effective in the short term to minimize edema.
Avoid sun exposure and tanning to skin incisions for several months.
Diet
Diet depends on the fracture pattern and the patient’s condition, but there are usually no limitations.
Clinical follow-up
Clinical follow-up depends on the complexity of the surgery and the patient’s postoperative course.
In all patients with nasal bone trauma, all the following should be periodically assessed:
- Nasal airway status
- Excess compression from the splint or intranasal material
- External nasal deformity
Other issues to consider are:
- Facial deformity (including asymmetry)
- Sensory nerve compromise
- Problems of scar formation
- Anosmia
- Epiphora and dacryocystitis













