Anterior corpectomy and stabilzation
1. Introduction
Preoperative planning
Based on CT and MRI imaging, a plan should be prepared to determine:
- The size and optimal location of implants used
- Whether spinal cord decompression is necessary and if so, the amount of tissue to remove in order to achieve enough spinal cord decompression
Every case will be unique, and we will here illustrate just one example.
Anterior fixation is a useful technique for anterior decompression and reconstruction of the anterior column.
Anterior stabilization can be used without posterior stabilization in patients without tumor extension into the posterior element.
In very rare cases when resection of both anterior and posterior column is required in the surgical management of metastatic spine disease, bilateral posterior fixation above and below the anterior construct should be used.
From anterior, direct decompression from tumor or bone material can be performed directly without mobilization of the neurological structures. Visualization of the dura allows direct confirmation of complete decompression.
Evaluation of potential anatomic variations in the course of the vertebral artery using preoperative imaging is mandatory. Unidentified anatomical variations may increase the risk of compromising the artery during decompression.
Use of dexamethasone
Administration of dexamethasone (10 mg bolus, 4 mg every 6 hours) is recommended as soon as ESCC causing neurologic deficit is diagnosed. Dexamethasone should be stopped or tapered as soon as spinal cord decompression is completed.
Embolization
Embolization procedures are recommended to reduce operative blood loss in hyper vascular tumors, especially for larger resections.
Neurological evaluation
The preoperative neurological assessment must be carried out as described in the Neurological Evaluation.
2. Patient positioning and surgical approach
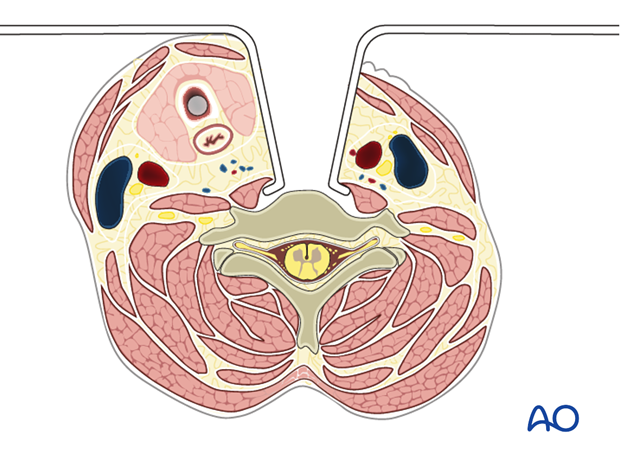
For this procedure the patient is placed in the supine position and the anterior approach to the cervical spine is used.
3. Corpectomy
Discectomy
Prior to performing the discectomy, the level is confirmed with intraoperative fluoroscopy.
The following landmarks are identified:
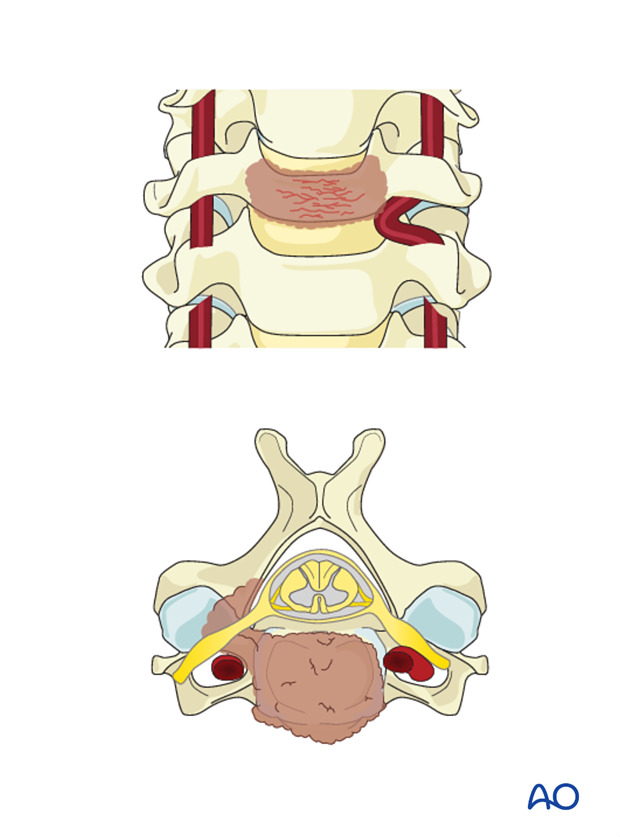
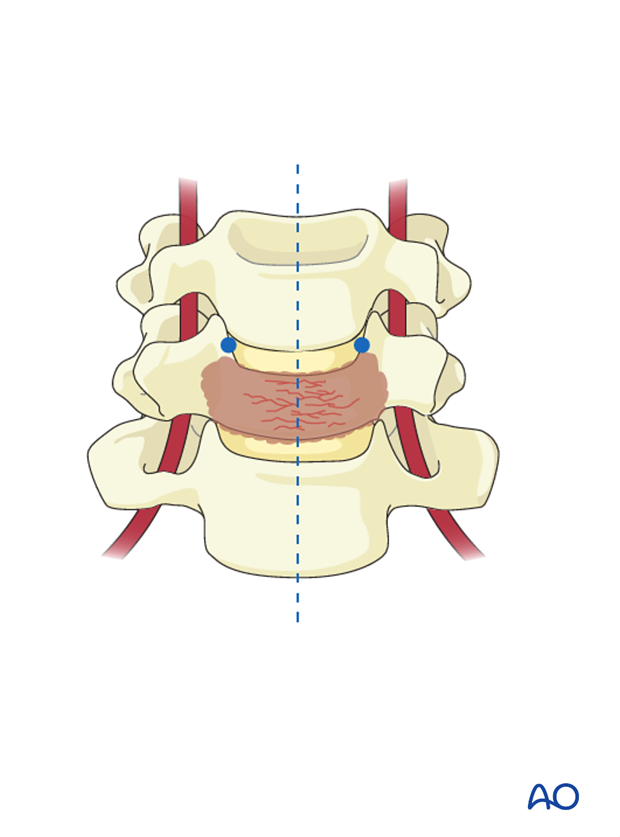
- Midline
- Uncovertebral process
The midline will dictate the AP orientation of the discectomy.
