En bloc resection (S3 to S5)
1. Introduction
En bloc resection of a primary tumor is a significant undertaking, even in the most experienced hands. We therefore recommend referring these cases to quaternary centers with experience in primary spine tumor surgery.
En bloc resections
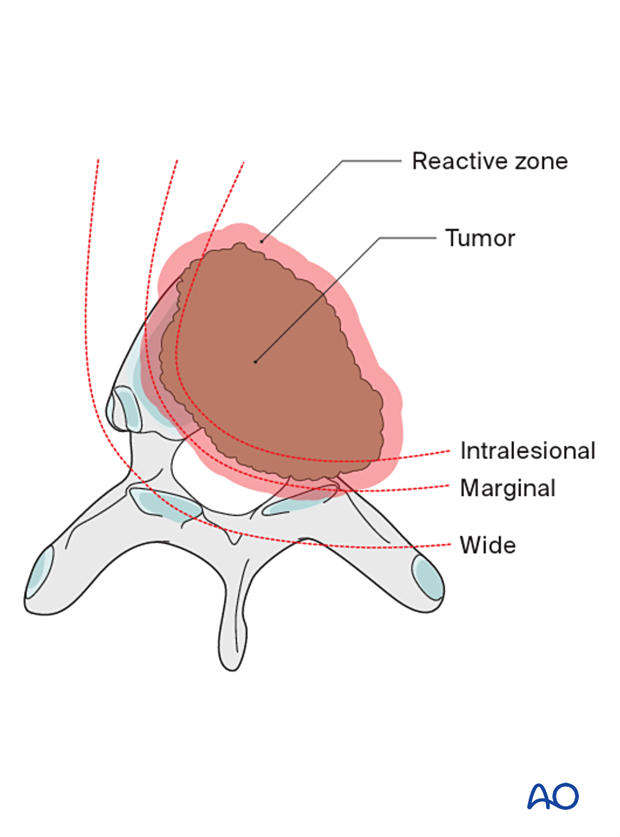
Terminology is essential in primary tumor management.
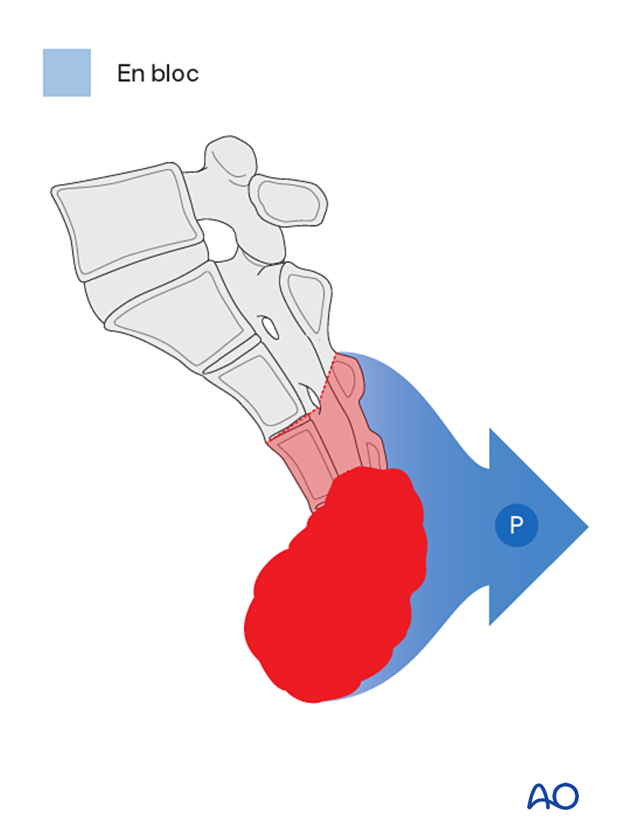
An en bloc resection refers to a surgical attempt to remove a tumor in one piece without violating it.
On the other hand, an intralesional resection or a curettage refers to a deliberate intralesional resection.
An en bloc resection needs to be associated with a pathological margin description to be correctly defined.
Four types of margins are described:
- Intralesional – resection margin is within tumoral tissue
- Marginal – resection margin is within a reactional zone or pseudocapsule (in the spine, the epidural margin is often marginal)
- Wide – resection margin is within normal tissue
- Radical – this is extracompartmental resection and, as such, does not apply to spine tumors
