Orbital reconstruction
1. General consideration
Due to the high incidence of greenstick fractures and the rapid reossification and remodeling, conservative treatment is often the best treatment in a pediatric patient unless there are signs of muscle or periorbital entrapment.
Please refer to general considerations on pediatric fractures for further details.
2. Emergency treatment
Emergency treatment in orbital fractures may be indicated in the following cases:
- Entrapment of eye muscle or periorbita (in trapdoor fractures)
- Partial or complete visual loss due to direct or indirect optic nerve trauma
- Severely increased intraocular pressure
- Acute space-occupying lesion (eg, retrobulbar hematoma, emphysema)
- Severe shift of orbital content
- Severe nasal or oral bleeding
Usually, there is no need for emergency treatment in orbital floor/medial wall fractures unless there is muscle entrapment with risk of ischemia or severe ongoing hemorrhage in the orbital cavity, the paranasal, or nasal cavity.
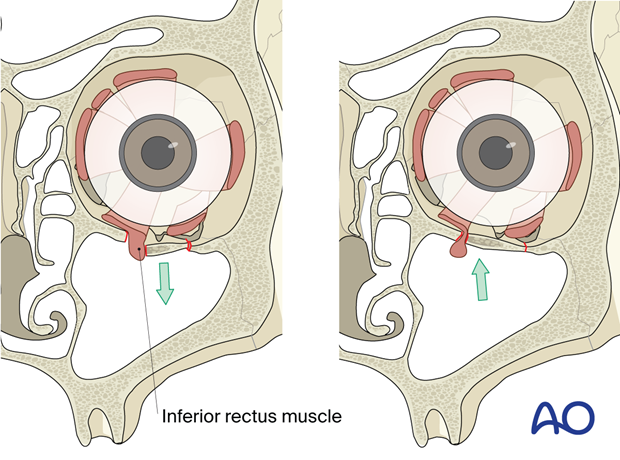
Entrapment of inferior rectus muscle
In some younger patients, the so-called trapdoor phenomenon can occur in which there is a risk of ischemia and necrosis of the entrapped rectus muscle and periorbital contents. Immediate release of entrapped tissues is necessary.
The inferior rectus muscle is the most common ocular muscle to become entrapped within an orbital floor fracture (trap-door phenomenon). CT scan imaging with coronal and sagittal views is necessary to accurately diagnose entrapment. Entrapment requires urgent release of the muscle and periorbita to prevent necrosis. Clinical examination should demonstrate impaired vertical eye motion. Entrapment is often associated with severe ocular pain, nausea, and vomiting on upgaze.
3. Case example 1: Orbital blowout fracture
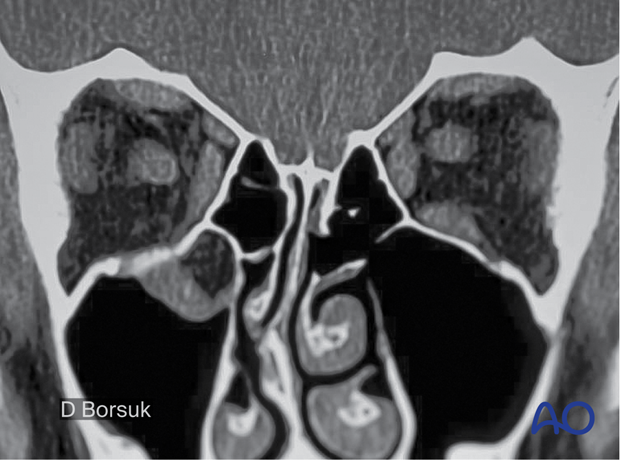
11-year-old boy with right orbital blowout fracture. Periorbital ecchymosis and swelling are observed as well as the white eye appearance of the right globe.

A coronal view on a CT scan demonstrates the entrapment of the right inferior rectus muscle.
Notice how the muscle is no longer visible in the orbit, but it is seen in the maxillary sinus below the orbital floor. This fracture should be surgically repaired as soon as possible to avoid necrosis of the entrapped tissues.
