Kyphoplasty
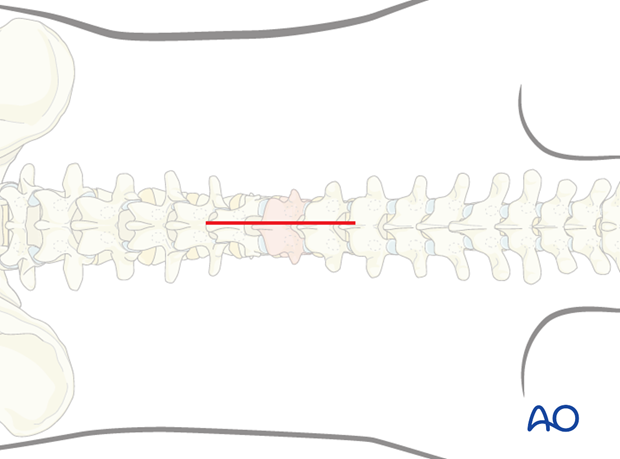
1. Patient positioning and surgical approach
For this procedure the patient is placed in the prone position and the posterior midline approach is used.
2. Kyphoplasty
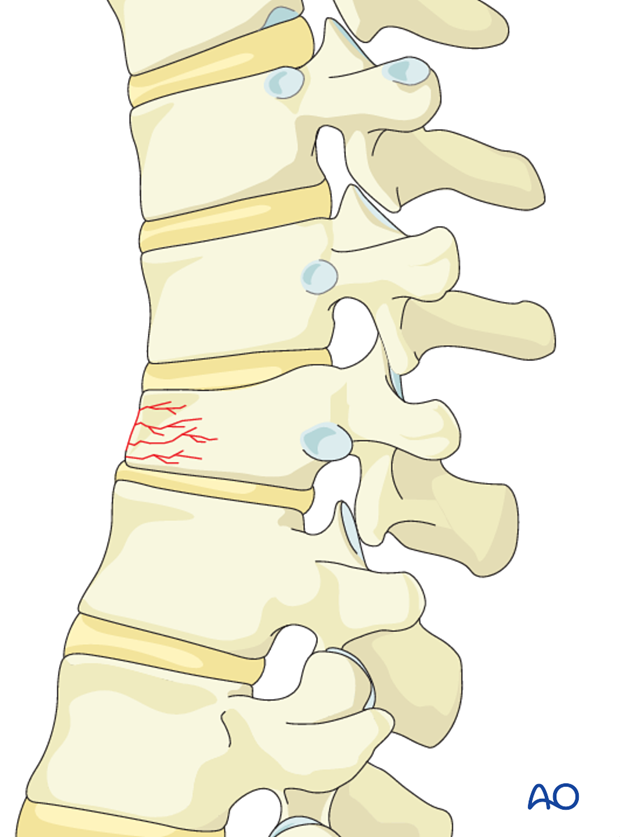
Depending on the amount of wedging and vertebral configuration, the procedure will be performed uni- or bi-laterally.
Using radiography, ensure that planned instrument trajectories end up inside the vertebral body. In cases with high degree vertebral body compression, this may not be possible.