The uncovertebral processes dictate the lateral borders of the discectomy, establishing the safe area from the artery. This will leave a 3mm safe zone to the normal anatomy of the vertebral artery.
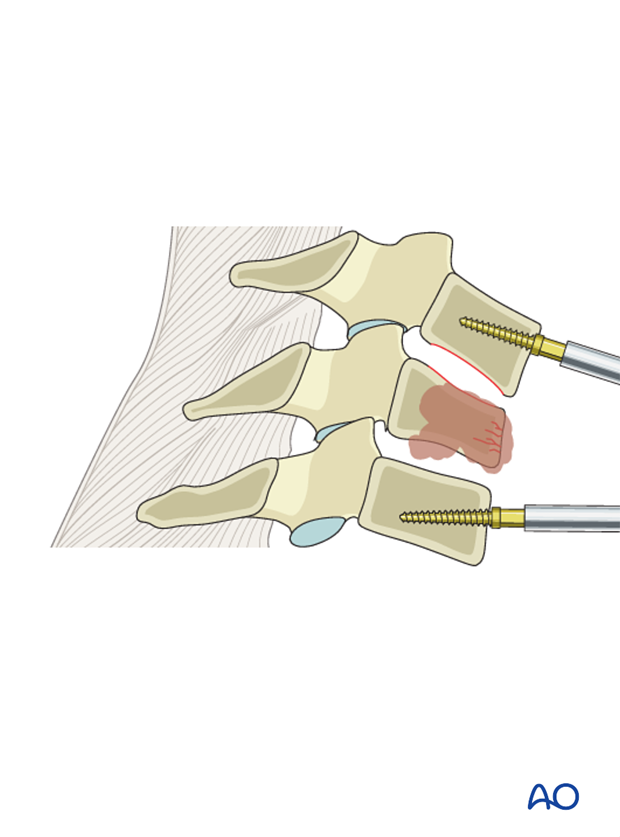
A small blade is used to open the annulus from uncinate to uncinate as close as possible to the endplates.
Pearls
- To help stop a slipping blade, a suction tip is held in place in the direction the blade is cutting.
- To prevent accidental durotomy and spinal cord transection, the annulotomy should not go deeper than 11 mm.

The discectomy continues using a pituitary rongeur forceps to remove the annulus and small curettes to scrape the endplates.
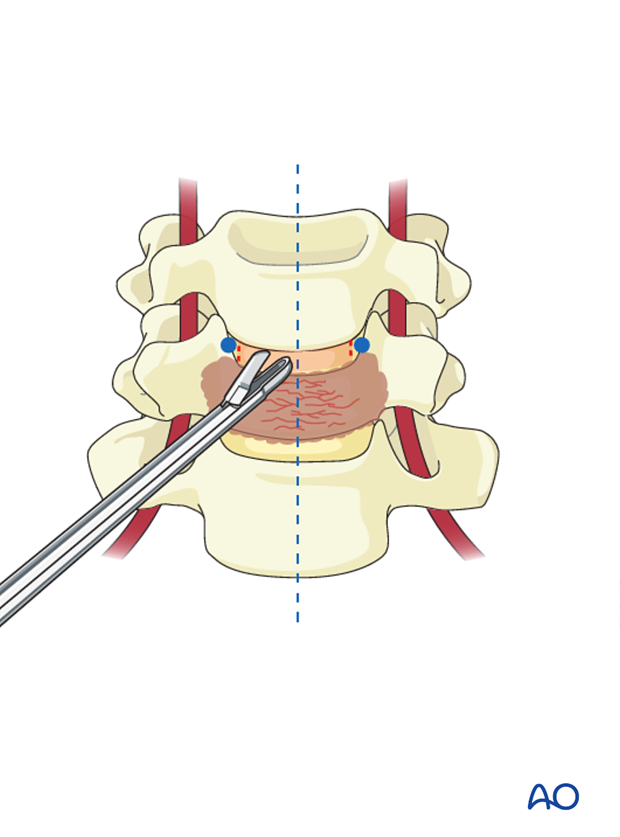
The use of a distractor or an intervertebral distractor will facilitate the removal of the posterior half of the disk and visualize the posterior longitudinal ligament.
Care should be taken not to over distract.
A complete discectomy will allow good visualization of the spinal canal and facilitate tumor removal where necessary.
Prepare the area for the stable placement of a cage by removing cartilage from the endplates.
A small probe is used to ensure that no fragments are left in the area behind the vertebra which is not directly visualized, or in the foramen.
Prior to performing a full corpectomy, both the superior and inferior discs are removed to define the safe depth of bone resection.