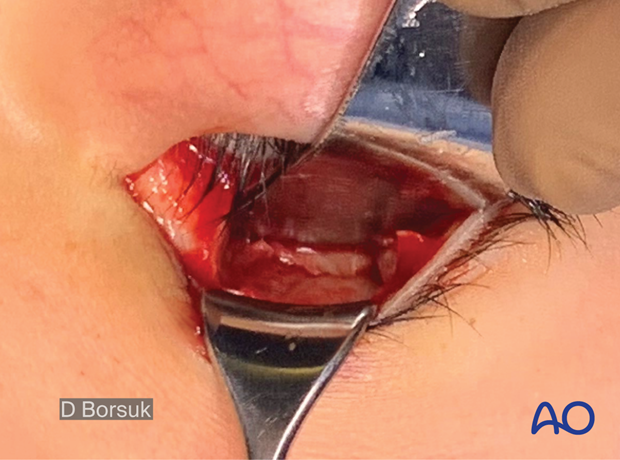
A transconjunctival approach to the orbital floor will give access to the blowout fracture and allow adequate reconstruction with any material.
Notice the periorbita entrapped within the floor fracture.
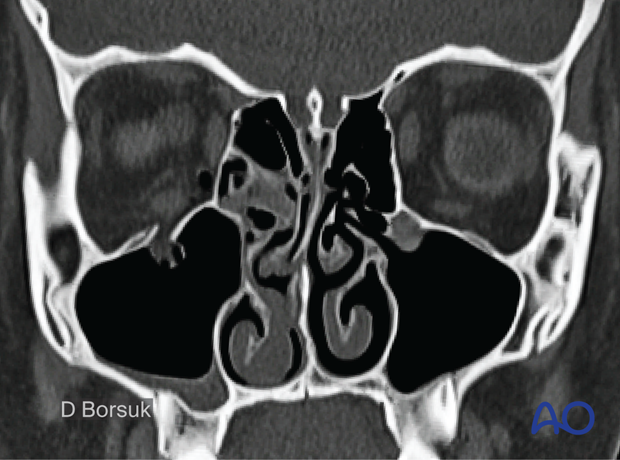
4. Case example 2: Orbital blowout fracture
13-year-old boy with right orbital blowout fracture. Notice the entrapment of periorbital tissue within the floor fracture without muscle entrapment. When compared to the left inferior rectus, the right muscle appears round and not oval. The round appearance indicates muscle swelling and a possible globe position change and enophthalmos.
5. Surgical approach
A transconjunctival approach is recommended in children due to its low complication profile and lack of visible scars.
6. Reduction
The surgical reduction is performed as in the adult section.
A forced duction test should always be performed before and after fracture reduction and reconstruction.
7. Choice of reconstruction material
Pediatric considerations
Due to the growing orbit and the variation in shape and size, absorbable materials should be considered to restore pediatric floor fractures.
Alternatively, autogenous bone graft and titanium mesh/anatomic plates may be used as described in the adult section.