2. Planning
Preoperative management
Proper planning is instrumental in the management of primary spine tumors. A multidisciplinary approach may be required depending on the localization of the tumor.
A CT scan and an MRI with a spinal angiogram will assist with the final planning. 3D models, if available, can also help in the planning of those cases.
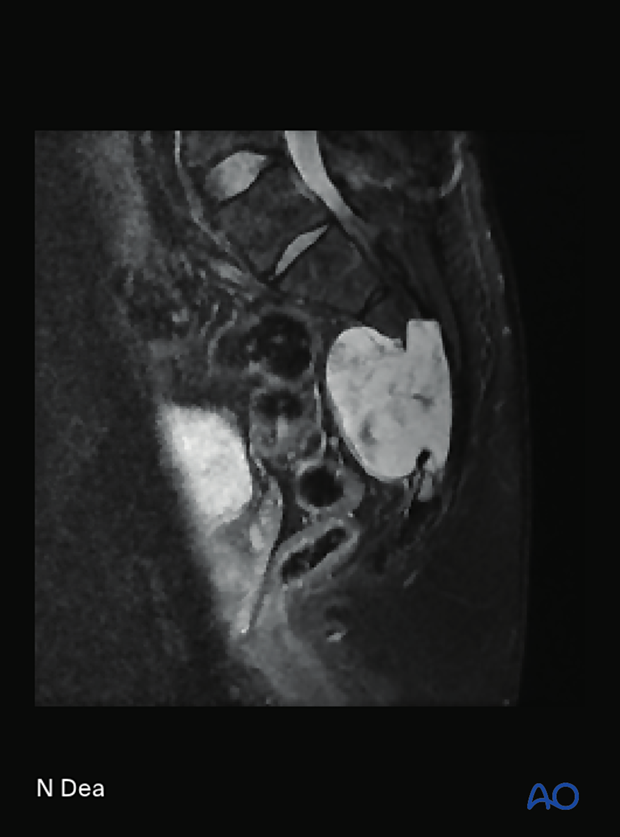
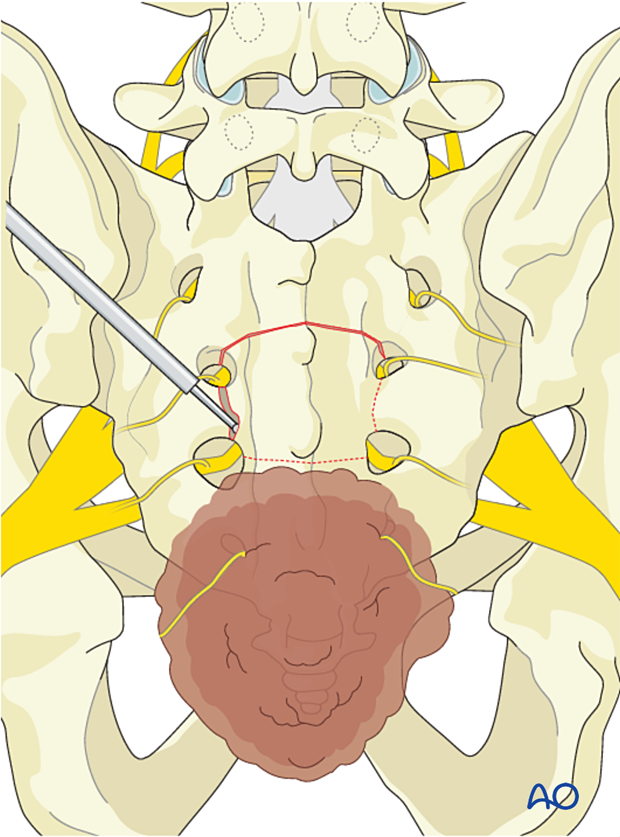
This picture shows an S3–S5 chordoma.
Embolization
Embolization procedures are recommended to reduce operative blood loss in hypervascular tumors, especially during more extensive resections.
Embolization should be considered for hypervascular tumors, such as giant cell tumors, aneurysmal bone cysts, and hemangiomas.
The role of the embolization is:
- To reduce the vascularity of the tumor
- To facilitate dissection around the tumor
- Mapping of spinal cord vascular supply
Embolization on its own may also have a therapeutic effect.
This image shows the embolization of a hypervascular tumor.