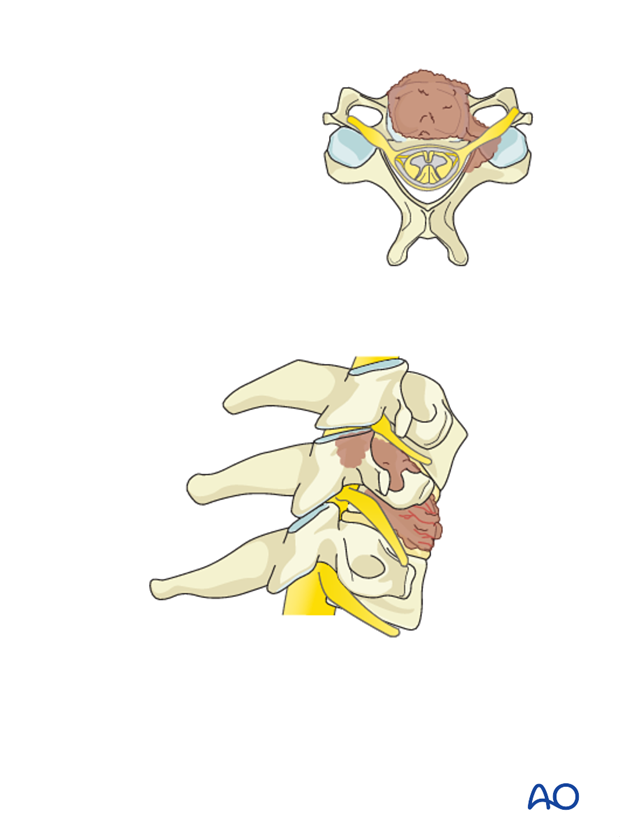
Laterally the corpectomy is limited by the medial border of the uncovertebral process.
The uncovertebral processes indicates the lateral borders of the corpectomy, establishing the safe area from the artery. This will leave a 3mm safe zone to the normal anatomy of the vertebral artery.
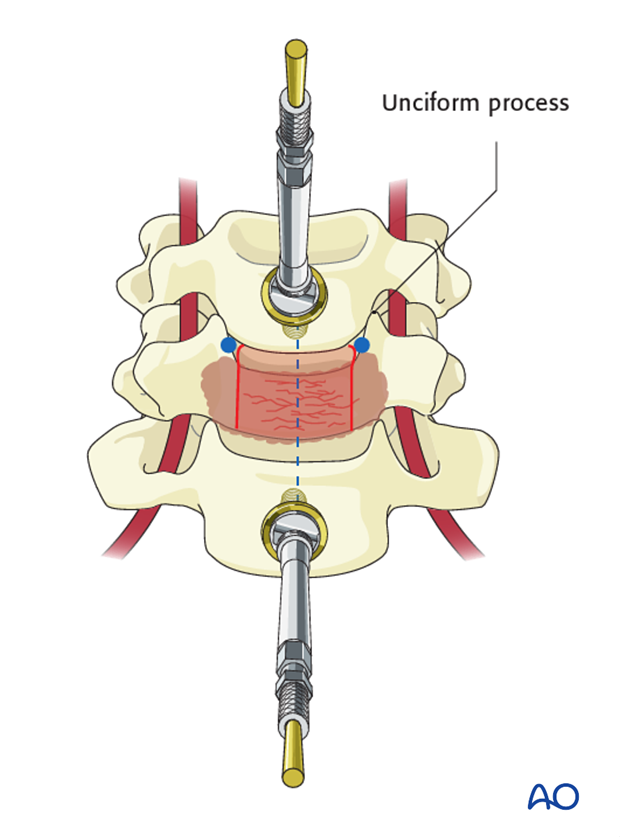
Pitfall: As the surgeon is standing lateral to the midline of the patient, the true midline may be difficult to recognize and there is a tendency