Cross pinning and lag screw
1. Principles
This technique may be considered in juvenile or adult dog if the fracture configuration allows for inherent stability when reduced.
The addition of crossed pins provides ancillary stabilization to allow healing with early range of motion of the joint. For maximal stability the pins must cross proximal to the fracture.
Interfragmentary compression is achieved with a lag screw for anatomical reduction of the wedge fracture in the metaphysis. This step is usually performed first to ensure that pin placement does not interfere with the reduction.
2. Positioning and approach
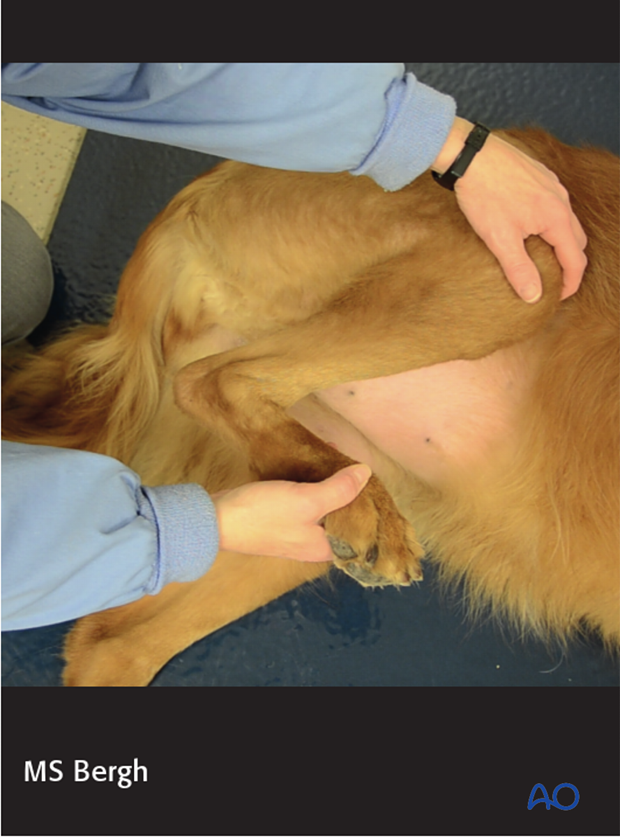
This procedure is performed with the patient placed in either of the two positions:
The lateral parapatellar approach is used.
3. Surgical technique
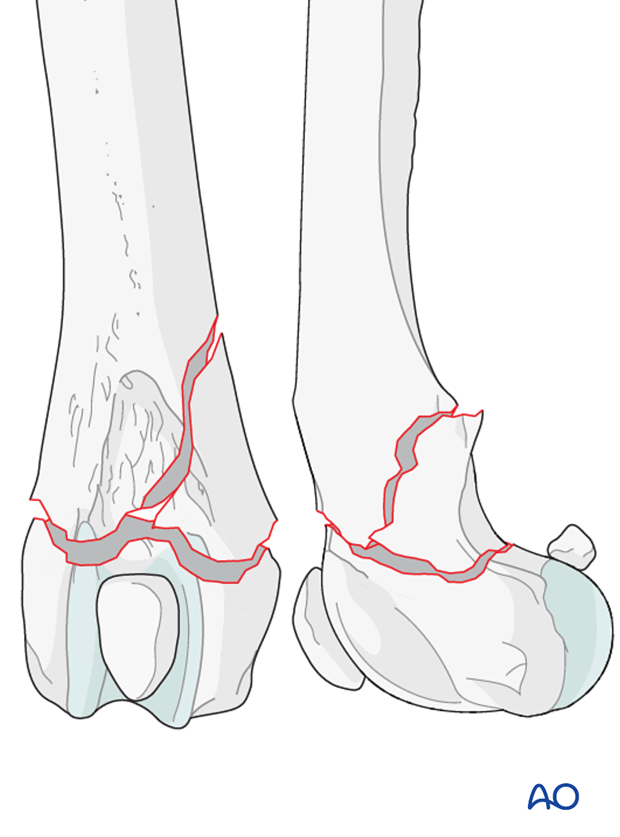
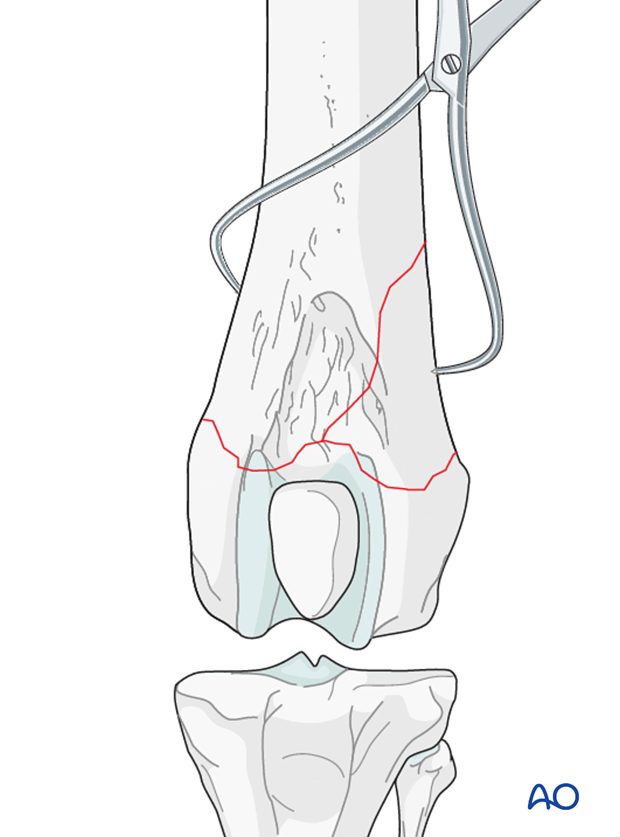
Reduction and preliminary stabilization