Resection strategy
A wide visualization is essential in these cases. An adequate amount of sacral lamina needs to be removed to achieve:
- Good visualization of normal and abnormal anatomy
- Safe decompression of the neural elements.
A posterior-only approach is feasible for low sacral tumors. However, if the rectum or the pelvic vessels are involved with the tumor, a posterior-only approach is not recommended.
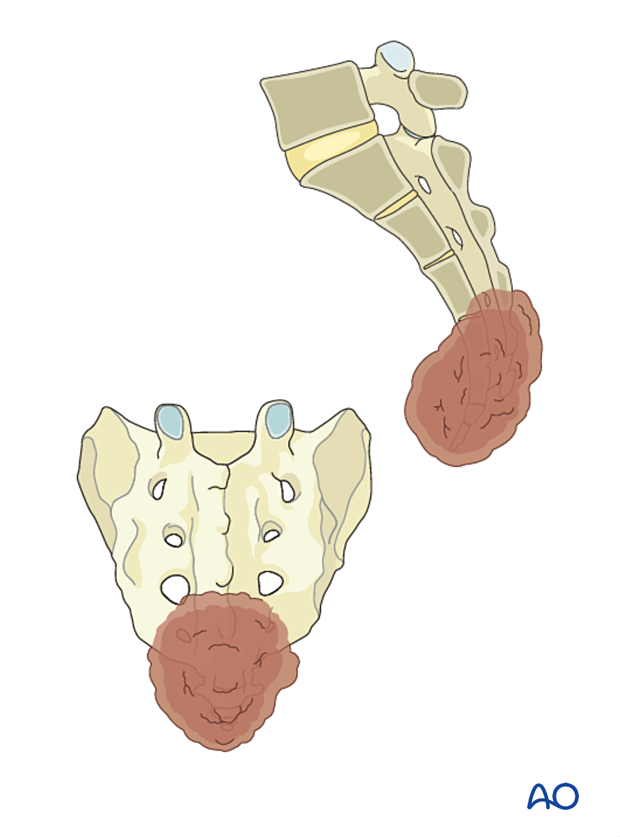
Sacral nerve root sacrifice is associated with neurological morbidity. If at least one S3 nerve root is preserved, continence will be maintained in most patients.
For a low sacral resection (as in this case), both S3 nerve roots will be preserved, and both S4 and S5 nerve roots will be sacrificed. Preservation of continence and sexual function is therefore expected.
A multidisciplinary team is needed to perform a sacrectomy. The team should include a spine surgeon, a plastic surgeon, and a general surgeon.
Reconstruction strategy
A distal sacrectomy does not require lumbopelvic reconstruction.