to direct the decompression to the contralateral side as shown in the illustration. This may lead to an incomplete decompression.
To prevent this, verification of anatomical landmarks using intraoperative imaging may be useful.
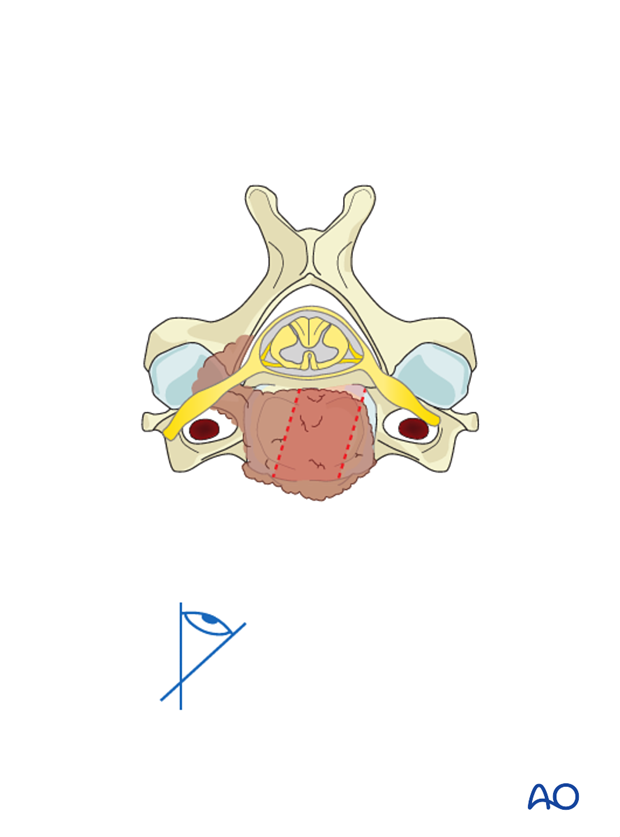
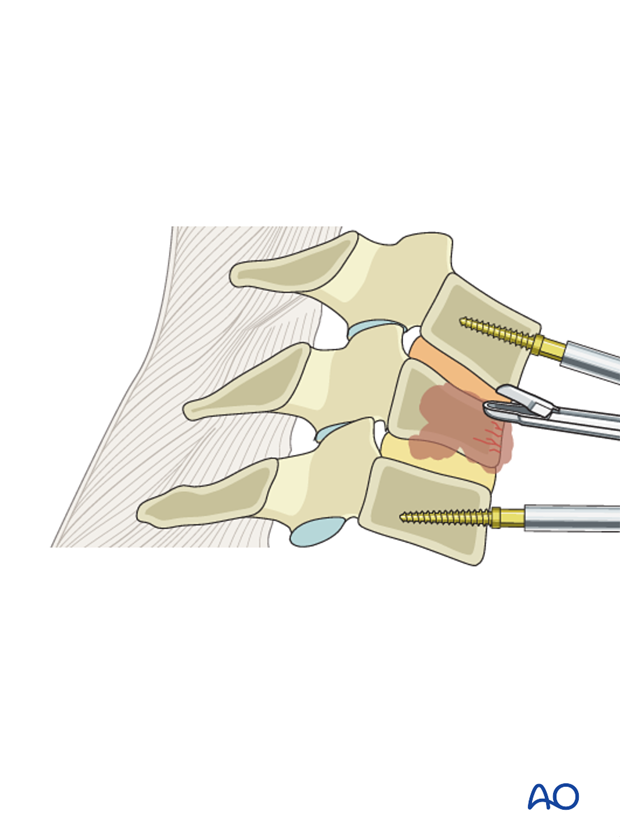
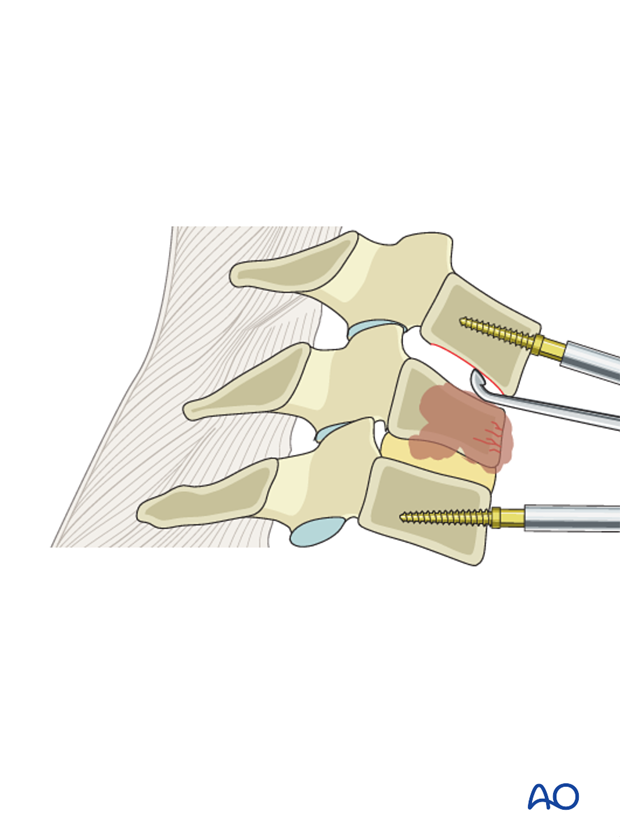
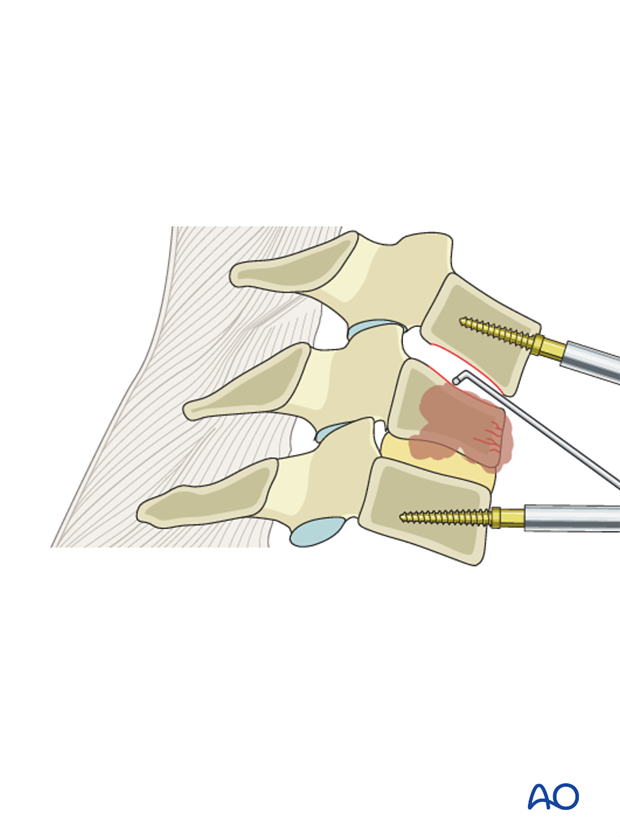
At this point, the tumor is removed using a combination of Leksell rongeurs, osteotomes, pituitary rongeurs, and suction.
