Computer assisted surgery
1. What is computer assisted surgery?
Computer assisted surgery is the use of computers to manipulate DICOM data for planning, performing and/or assessing surgery.
Computer assisted surgery can be broken down into three basic steps, presurgical planning, intraoperative, and postoperative applications.
The benefits of presurgical planning include:
- Improved diagnostic accuracy
- Virtual simulation of the surgical procedure
Intraoperatively, the main benefit of computer assisted surgery is improved accuracy of the surgical repair. This results from the use of:
- Intraoperative navigation
- Cutting and drill guides
- 3D printed models
- Patient specific implants
- Intraoperative CT
Postoperatively, assessment of the accuracy of a surgical procedure is facilitated.
Disadvantages of computer aided surgery are primarily related to the cost of the hardware and software. There is also a greater time requirement necessary for training and use of the planning software compared to traditional techniques.
2. Planning software
There are multiple software packages currently (2013) available for presurgical planning. These include both freeware and for profit applications.
Ideal planning software should allow for the upload of the color virtual plan into the navigation system.
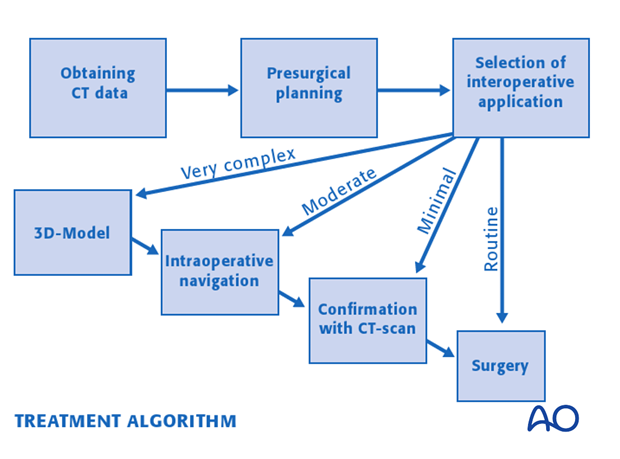
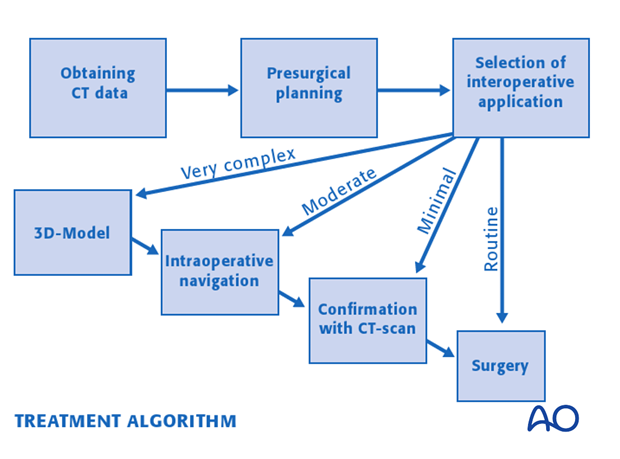
3. General workflow
This illustration incorporates the following pre- and intraoperative applications into a common surgical workflow. CT data is obtained, presurgical planning is performed and the intraoperative application is selected on the complexity of the procedure. Very complex cases may start with the use of models or guides followed by intraoperative navigation and final confirmation with intraoperative CT. Less complex cases may require one of more of these applications.
4. Intraoperative applications
Anatomic models
Rapid prototype models can be fabricated externally or in house to provide a physical 3D-representation of the patient preoperatively or after virtual surgery. These models can be costly and time consuming to fabricate. Therefore they are typically used for complex deformities where physical osteotomies on a model are felt to be necessary or in which presurgical hardware shaping is beneficial.
Some fabrication processes allow for sterilization and intraoperative use.

Drill guides and cutting templates
Guides and templates are generally used intraoperatively to assist accurate placement of drill holes (dental implants, distractor placement etz)...
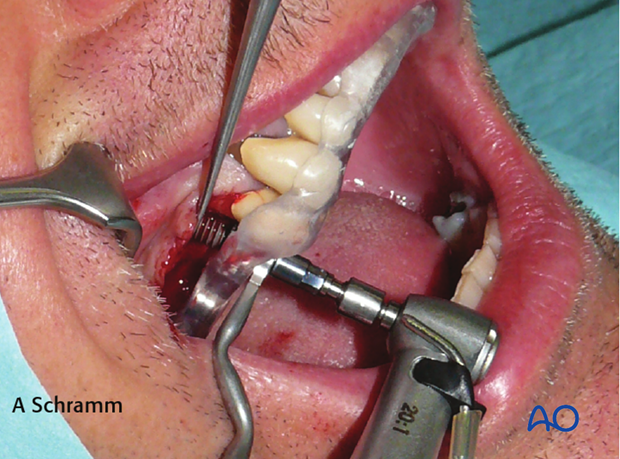
...and osteotomies (fibular/mandibular osteotomies).