Case-based scenario
Every case is unique.
To illustrate the surgical principle of a posterior en bloc sacrectomy of a sacral tumor, we will use a low sacral tumor located in S4–S5.
3. Patient preparation and surgical access
Patient preparation
The patient is placed prone on a Jackson table. Regular prone positioning or a split leg attachment can be used. The potential advantage of a split leg attachment is that a third surgeon can work between the legs to connect the posterior and anterior exposure.

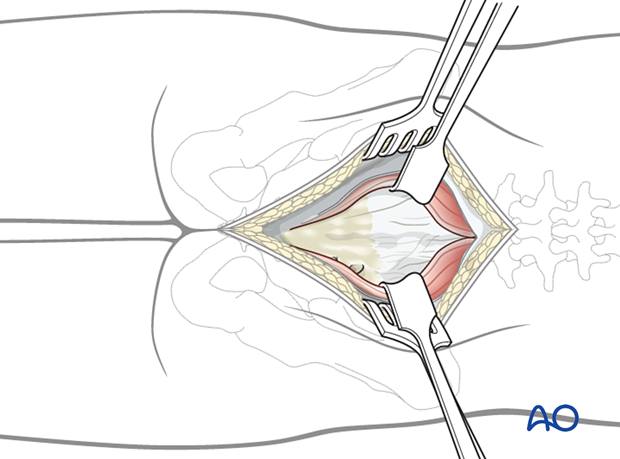
Surgical access
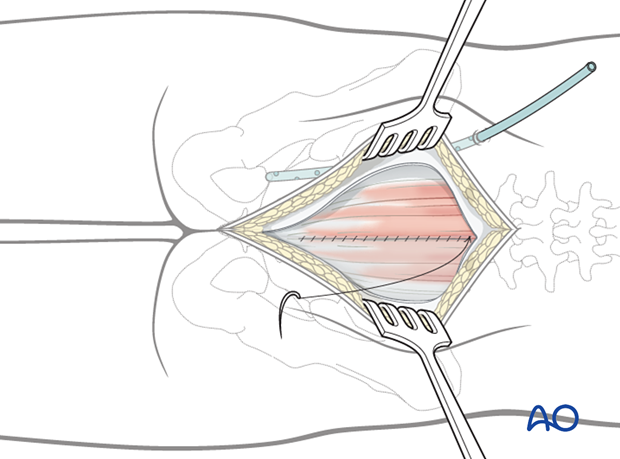
A posterior midline approach to the sacrum is performed.
A wider dissection will typically be performed for primary tumors compared to a trauma case.
Great care should be taken not to enter the tumor during exposure.
Review preoperative images to verify whether the tumor invades the lamina. In such cases, exposure of the posterior elements should be performed with great care, and the use of Cobb elevators should be avoided.
4. Tumor resection
Sacral laminectomy
Remove intact sacral lamina according to the preoperative planning using a high-speed burr or a Kerrison rongeur.
In this case, the spinal canal can be entered via the dorsal S3 foramen, and a laminectomy of S2 only can be performed.

Dissection should progress from normal to abnormal tissues to protect normal neurological elements and facilitate dissection.
Soft-tissue dissection
Dissect the posterolateral soft tissues around the tumor in normal tissue planes.
Divide the sacral tuberous and the sacral spinous ligaments.
To decrease the risk of local recurrence, ensure a liberal piriformis muscle margin.
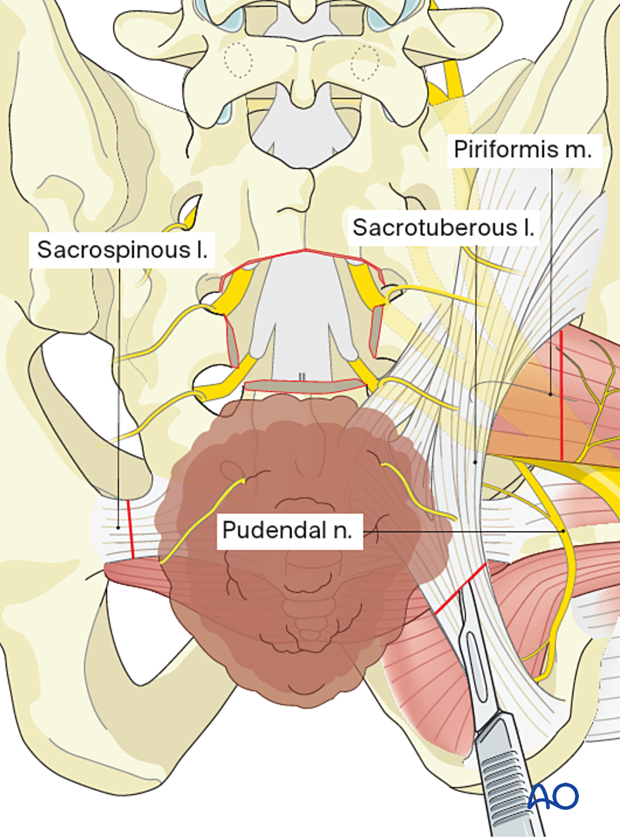
Dissect the rectum from the ventral side of the tumor. A careful review of preoperative imaging to ensure no rectal and pelvic vessel involvement is important. The assistance of a general surgeon is also preferred for this part.

