Closed treatment
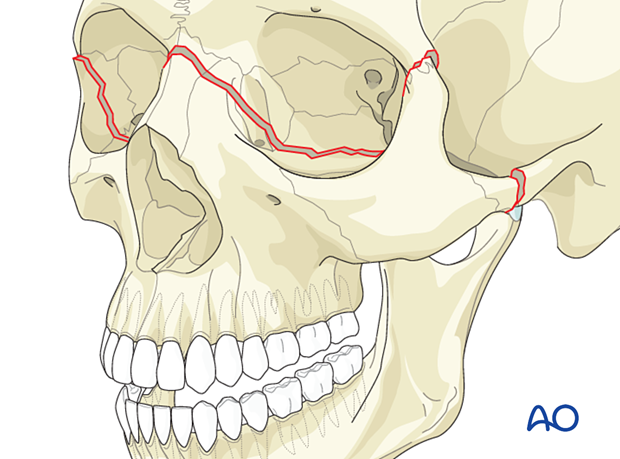
1. Indications
Fractures with minor malocclusion, readily correctable with maxillary disimpaction and manipulation, and not grossly mobile after repositioning, may be treated closed. These fractures are rare.
Patients with malocclusion who cannot have general anesthesia can be treated by applying arch bars and elastic traction.
A closed reduction of the midface may be part of an emergency treatment to stop bleeding or stop a CSF leak. Other options to control bleeding may include nasal packing or placement of a nasal balloon, and anterior and/or posterior packing. If these methods fail, embolization via interventional radiology may be required.
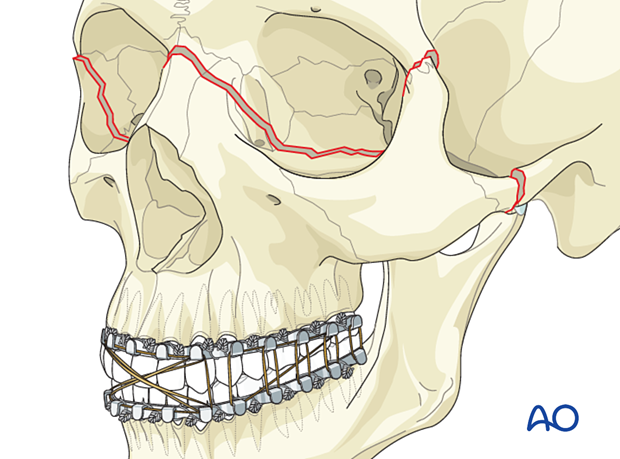
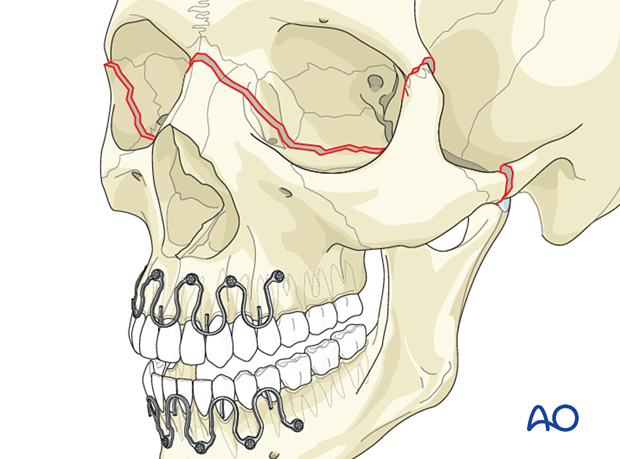
Option: hybrid arch bars
You can choose between traditional arch bars or hybrid arch bars.
Hybrid arch bars use screws to fix the arch bar to the bone, making the procedure faster.
2. Aftercare
Patient vision is evaluated as soon as awakening from anesthesia and then at regular intervals until hospital discharge.
A swinging flashlight test may serve in the unconscious or noncooperative patient; alternatively, an electrophysiological examination must be performed but this is dependent on the appropriate equipment (VEP).