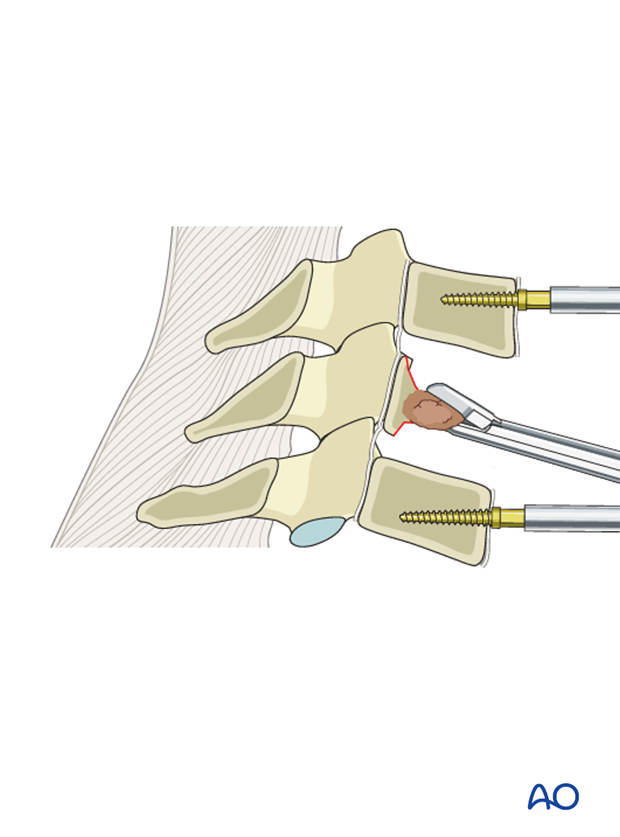
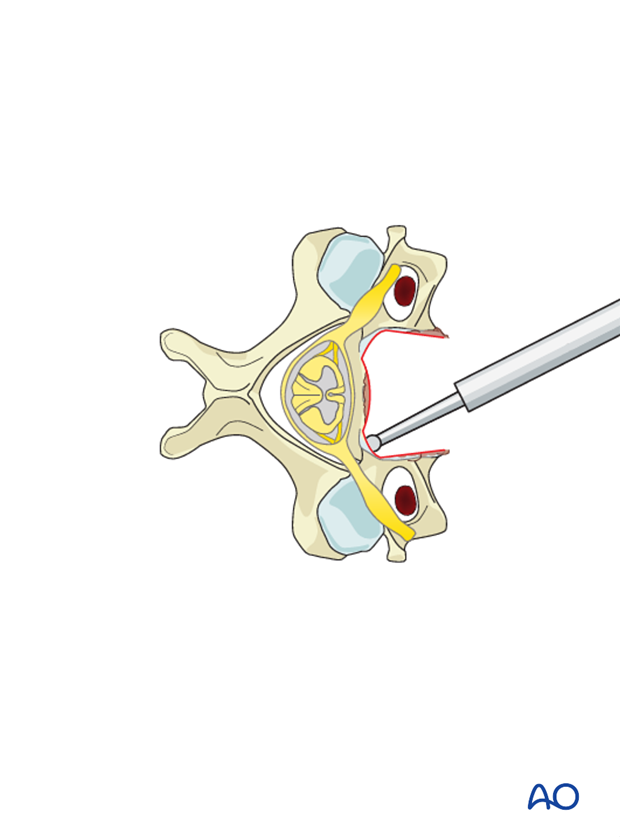
The spinal canal is exposed by the resection of the posterior wall of the vertebral body.
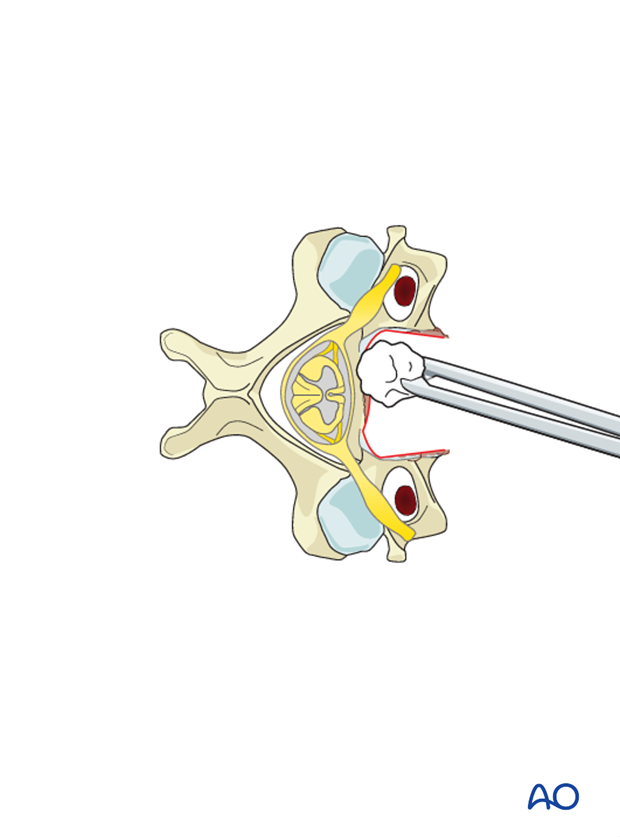
The remaining posterior cortex should be thinned with the burr to an eggshell. Retropulsed tumor fragments can be removed with curettes and thin footplate Kerrison punches.
Pearl: Care should be taken to protect the dura. Epidural venous bleeding can be troublesome at times, so meticulous hemostasis with bipolar cautery, cottonoid patties, and hemostatic adjuncts can be helpful.