With the patient under general anesthesia, the fracture may be reduced with pointed reduction forceps on each fragment. Anatomic reduction is desired in all cases. Under-reduction of the fracture should be avoided as it is less stable, and the cranial aspect of the metaphysis would interfere with the gliding of the patella in the trochlear groove.
Note: Bone in juvenile patients is very soft. Care must be taken not to damage it during reduction.
Reduction may be difficult if the fracture is more than 48 hours old, due to the contraction of the muscles and peri-articular fibrosis.
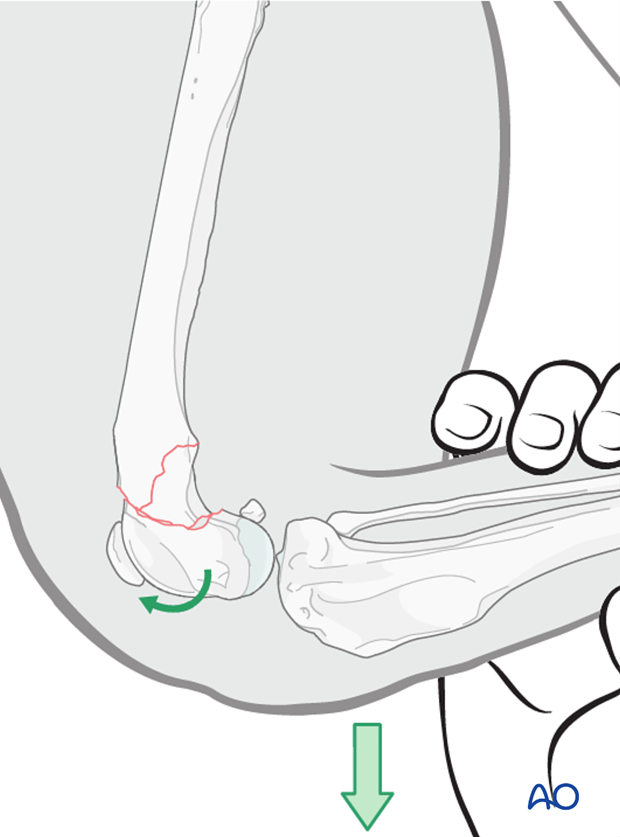
Pearl: Achieving partial reduction of the fracture and gently extending the stifle joint, may aid reduction.
Alternatively, the fracture may be reduced flexing the stifle joint and extending the tarsus, to reduce tension on the gastrocnemius mechanism. With the femur stabilized, the tibia is pulled cranially, which is used to push the distal fragment into reduction. The stifle is then extended to lock the fragments into position.
