Tumor biopsy
Indications
Guided tumor biopsy using intraoperative navigation is useful to assist in obtaining biopsies in anatomically difficult areas, especially those that may not be visible by surgical exposure.
Useful additional reading
Biopsy
In the area of the midface and the skull base, tumors often show a broad variety of histopathological entities and often neighbor critical anatomical structures eg. optic nerve, carotid artery etc. To determine the specific treatment, a biopsy has to be taken.
The following case illustrates the advantages of a pre-planned trajectory-guided tumor biopsy.
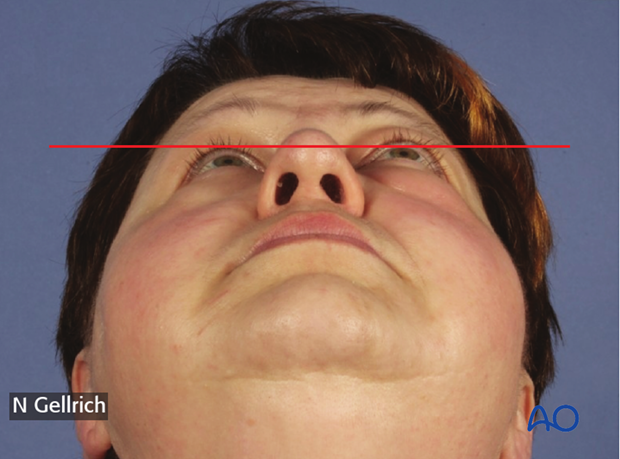
A 56 year old female with an unknown orbital tumor, demonstrated on MRI, presented with proptosis, pain and exophthalmos.
Lesions occupying the intraorbital space always pose a challenge both in terms of definite surgical removal as well as of pre-operative sampling for histopathological examination.
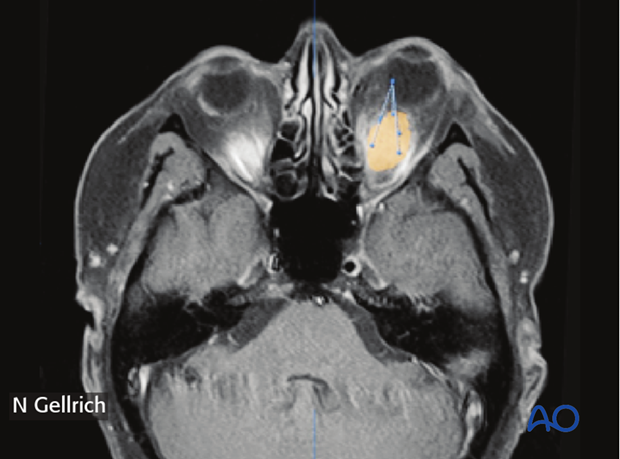
3D-CT scans and/or MRI is/are obtained using navigation fiduciary markers.
In this case, a dental splint attached to the maxilla containing radiopaque markers was used.
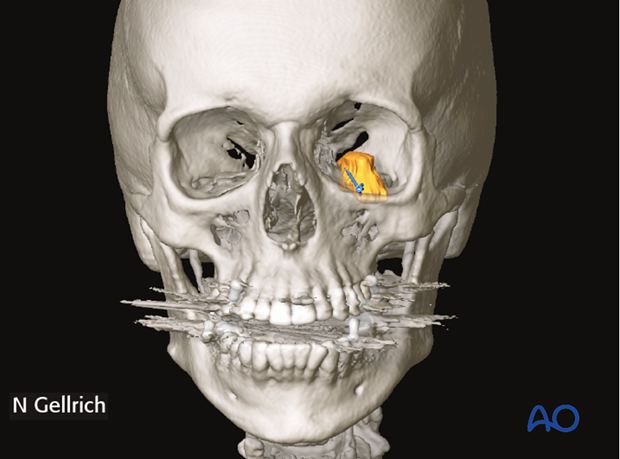
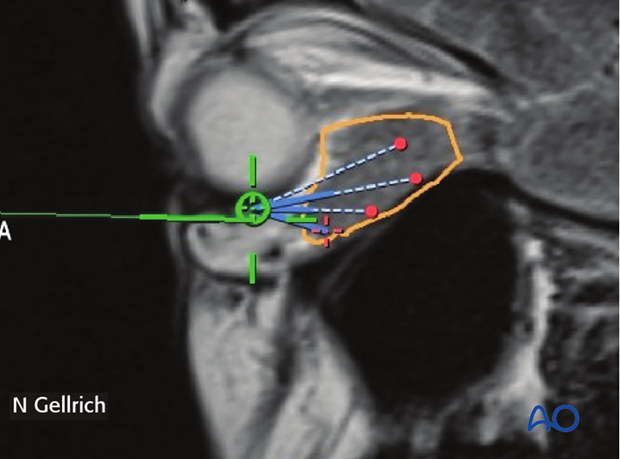
Using different imaging modalities (CT/MRI) the tumor shape was outlined manually using analyzing software.