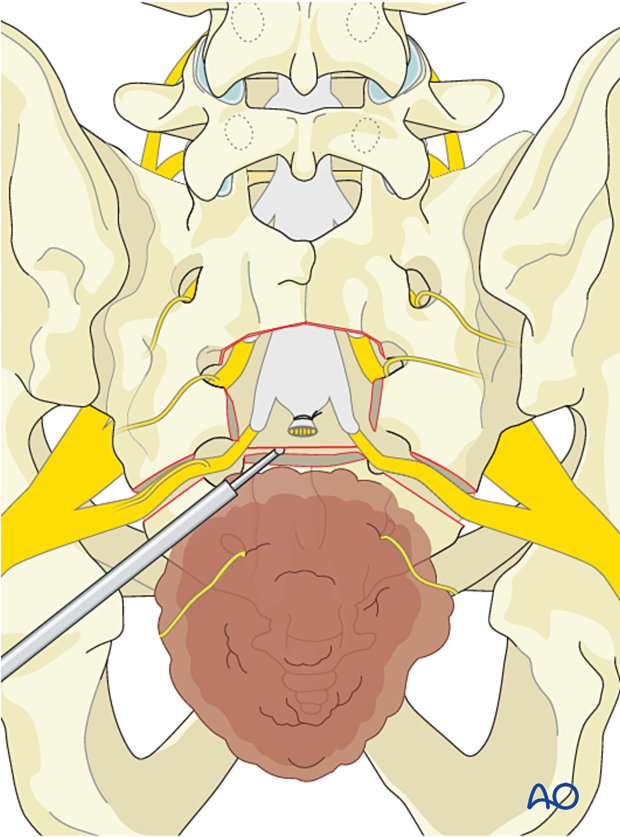
Thecal sac ligation
Ligate the thecal sac at the chosen level.
In this case, just distal to the S3 nerve root takeoff.

Remove the bone by following the S3 nerve root out laterally to visualize and protect it.

Transverse sacral osteotomy
Protect the visceral organs by inserting a sponge in the previously dissected presacral plane.

With an osteotome or bone scalpel, perform the transverse osteotomy just distal to the nerve root, as illustrated. Then continue the osteotomy laterally to the ventral S3 foramen.
Tumor delivery
Deliver the tumor.

Closure
Perform a multilayer closure as described in the approach.
Even a low sacrectomy has a high chance of deep wound infection.
To decrease the risk of wound infections, a gluteal advancement flap may be considered. This is typically performed by the plastic surgeon.
Intrawound vancomycin can be applied to decrease the risk of postoperative wound complications.
5. Aftercare
Patients are mobilized progressively without any direct pressure on the wound as directed by the plastic surgeon.
Patients with intact neurological status are made to stand and walk on the first day after surgery.
Patients can be discharged when medically stable or sent to a rehabilitation center if further care is necessary.
Throughout the hospital stay, adequate caloric intake of a high-quality diet should be monitored.
Patients are generally followed with an MRI every 6 months for tumor surveillance.
Some primary benign tumors of the spine can recur years after surgery, and long-term tumor surveillance is important.