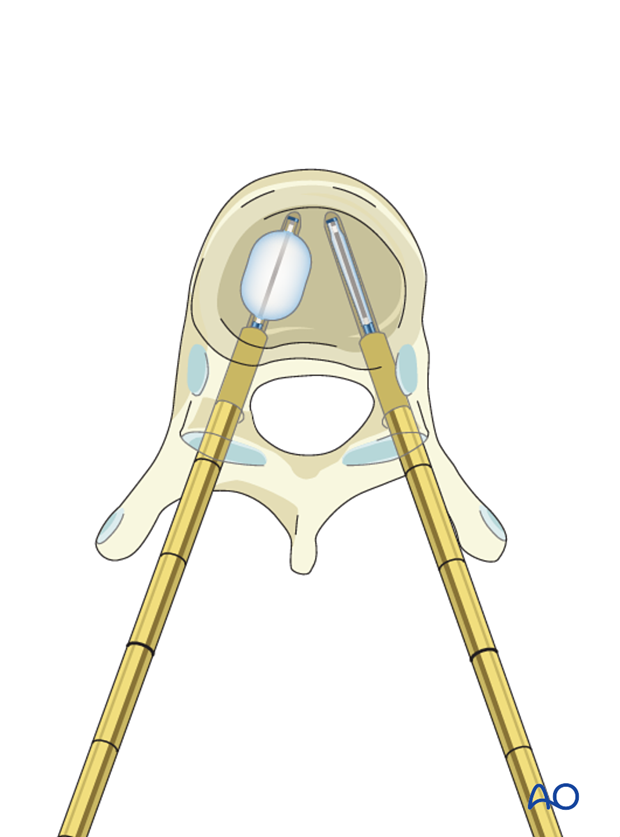
Insert a guide wire through the pedicle, into the vertebral body under radiographic control
Care must be taken not to penetrate the vertebral body anteriorly. The preferred end-position is paramedian in the anterior third of the body.
A cannula is gently inserted over the guide wire and the guide wire removed.
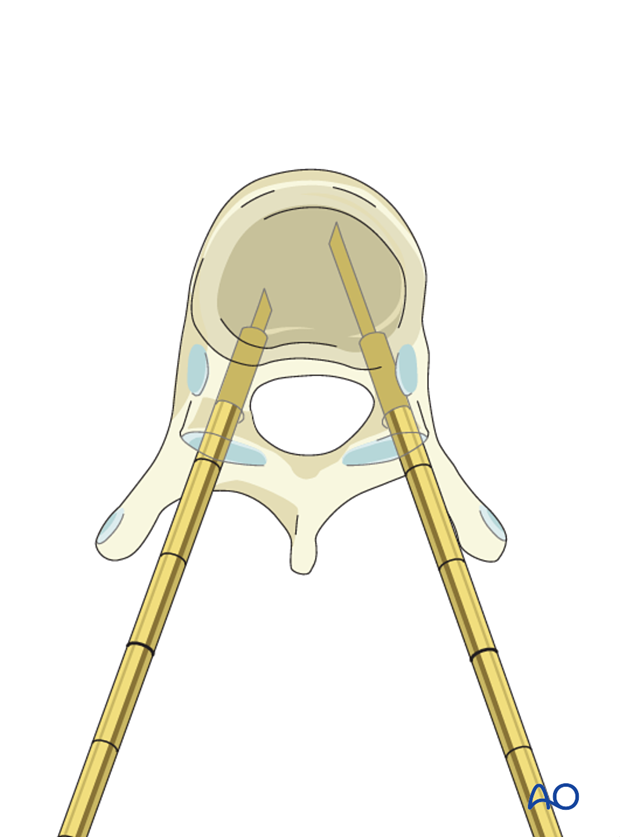
A drill is then inserted until the anterior body cortex to prepare an initial space for the balloon insertion.
The location of the cannula is verified by radiography.