A clearly defined anatomical representation of the patient’s anatomy together with a target region at the tumor position for taking the biopsies was achieved.
To accurately reach the planned biopsy site, additional trajectories were planned starting at anatomical landmarks (in this case superior to the left infraorbital foramen) and defining a path along the orbital cavity directly to where it is planned to take the biopsy.
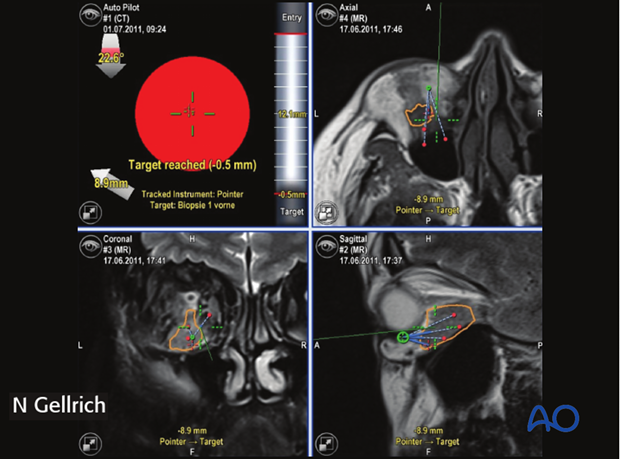
All pre-planned virtual patient data, objects and trajectories were transferred to an image guided surgery system.

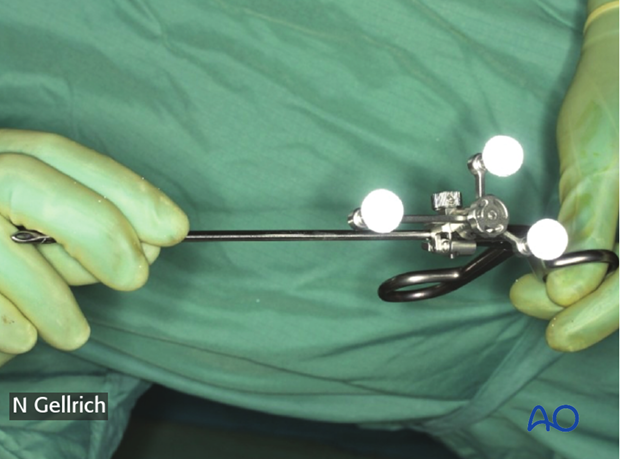
A regular biopsy forceps is registered. The position of the forceps tip and its vector can then be followed on the screen in real time.