4. Anterior fusion following corpectomy
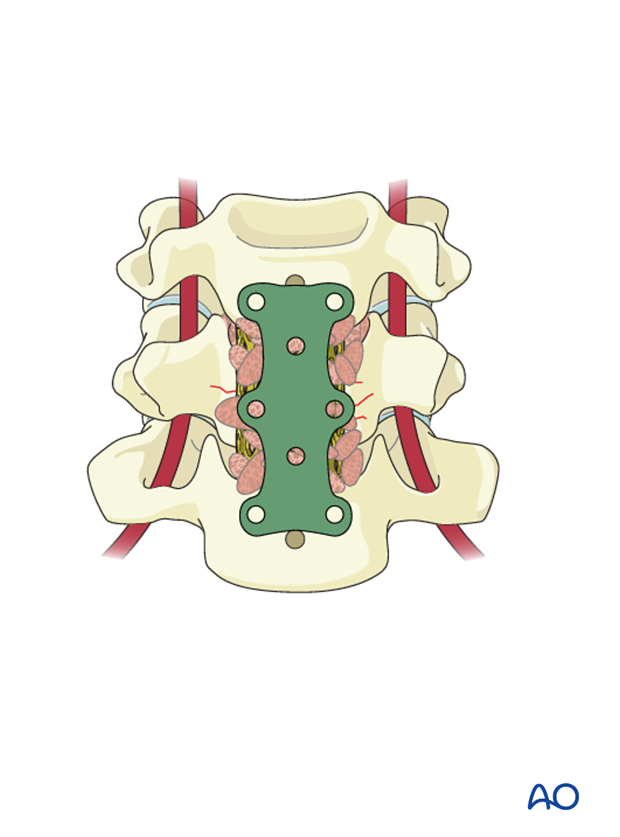
Anterior reconstruction of the disc space or vertebral body following a complete corpectomy should be performed using a cage and plate.
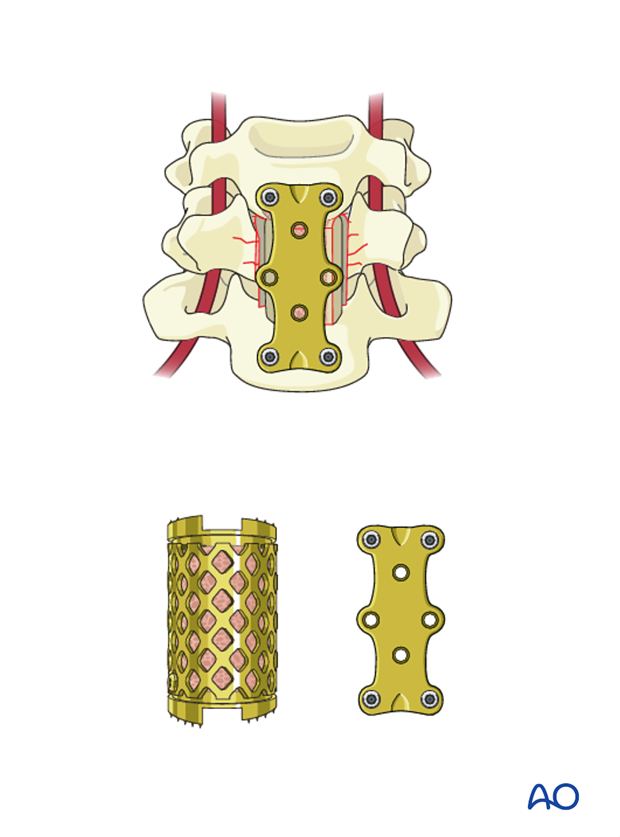
Reconstruction using Mesh cage and plate
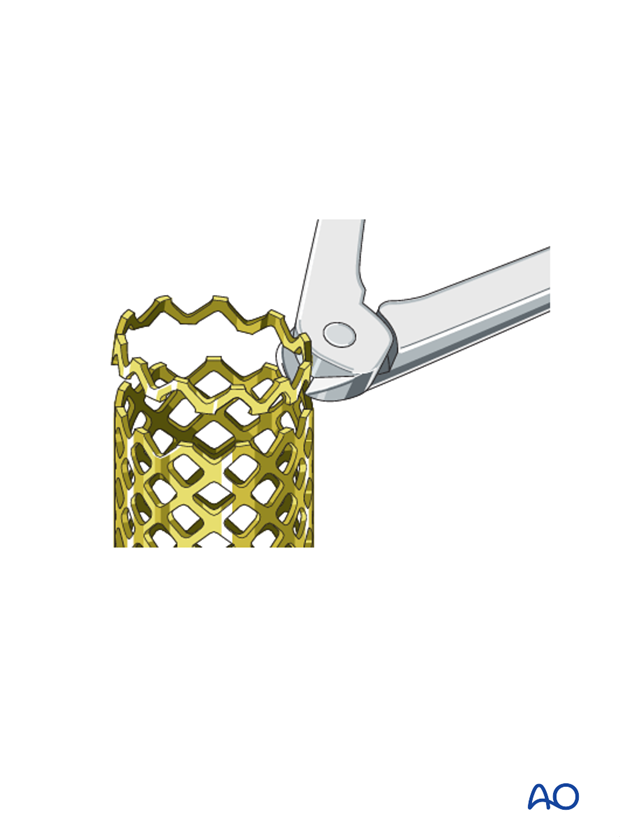
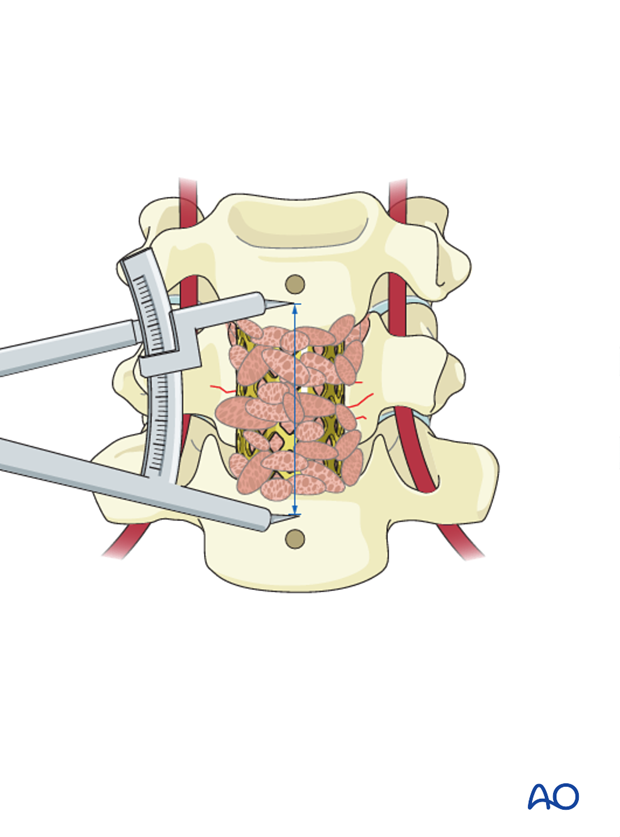
The corpectomy defect is measured using a caliper.