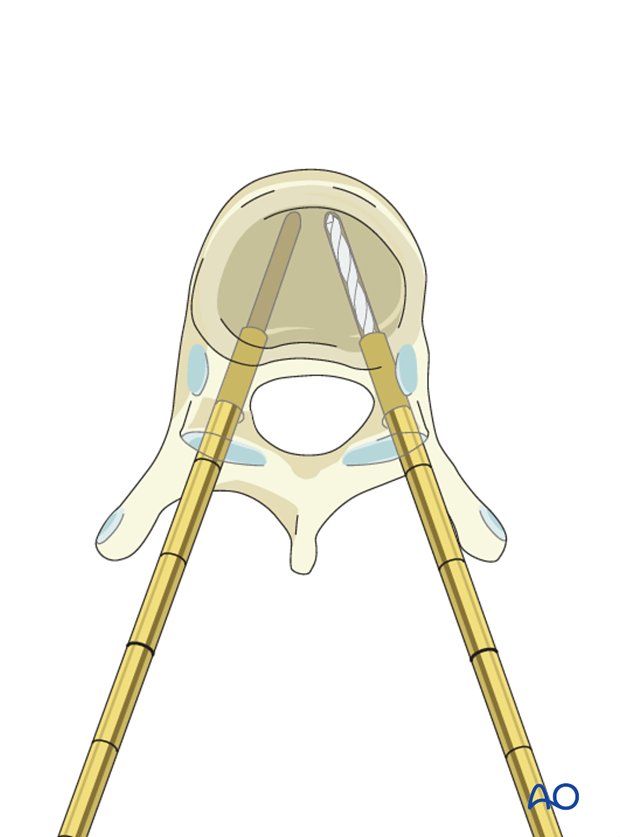
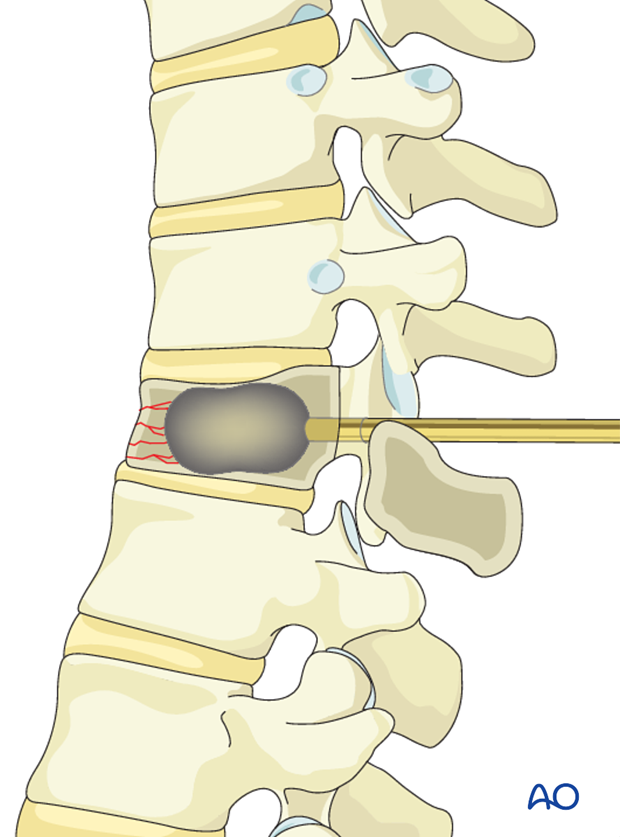
If the vertebra is significantly wedge shaped, an inflatable balloon is inserted though the cannula and carefully inflated to create a space between the endplates allowing for the cement column. Vertebral height restoration may not be possible and is typically not required to alleviate pain.
The balloon is carefully deflated and removed, leaving a space in the middle of the vertebra.
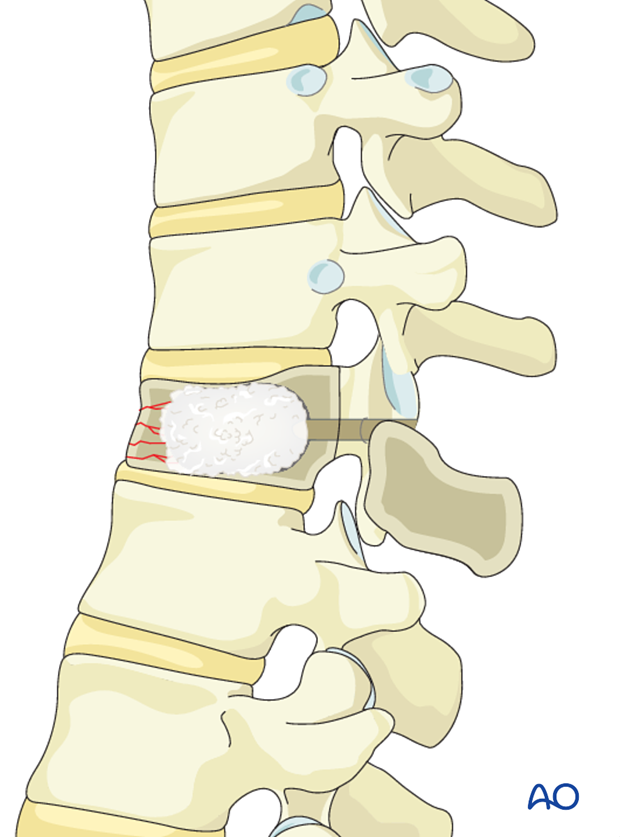
The cement is prepared and its consistency monitored until it's adequate for injection.