Patient specific implants
Patient specific implants are fabricated to either fill a bony defect or accurately reconstruct a bony contour.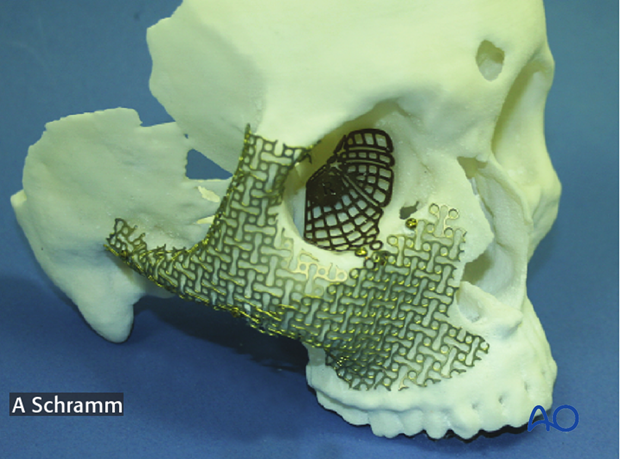
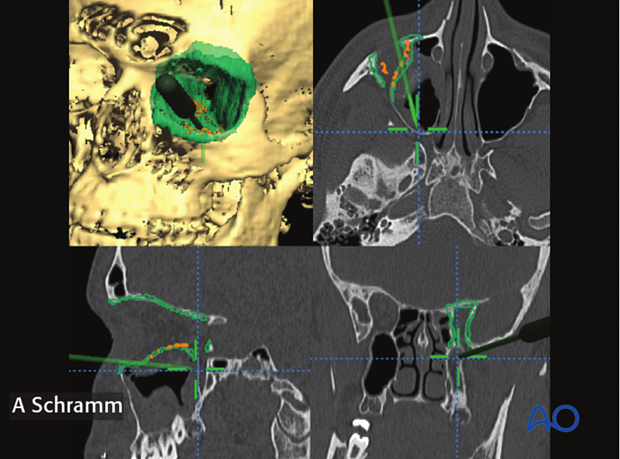
Navigation
Intraoperative navigation is an interactive process used to confirm bony reduction or implant positioning. A trackable probe is moved along the bone/implant contour, while position is confirmed on the monitor. Navigation provides anatomic information without the use of X-rays. While the information is not as robust as intraoperative CT, navigation can be used as often as needed until the implant is found to be in the appropriate position without radiation exposure.
Intraoperative CT
Intraoperative CT gives definitive anatomic information about bony reduction or radio opaque implant placement. This is generally performed when the surgeon is confident of the repair, as repeated CT scans may result in excessive X-ray exposure.
5. Virtual planning
Data acquisition
Appropriate imaging data is obtained prior to surgery. This may include MRI for soft tissue tumors and/or CT for bony reconstruction or orthognathic surgery.
This data is then imported into the planning software.
Segmentation
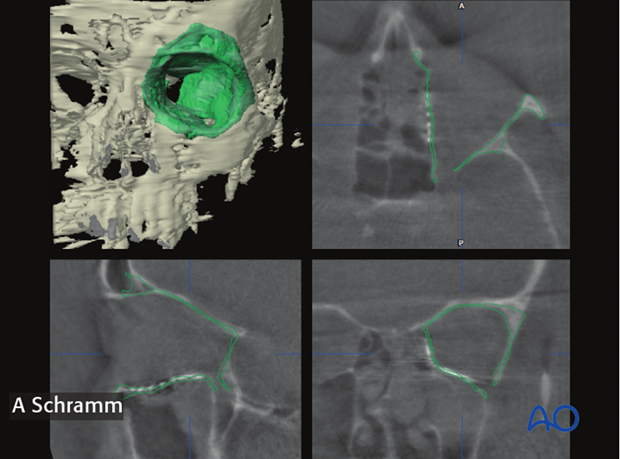
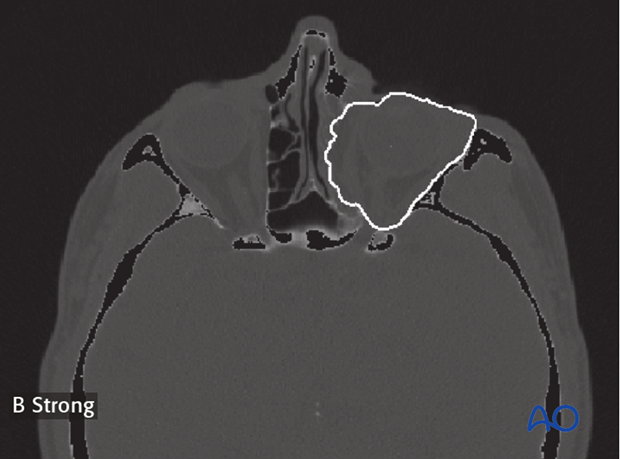
Segmentation using Hounsfield units (radiodensity) to divide a data set into bone and soft tissue.