A mesh cage of the largest possible diameter is cut to a corresponding length.
Depending on surgeon’s preference, the cage can be filled with graft material, although it is well advised to consider the life expectancy of the patient and whether achieving a bony fusion will add to quality of life. Obtaining autologous iliac crest bone graft is strongly discouraged as it will add to patient discomfort.

The cage is inserted and tapped into its final position under lateral fluoroscopic monitoring.
The Caspar pins are removed.

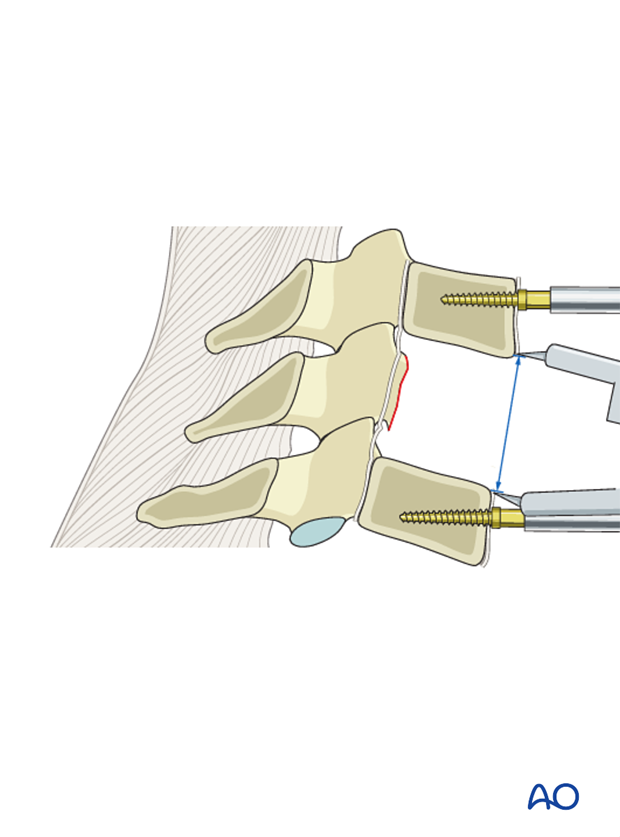
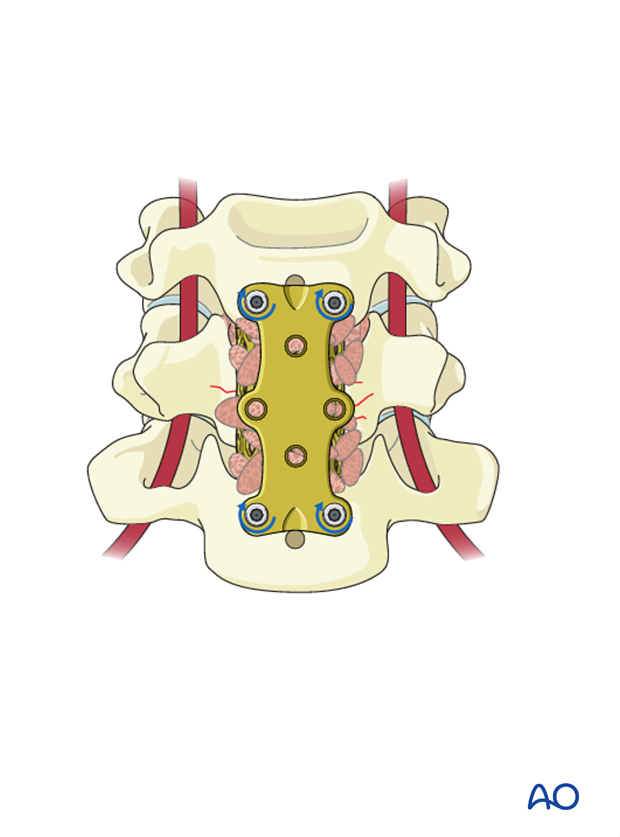
5. Anterior plating
When choosing the plate length, care must be taken to prevent it from damaging the mobile disks above and below.
Ideally the plate would extend as little as possible above and below the endplates of the tumor level.
The plate is bent to accommodate the patient’s lordosis and fixed in place with two temporary pins placed in holes diagonal to each other.
The appropriate positioning of the plate is verified in AP and lateral views.
Variable angle plates with locking screws are also an option if thought to be necessary.