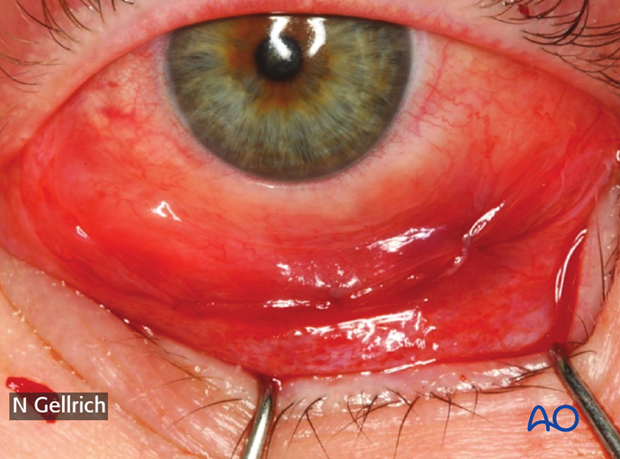
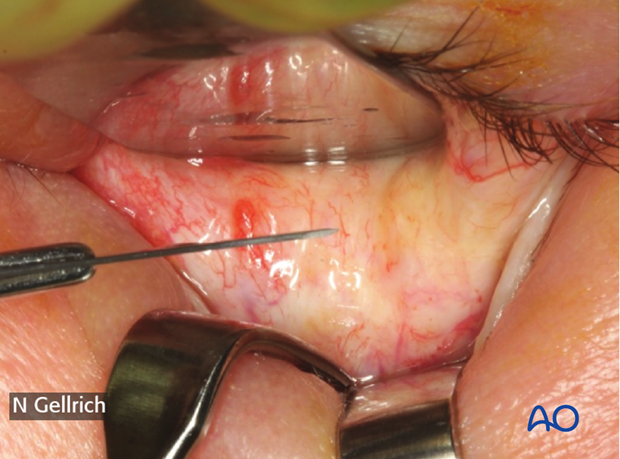
The forceps is then introduced through a transconjunctival approach.
When the tip of the forceps reaches the correct entry point, (in this case superior to the left infraorbital foramen) an autopilot feature will start and helps to guide the forceps to the point of interest.
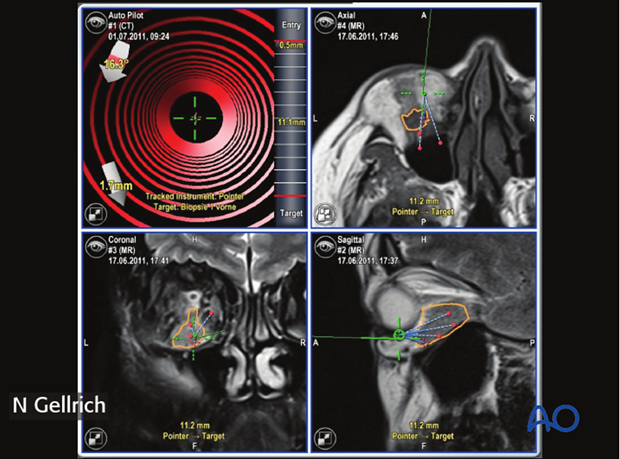
The distance to the target and the deviation from the ideal trajectory (in 3 dimensions) is shown in real time.
The autopilot will provide an audiovisual signal when the target is reached (and passed).
A representative biopsy is then taken as planned and submitted for histopathological examinations.
In this case, the pathology report confirmed the initial diagnosis of a lymphoma.
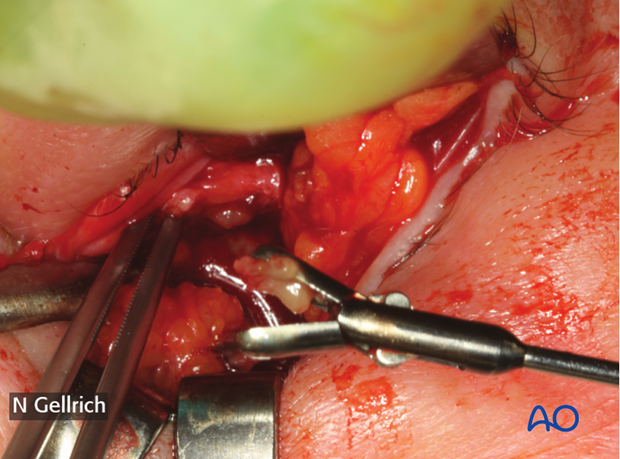
This picture shows the limited transconjunctival incision prior to wound closure.