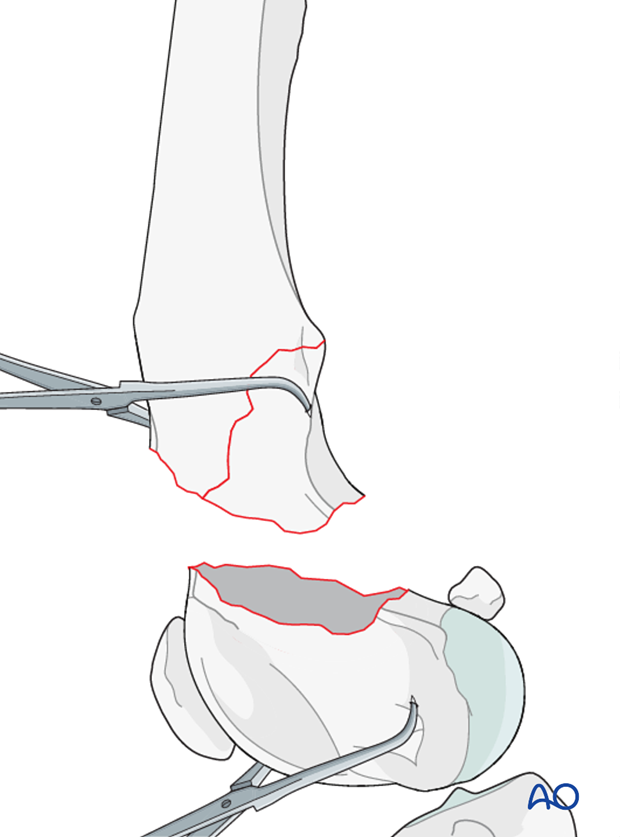
Preliminary stabilization is achieved with forceps placed across the wedge fracture in the metaphysis.
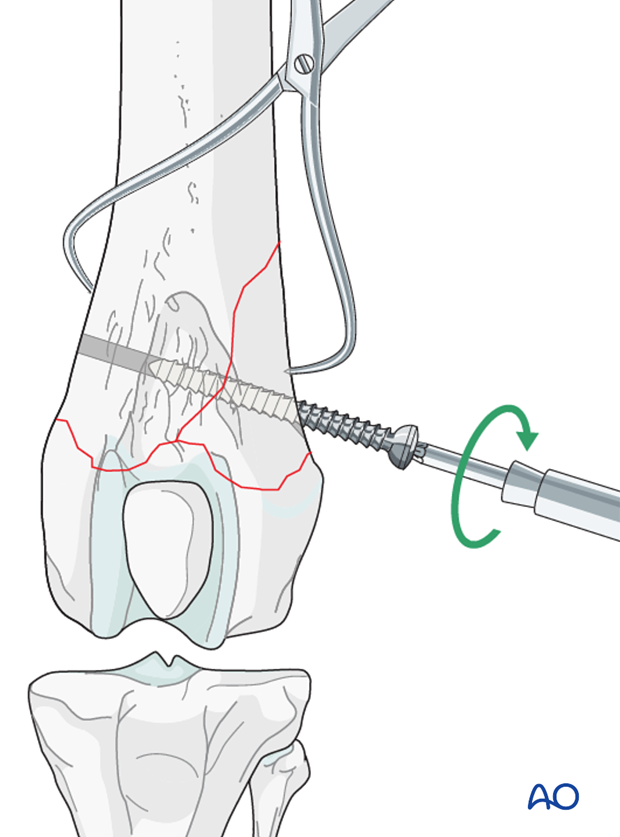
Screw insertion
A screw is inserted in lag fashion, perpendicular to the fracture line.
Read more about lag screw fixation.