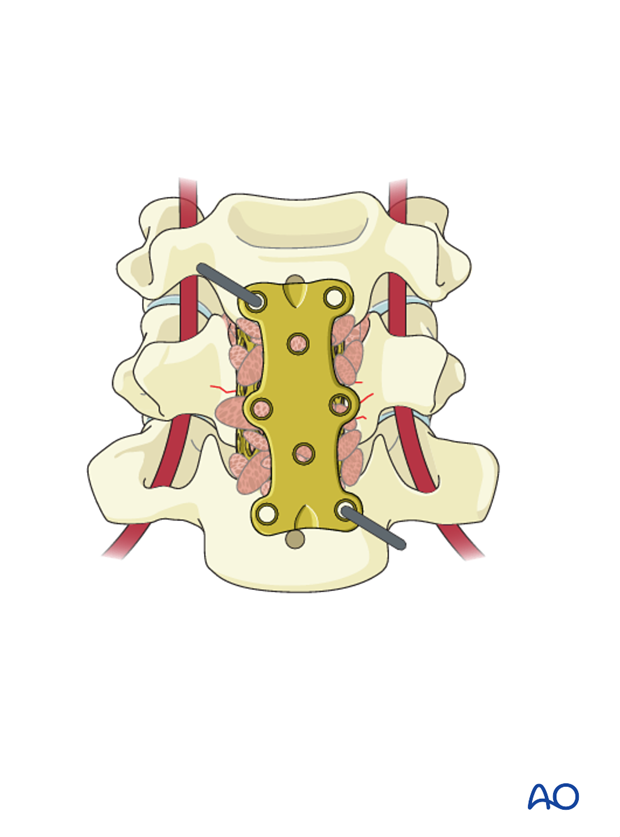
Malrotation of the plate is commonly seen on the AP view and can be adjusted by temporarily removing one pin while adjusting the rotation.
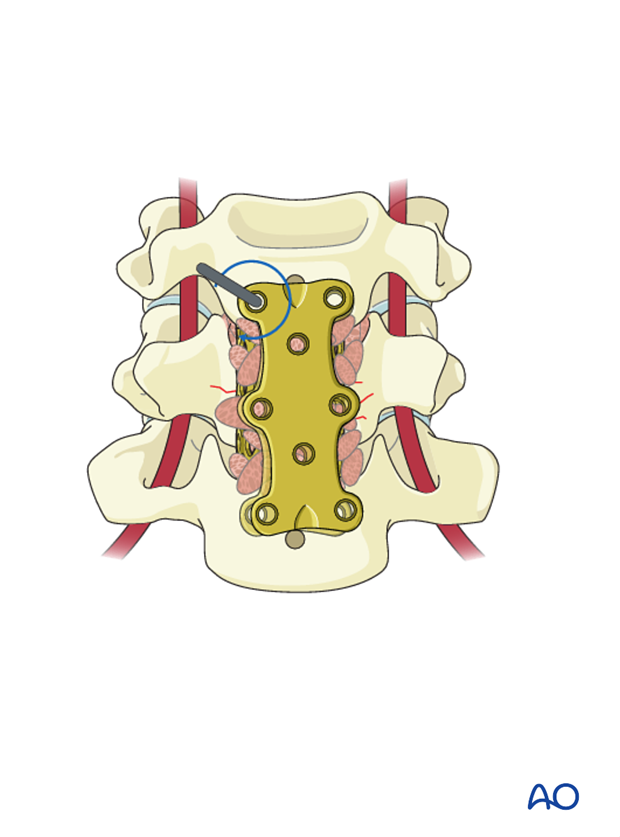
Based on a preoperative measurement of vertebral body depth, screw holes are prepared with the appropriate depth. This is performed under lateral fluoroscopic guidance. Screws of appropriate length are selected and …

… applied but not fully tightened until all screws have been inserted.
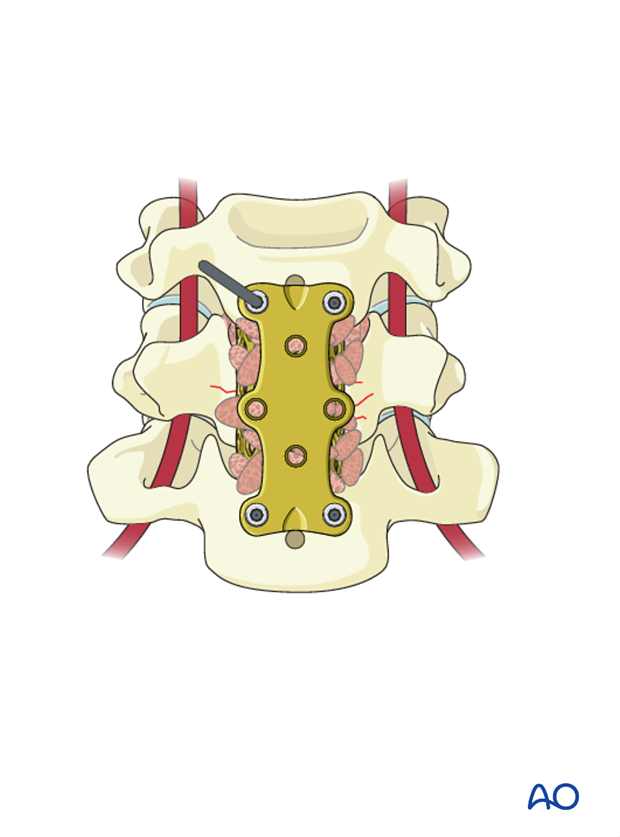
Final hardware positioning is verified in lateral and AP view.
6. Aftercare
Patients are made to sit up in the bed on the first day after surgery. Bracing is optional but preferably omitted for patient comfort. Patients with intact neurological status are made to stand and walk on the first day after surgery.
Patients can be discharged when medically stable or sent to a rehabilitation center if further care is necessary.
During admission adequate caloric intake of a high-quality diet should be monitored.
Patients are generally followed with periodical x-rays and (optionally) MR imaging at 6 weeks, 3 months, 6 months, and 1 year to monitor for tumor recurrence and hardware failure.
Postoperative radiation is required to avoid tumor recurrence. SBRT is usually initiated within two weeks following surgery. Conventional radiotherapy is usually initiated 2-4 weeks after surgery to reduce the risk of wound healing disturbances.
The radiation modality is selected based on tumor histology and history of prior radiation.