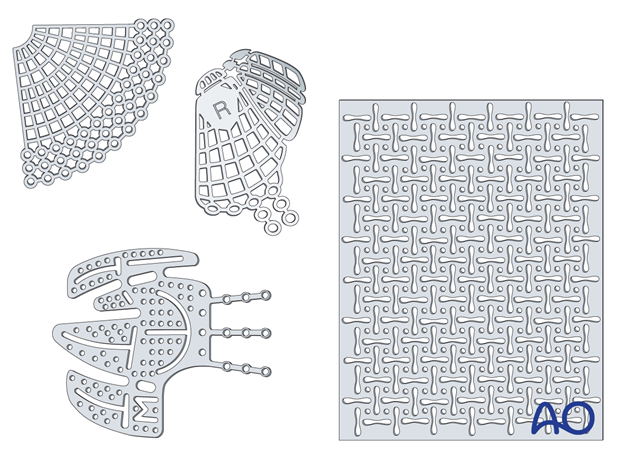
Resorbable materials
Thermoplastic and non-thermoplastic materials
Advantages
- Availability
- Handling/contourability (only for thermoplastics)
- Smooth surface and smooth edges
Disadvantages
- Non radiopaque
- Degradation of material with possible contour changes
- Sterile infection / inflammatory response
- Challenging to shape according to patient’s anatomy (only for non-thermoplastics)
- Non perforated implants may not allow drainage of fluid or blood from the orbit
- Any material may have sharp edges if not properly contoured
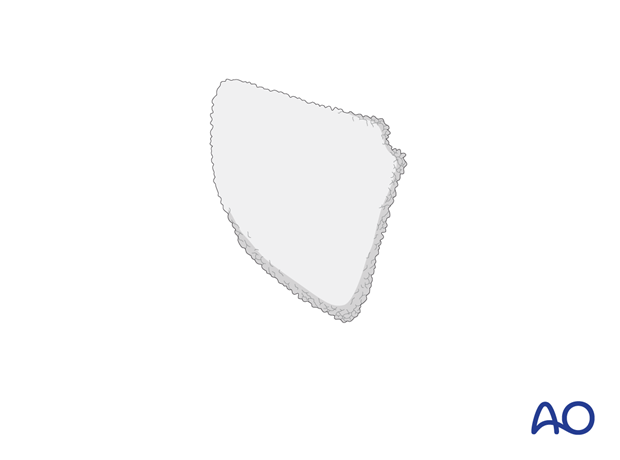
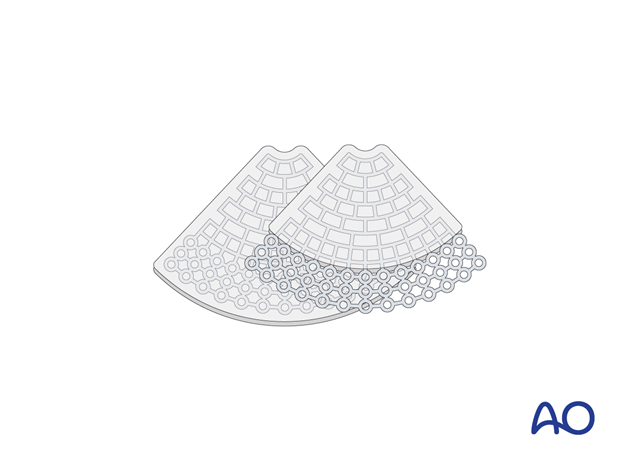
Illustration showing a non-thermoplastic poly-p-dioxanone sheet (PDS).
Titanium meshes
Advantages
- Availability
- Stability
- Contouring (aided using a sterile artificial skull)
- Ideal for large defects or three-wall fractures (the pre-bent plate is limited to medial wall and orbital wall fractures only)
- Radiopaque
- Spaces within the mesh to allow dissipation of fluids and blood
- No donor site needed
- Tissue incorporation may occur
Disadvantages
- Costs
- Possible sharp edges if not adequately trimmed
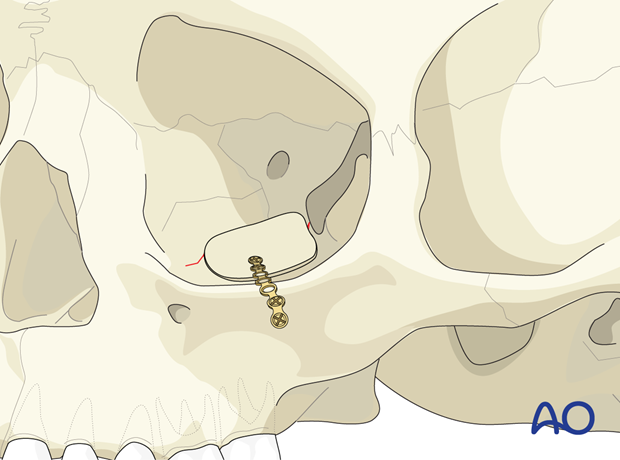
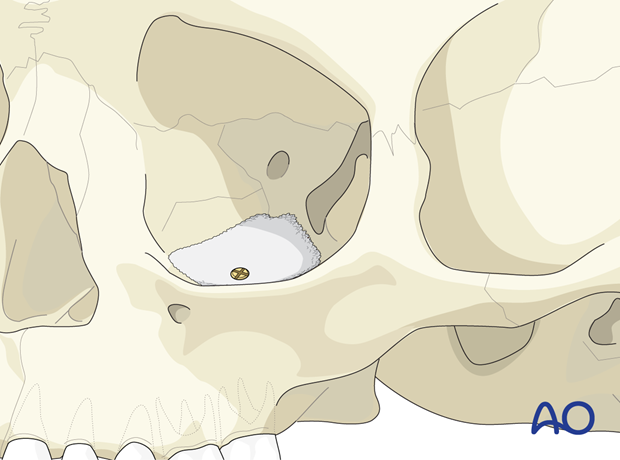
Bone graft
The illustration shows an individual calvarial bone graft.
