Orbital reconstruction
1. General consideration
Due to the high incidence of greenstick fractures and the rapid reossification and remodeling, conservative treatment is often the best treatment in a pediatric patient.
Please refer to general considerations on pediatric fractures for further details.
2. Approach
A transconjunctival lower eyelid surgical approach with a transcaruncular extension is usually recommended in children due to its low complication profile and lack of visible scar.
3. Reduction and fixation
The surgical reduction and fixation are performed as described in the adult section.
4. Aftercare
Patient vision is evaluated as soon as awakening from anesthesia and then at regular intervals until hospital discharge.
A swinging flashlight test may serve to confirm pupillary response to light in the unconscious or non-cooperative patient; alternatively, an electrophysiological examination while possible is seldom available in the operation area.
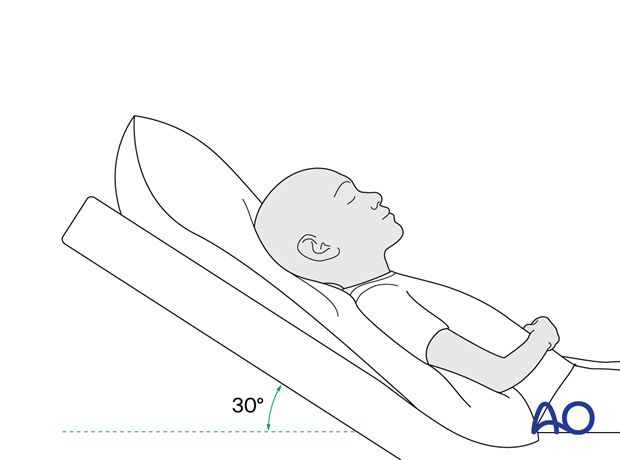
Postoperative positioning
Keeping the patient’s head in an upright position both preoperatively and postoperatively may significantly improve periorbital edema and pain.
Nose blowing
Nose blowing should be avoided for at least ten days following orbital fracture repair to prevent orbital emphysema.
Medication
The use of the following perioperative medication is controversial. There is little evidence to make solid recommendations for postoperative care.
- No aspirin or nonsteroidal anti-inflammatory drugs (NSAIDs) prescribed for seven days.
- Provide analgesia as necessary.
- Antibiotics (many surgeons use perioperative antibiotics. There is no clear advantage of any antibiotic, and the recommended duration of treatment is debatable.)
- A nasal decongestant may be helpful for symptomatic improvement in some patients.
- Steroids, in cases of severe orbital trauma, may help with postoperative edema. Some surgeons have noted increased complications with perioperative steroids.
- Ophthalmic ointment should follow local and approved protocol. This is not generally required in the case of periorbital edema. Some surgeons prefer it. Some ointments have been found to cause significant conjunctival irritation.
Ophthalmological examination
Postoperative examination by an ophthalmologist may be requested. The following signs and symptoms are usually evaluated:
- Vision
- Extraocular motion (motility)
- Diplopia
- Globe position
- Visual field examination
- Lid position
- If the patient complains of epiphora (tear overflow), lacrimal duct function must be checked.
Postoperative imaging
Postoperative imaging has to be performed within the first days after surgery. 3D imaging (CT, cone beam) is recommended to assess complex fracture reductions. An exception may be made for centers capable of intraoperative imaging.
Wound care
Ice packs are effective in the short term to minimize edema.
Remove the sutures from the skin after approximately five days if non-resorbable sutures have been used.
Avoid sun exposure and tanning to skin incisions for several months.
Clinical follow-up
Clinical follow-up depends on the complexity of the surgery and whether the patient has any postoperative problems.
With patients having fracture patterns including periorbital trauma, issues to consider are the following:
- Globe position
- Double vision
- Other vision problems
Other issues to consider are:
- Facial deformity (incl. asymmetry)
- Sensory nerve compromise
- Problems of scar formation
Eye movement exercises
Following orbital fractures, eye movement exercises should be considered.
Implant removal
Generally, orbital implant removal is not necessary except in the event of infection or exposure.
Follow-up
Follow-up should be performed to monitor healing and vision.
Special considerations for orbital fractures
Travel in commercial airlines is permitted following orbital fractures. Commercial airlines pressurize their cabins. Mild pain on descent may be noticed.
No scuba diving should be permitted for at least six weeks.
Children who participate in sports should consider wearing eye protection for the first three months following the fracture.