Carefully inject the bone cement (bilaterally), preferably without any pressure. The space is filled from anterior to posterior as the cannula is slowly retracted. The process is closely monitored to ensure that no cement leaks into unwanted areas such as the ventral venous system or epidural space.
Although complete filling of the vertebral body is the goal, it is not always possible or necessary.
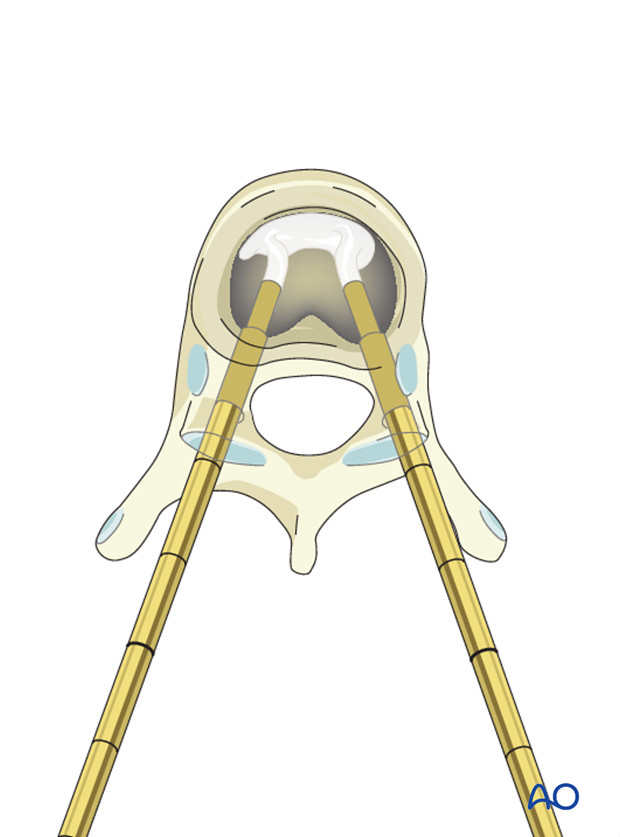
Once the cement is settled, the cannulas are removed.
Aftercare
The patient is encouraged to sit 1h following surgery, and to walk 2 hours following surgery.
After 24 h the patient can gradually start returning to normal activities.
3. Aftercare
Patients are made to sit up in the bed on the first day after surgery. Bracing is optional but preferably omitted for patient comfort. Patients with intact neurological status are made to stand and walk on the first day after surgery.
Patients can be discharged when medically stable or sent to a rehabilitation center if further care is necessary.
During admission adequate caloric intake of a high-quality diet should be monitored.
Patients are generally followed with periodical x-rays and (optionally) MR imaging at 6 weeks, 3 months, 6 months, and 1 year to monitor for tumor recurrence and hardware failure.
Postoperative radiation is required to avoid tumor recurrence. SBRT is usually initiated within two weeks following surgery. Conventional radiotherapy is usually initiated 2-4 weeks after surgery to reduce the risk of wound healing disturbances.
The radiation modality is selected based on tumor histology and history of prior radiation.