Advantages:
- Low material costs
- Smooth surface
- Variability in thickness
- Radiopacity
- Maximal biocompatibility
- Periorbita readily dissects off of the bone in secondary reconstructions
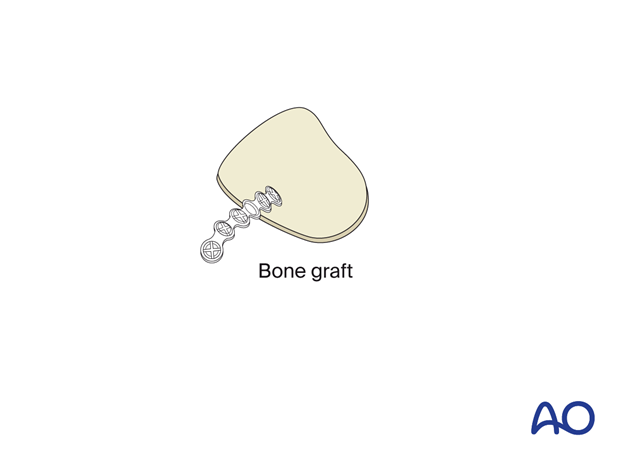
Disadvantages:
- Additional donor site needed (necessitating extra surgery time for harvest, pain, scar, and possible surgical complications)
- Possible contour and dimensional changes due to remodeling
- Difficult to shape according to patient’s anatomy
- Less drainage from the orbit than with titanium mesh
Porous polyethylene sheets (PPE)
Advantages
- Availability
- Contouring (eased by the sterile artificial skull)
- Smooth edges
- Allows tissue ingrowth
Disadvantages
- Not radiopaque (not visible on postoperative images)
- Lack of rigidity when a very thin wafer of PPE is used. When a thicker rigid wafer is used, there is a risk of causing a dystopia.
- Less drainage from the orbit than with titanium mesh
- Difficult to reproduce normal orbital anatomy
Composite of porous polyethylene and titanium mesh
By combining titanium mesh with porous polyethylene, the material becomes radiopaque and more rigid than porous polyethylene of a similar thickness. Some surgeons also believe that there is less risk of having retained sharp barbs, leading to entrapment of soft tissues during placement.
Advantages
- Availability
- Stability
- Contouring (eased by the sterile artificial skull)
- Adequate in large three-wall fractures (the pre-bent plate is limited to medial wall and orbital wall fractures only).