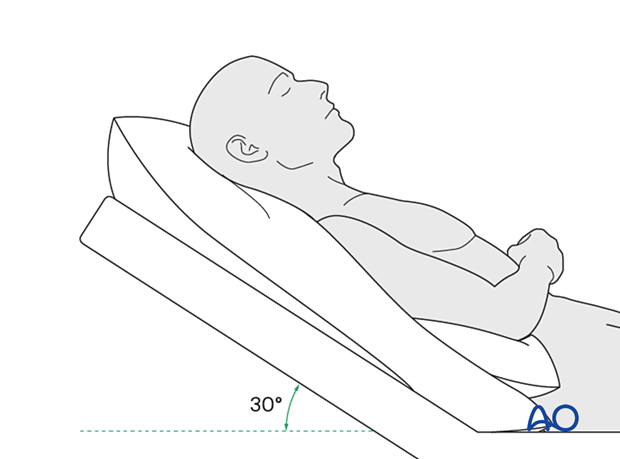
Postoperative positioning
Keeping the patient’s head in an upright position both preoperatively and postoperatively may significantly reduce periorbital edema and pain.
Nose-blowing
Nose-blowing should be avoided for at least ten days following orbital fracture repair to prevent orbital emphysema.
Medication
The following medications may be used:
- Analgesia as necessary (no aspirin or nonsteroidal anti-inflammatory drugs (NSAIDs) for seven days).
- Antibiotics: many surgeons use perioperative antibiotics. There is no clear advantage of any antibiotic, and the recommended duration of treatment is debatable.
- A nasal decongestant may be helpful for symptomatic improvement in some patients.
- Steroids, in cases of severe orbital trauma, may help with postoperative edema. Some surgeons have noted increased complications with perioperative steroids.
- Regular perioral and oral wound care must include disinfectant mouth rinse, lip care, etc.
Ophthalmological examination
Postoperative examination by an ophthalmologist may be requested. The following signs and symptoms are usually evaluated:
- Vision
- Extraocular motion (motility)
- Diplopia
- Globe position
- Perimetric examination
- Lid position
- If the patient complains of epiphora (tear overflow), the lacrimal duct must be checked
Postoperative imaging
Postoperative imaging may be considered. 2D and 3D imaging (CT, cone beam) are recommended to assess complex fracture reductions. An exception may be made for centers capable of intraoperative imaging.
In fractures involving the alveolar area, orthopantomograms (OPG) are helpful.
Wound care
Remove sutures from the skin after approximately five days if non-resorbable sutures have been used.
Apply ice packs (may be effective in the short term to minimize edema).
Avoid sun exposure and tanning to skin incisions for several months.
Diet
Diet depends on the fracture pattern.
Patients in MMF will remain on a liquid diet until the MMF is released.
Clinical follow-up
Clinical follow-up depends on the complexity of the surgery and whether the patient has any postoperative problems.
With patients that have fracture patterns that include periorbital trauma, consider the following issues:
- Globe position
- Double vision
- Other vision problems
Other issues to consider are:
- Facial deformity (including asymmetry)
- Sensory nerve compromise
- Problems of scar formation
Issues to consider with Le Fort fractures, palatal fractures, and alveolar ridge fractures include:
- Problems of the dentition and dental sensation
- Problems of occlusion
- Problems of the temporomandibular joint (TMJ), such as lack of range of motion, pain
MMF
The duration and use of MMF are controversial and highly dependent on the particular patient and the complexity of the trauma. In some cases, MMF may be recommended for 4–6 weeks.
The need and duration of MMF are very much dependent on:
- Fracture morphology
- Type and stability of fixation (including palatal splints)
- Dentition
- Coexistence of mandibular fractures
- Premorbid occlusion
Oral hygiene
Patients with arch bars, intraoral incisions, or wounds must be instructed about appropriate oral hygiene procedures. The presence of arch bars or elastics makes oral hygiene more complicated. A soft toothbrush (dipped in warm water to make it softer) should be used to clean the teeth and arch bars. Elastics are removed during oral hygiene procedures. Disinfectant mouth rinses (Chlorhexidine) should be prescribed and used at least three times a day to help sanitize the mouth.
For larger debris, a 1:1 mixture of hydrogen peroxide/Chlorhexidine can be used. The effervescent action of the hydrogen peroxide helps remove debris. A jet irrigator, (eg, Waterpik) is a handy tool to help remove debris from the wires. If used, care should be taken not to directly point the jet stream over intraoral incisions, which may lead to wound dehiscence.
Follow-up
The patient needs to be examined and reassessed regularly and often. Additionally, ophthalmological, ENT, and neurological/neurosurgical examinations may be necessary.
Special considerations for orbital fractures
Travel in pressurized aircraft is permitted following orbital fractures. Mild pain on descent may be noticed. However, flying in a non-pressurized plane should be avoided for a minimum of six weeks.
No scuba diving should be permitted for at least six weeks.