Pin insertion
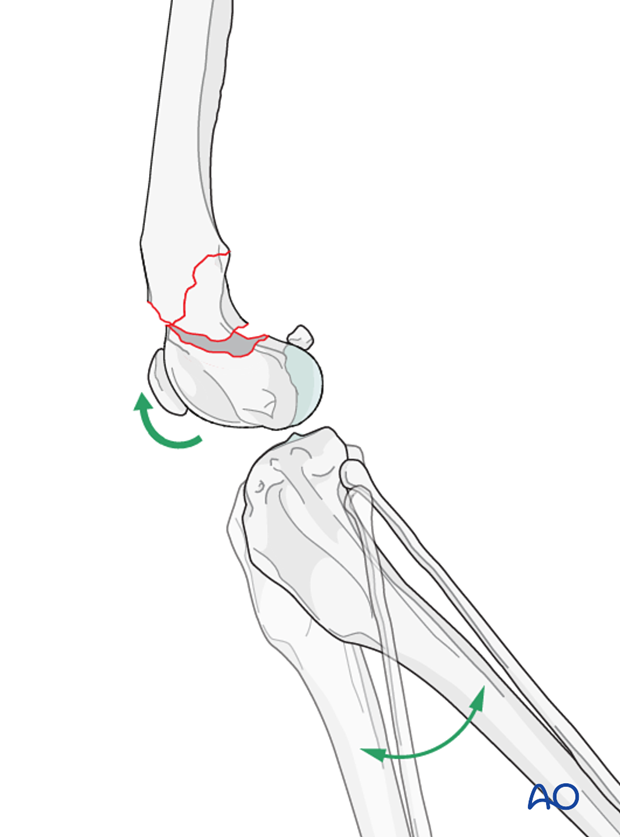
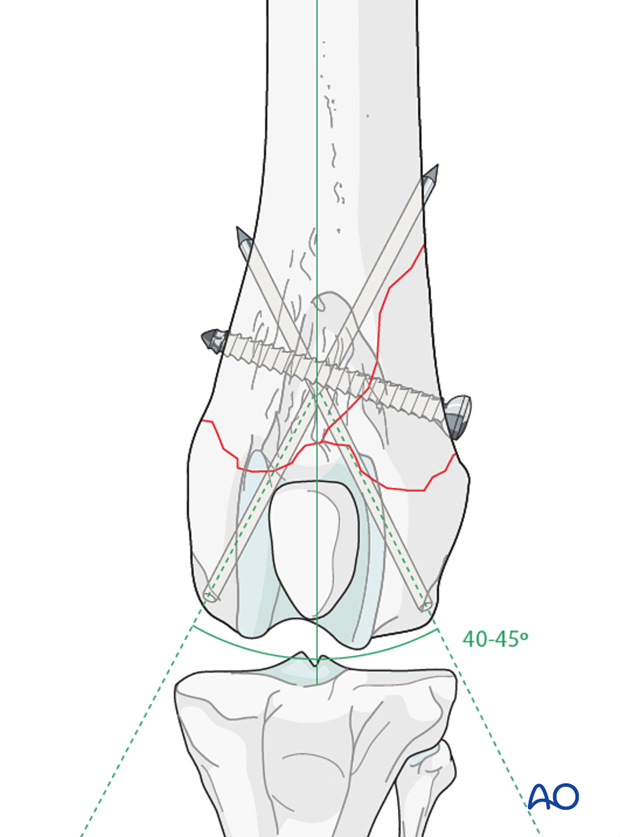
Two Steinmann pins or K-wires (depending on the size of the patient) are driven obliquely across the fracture plane to cross each other proximal to the fracture.
Insertion starts at the proximal aspect of the origin of the long digital extensor tendon, in the extensor fossa of the lateral femoral condyle.
Tip: Slight over reduction of the fracture prior to pin insertion helps ensure anatomic reduction when pins are seated. Otherwise, as the pins are inserted, the distal fragment moves caudal and can be under reduced.
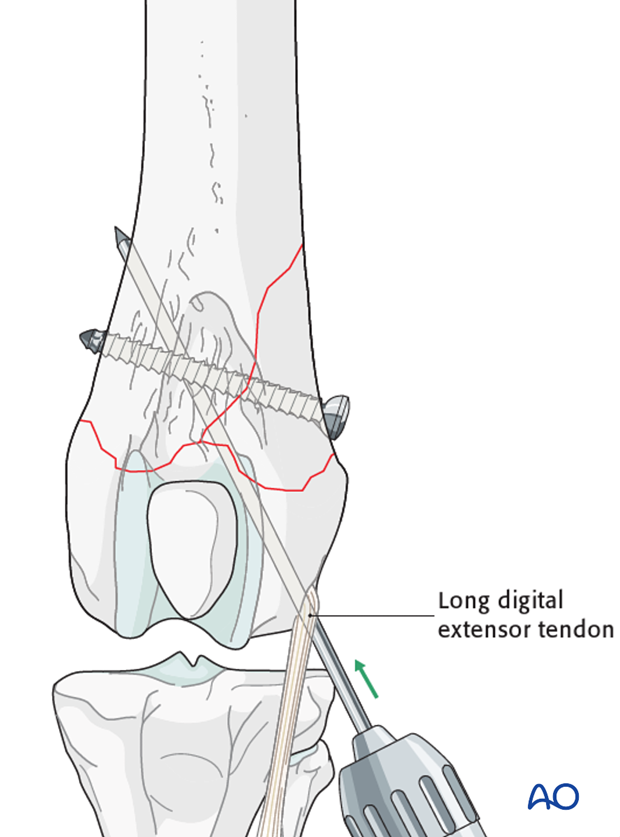
The second pin is inserted at a similar level on the medial femoral condyle.