- Radiopacity
- No donor site needed
- Tissue incorporation may occur
Disadvantage
- Less drainage from the orbit than with titanium mesh
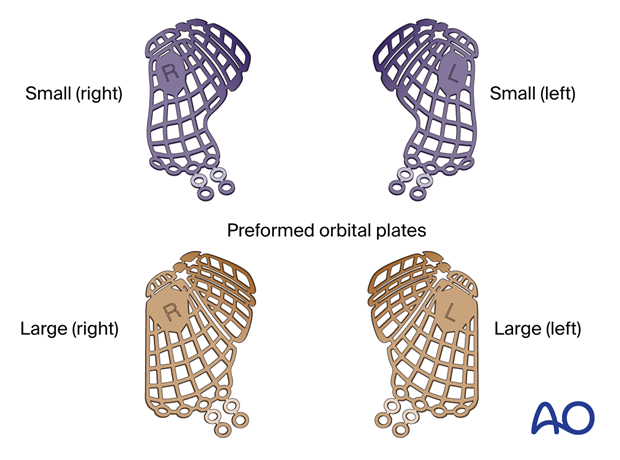
Preformed orbital implant
Advantages
- Radiopacity
- Smooth surface
- Minimal or no contouring necessary
- Restores normal orbital anatomy
Disadvantages
- Cost
- May be difficult to position properly
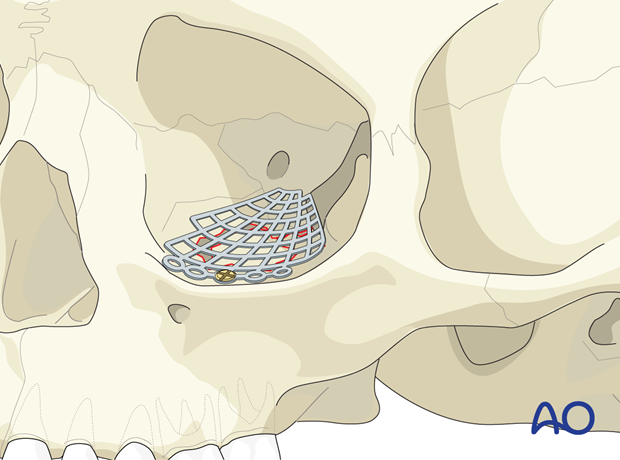
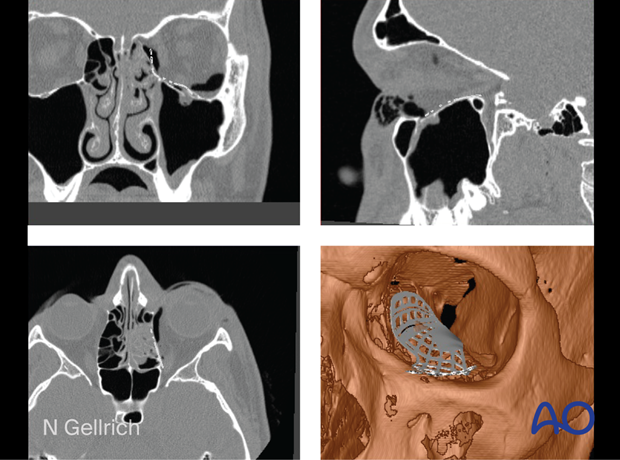
Multiplanar and 3D view showing a preformed mesh plate placed before surgery into patient CT dataset.
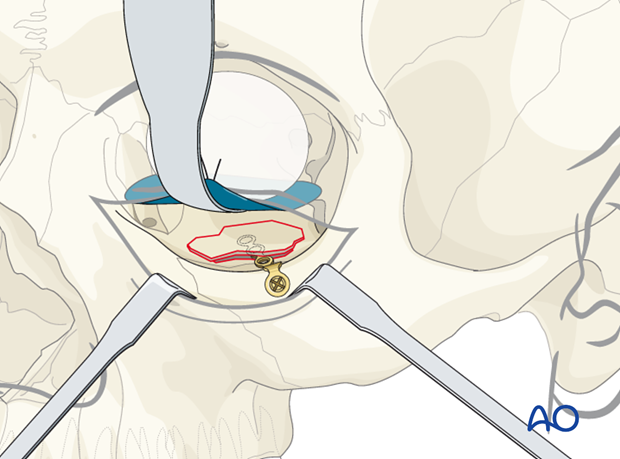
Implant fixation
Fixation of orbital reconstruction material varies with the type and nature of the fracture.
Fixation of most materials in the orbital floor is achieved by the use of one or more screws. The diameter depends on anatomical requirements but will typically vary between 1.0, 1.3, or 1.5 mm. Alternatively, Matrix Midface screws can be used.
8. Fixation
In small fractures, pediatric orbital floor fractures may be reduced without reconstruction. If, however, the fragment is unstable or the defect is large, reconstruction of the floor should be considered.
Resorbable or non-resorbable material may be used to restore the normal anatomy of the floor.
Surgical fixation is performed as in for adults.