Further segmentation can be done either manually or automatically, allowing the surgeon to manipulate a defined anatomic structure virtually.
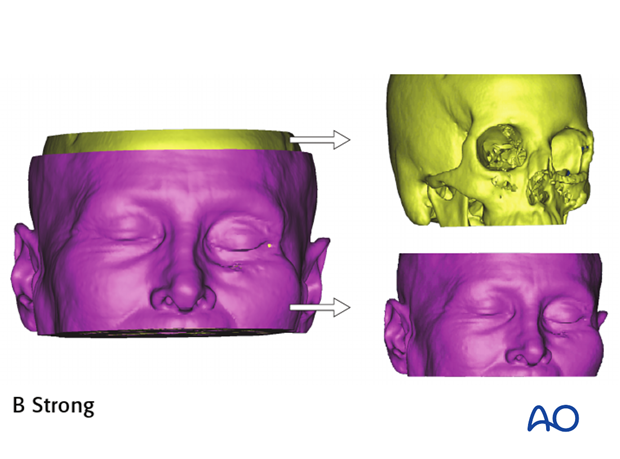
Manual segmentation can be rapidly performed by dividing an anatomic structure along a cutting plane.

However, complex segmentations such as the orbit or mandible will require outlining of the anatomic structure in sequential axial slices and combining these to form a 3D volume. This is very labor intensive and not conducive to routine clinical care.
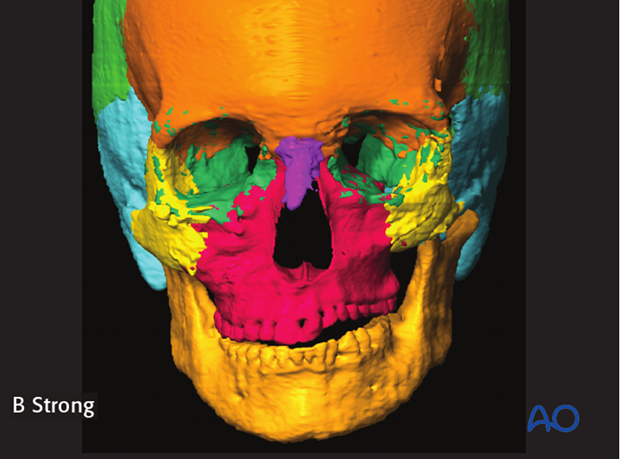
Auto segmentation has been developed for the segmentation of more complex structures. This allows the computer to automatically segment an anatomic structure into pre-defined component parts such as maxilla, orbit, frontal bone etc.
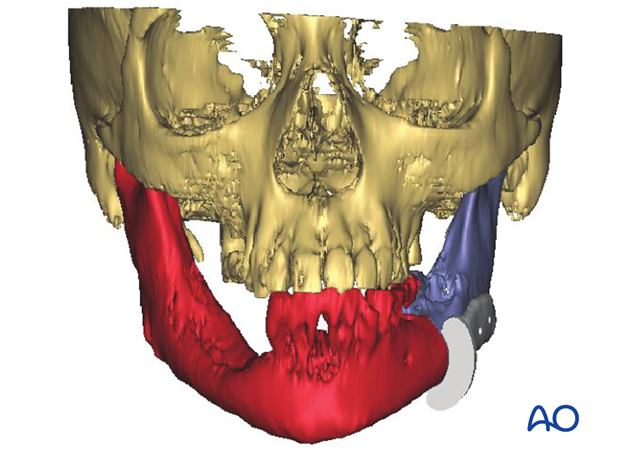
The illustration on the left show the auto segmentation into:
- Orbit (left/right)
- Maxilla
- Zygoma (left/right)
- Mandible
- Frontal bone
- Zygoma (left/right)
- Temporal bone (left/right)
Preoperative analysis
There is a broad range of measurements that can be performed during the preoperative analysis.
These include:
- Distance measurements
- Angle measurements.