Tip: Alternately advancing each pin into the metaphysis can aid in maintaining fracture reduction.
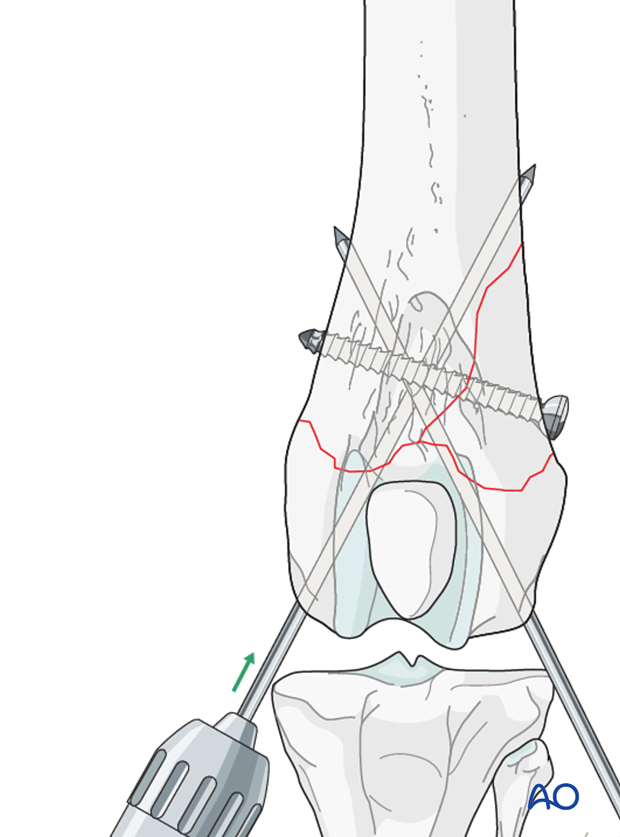
Both pins should be 40-45 degrees to the long axis of the femur.
Pins should be advanced until they penetrate the cortex proximally.
Note: Case should be taken not to penetrate the articular surface.
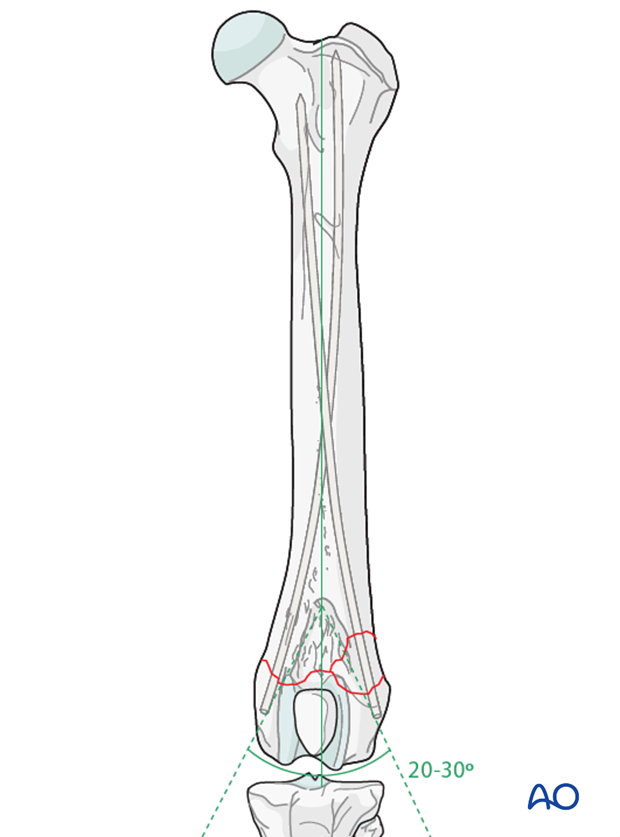
Alternative technique: Rush pinning/Dynamic cross pinning
Alternatively, the pins may be inserted using a modified Rush/dynamic cross pinning technique. In this case, the pin insertion sites are the same, except each pin is angled 20-30 degrees to the long axis of the femur. A slightly smaller diameter pin is used to achieve success with this technique.