9. Aftercare
Patient vision is evaluated as soon as awakening from anesthesia and then at regular intervals until hospital discharge.
A swinging flashlight test may serve to confirm pupillary response to light in the unconscious or non-cooperative patient; alternatively, an electrophysiological examination while possible is seldom available in the operation area.
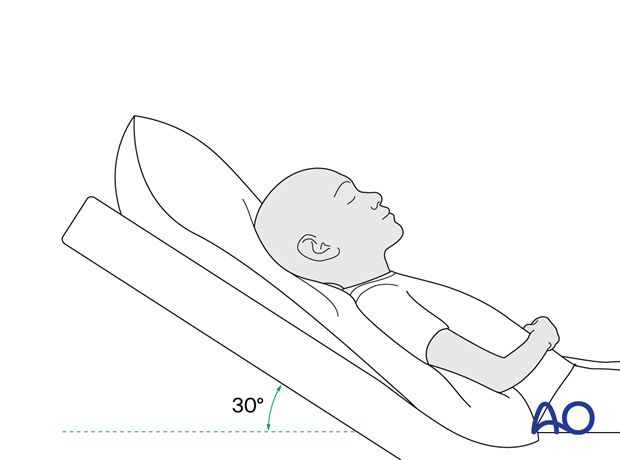
Postoperative positioning
Keeping the patient’s head in an upright position both preoperatively and postoperatively may significantly improve periorbital edema and pain.
Nose blowing
Nose blowing should be avoided for at least ten days following orbital fracture repair to prevent orbital emphysema.
Medication
The use of the following perioperative medication is controversial. There is little evidence to make solid recommendations for postoperative care.
- No aspirin or nonsteroidal anti-inflammatory drugs (NSAIDs) prescribed for seven days.
- Provide analgesia as necessary.
- Antibiotics (many surgeons use perioperative antibiotics. There is no clear advantage of any antibiotic, and the recommended duration of treatment is debatable.)
- A nasal decongestant may be helpful for symptomatic improvement in some patients.
- Steroids, in cases of severe orbital trauma, may help with postoperative edema. Some surgeons have noted increased complications with perioperative steroids.
- Ophthalmic ointment should follow local and approved protocol. This is not generally required in the case of periorbital edema. Some surgeons prefer it. Some ointments have been found to cause significant conjunctival irritation.
Ophthalmological examination
Postoperative examination by an ophthalmologist may be requested. The following signs and symptoms are usually evaluated:
- Vision
- Extraocular motion (motility)
- Diplopia
- Globe position
- Visual field examination
- Lid position
- If the patient complains of epiphora (tear overflow), lacrimal duct function must be checked.
Postoperative imaging
Postoperative imaging should be performed within the first days after surgery to assess reductions and possible malpositioning. 3D imaging (CT, cone beam) is recommended to assess complex fracture reductions. An exception may be made for centers capable of intraoperative imaging.
Especially in fractures involving the alveolar area, orthopantomograms (OPG) are helpful.
Wound care
Ice packs are effective in the short term to minimize edema.
Remove the sutures from the skin after approximately five days if non-resorbable sutures have been used.
Avoid sun exposure and tanning to skin incisions for several months.
Clinical follow-up
Clinical follow-up depends on the complexity of the surgery and whether the patient has any postoperative problems.
With patients having fracture patterns including periorbital trauma, issues to consider are the following:
- Globe position
- Double vision
- Other vision problems
Other issues to consider are:
- Facial deformity (incl. asymmetry)
- Sensory nerve compromise
- Problems of scar formation
Eye movement exercises
Following orbital fractures, eye movement exercises should be considered.
Implant removal
Generally, orbital implant removal is not necessary except in the event of infection or exposure.
Follow-up
Follow-up should be performed to monitor healing and vision.
Special considerations for orbital fractures
Travel in commercial airlines is permitted following orbital fractures. Commercial airlines pressurize their cabins. Mild pain on descent may be noticed.
No scuba diving should be permitted for at least six weeks.
Children who participate in sports should consider wearing eye protection for the first three months following the fracture.