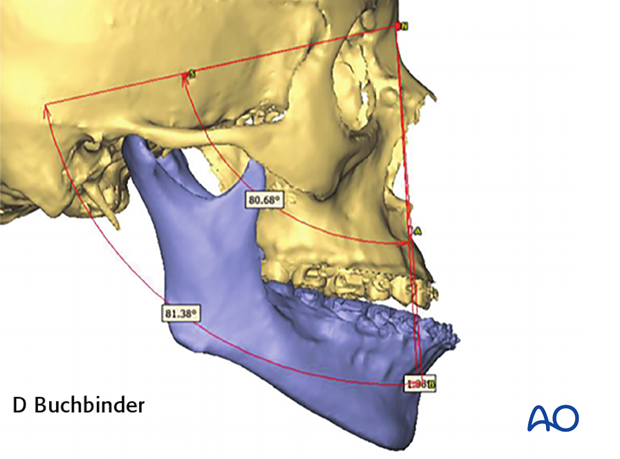
- Volume measurements.
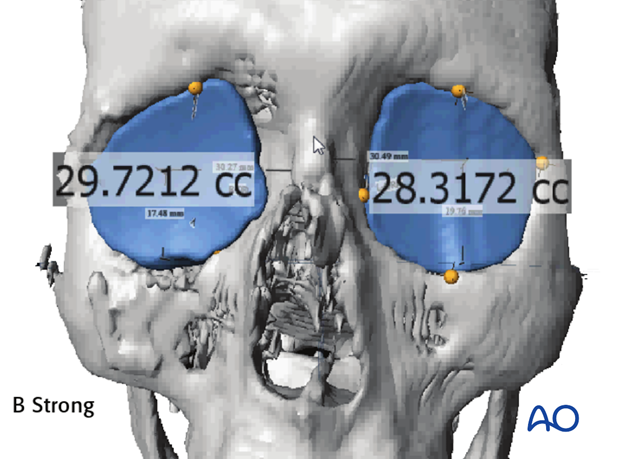
Presurgical planning software moves the control of data presentation from the hands of the radiologist to the surgeon. He/she can rotate and visualize the virtual model with 3 degrees of freedom. This offers an accurate depiction of depth, width, and projection. The surgeon can assess bony defects or deformities that would otherwise be very difficult to perceive in a 2D-image.
Editing
Editing functions allow the surgeon to optimize the virtual model by erasing, adding or moving structures.
Some examples might include:
- removal of unnecessary peripheral structures to isolate an anatomic region
- adding thickness to the bony orbit to ensure that a stereolithographic model is strong enough to allow shaping of hardware
- refining the contour of the bony orbit
This function allows the surgeon to mirror a template of the normal anatomy from the non-injured to the injured side of the virtual model. Hence, it is mainly useful for unilateral injuries/deformities.
It is important that the surgeon:
- defines a symmetric mirror plane so that uninjured template can be mirrored accurately over the injured anatomy. Some manipulation and refinement will be necessary.
- makes a large enough template such that it will extend beyond the area of injury and can be aligned with the uninjured anatomy on the affected side.
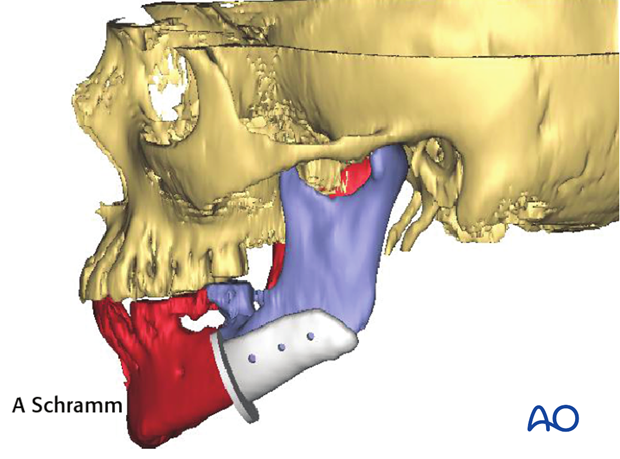
Presurgical planning/Virtual surgery
The surgical procedure is then planned in a virtual environment.
This may involve:
- determination of tumor resection margins
- osteotomies and occlusal corrections
- fracture reduction
Presurgical planning may involve one or more of the five following steps.
6. Image fusion
Image fusion is used to precisely overlay two different datasets. This allows the surgeon to accurately analyze anatomic differences between the datasets. Image fusion can be performed with two different CT data sets. This is most commonly used for pre- and postoperative analysis. Fusion of MRI and CT data sets is commonly performed for tumor surgery.