With the modified Rush/Dynamic cross pinning technique, the pins do not penetrate the cortex of the femoral diaphysis but create friction by bending and creating a “spring like” action against the endosteum.
Due to the anatomical differences between the canine and feline femur, this technique is easier to perform in the cat, as there is less caudal curvature in the distal femur.
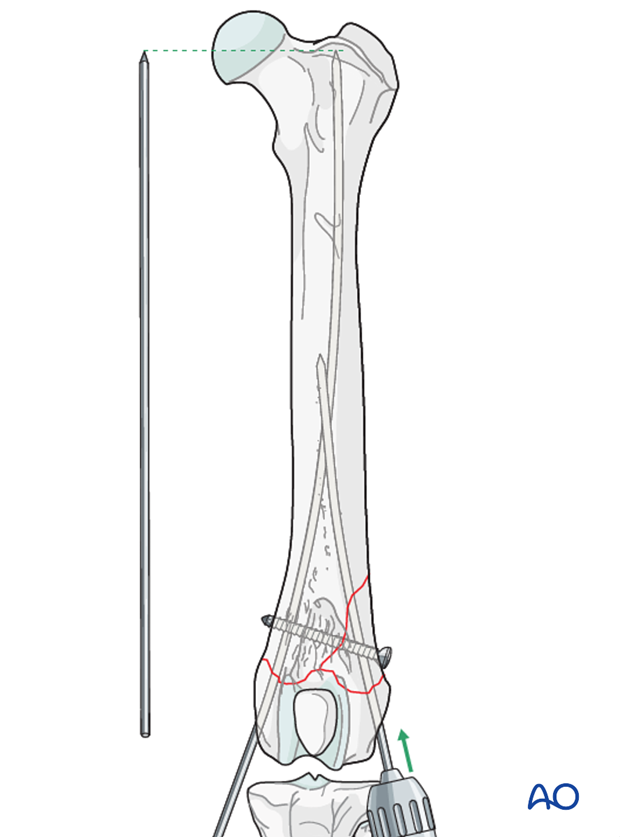
As the pins are advanced they bounce off the endosteal cortex and slide up the medullary canal. Advancement of the pins stop when they reach the proximal metaphysis.
Pearl: The depth of penetration of the pin is measured using a pin of same size as a reference, by holding it outside the bone.
Tip: Alternately advancing each pin into the metaphysis can aid in maintaining fracture reduction and should be used.
Cutting the pins
The pins can be cut flat with the bone surface, countersunk with a pin punch, or bent over and then cut short.
Note: Care should be taken if the bone is very soft, as bending the pin may cause damage to the bone.

Validation of fixation
Postoperative radiographs should be taken to assess the repair.
4. Aftercare
Activity restriction and controlled walking is indicated until evidence of bone healing is detected by radiographic examinations.
Phase 1: 1-3 day after surgery
The aim is to reduce the edema, inflammation and pain using anti-inflammatory and analgesic medications.
Passive range of motion of the hip and stifle joint can be initiated to promote mobility and joint health.

Phase 2: 4-10 days after surgery
The aim is to resolve the hematoma, edema and control pain, and prevent muscle contracture.
Anti-inflammatory and analgesic medications are still needed. Rehabilitation and integrative medical therapies can be used.
Special attention should be given to patients less than 1 year of age with a femoral fracture, as they are at risk for developing quadriceps contracture. Early controlled activity and passive range of motion is strongly recommended to help prevent this complication.
If the patient is not starting to use the limb within few days after surgery, a careful evaluation is recommended.
Phase 3: 10 days-8 weeks after surgery
Rehabilitation therapy is continued.
10-14 days after surgery the sutures are removed.
Radiographic assessment is performed every 4-8 weeks until bone healing is confirmed.

Implant removal
Implants may be removed if there is irritation or infection present, however if they are not causing problems for the patient, there is no need for implant removal.













