Cervicothoracic junction - posterior fixation
1. Introduction
A B3 type injury is a high impact injury in a stiff spine resulting in hyperextension of the cervicothoracic junction. Most fractures are associated with severe cord injury and complete neurologic deficit. More than 50% of the fractures are associated with dural injuries and cerebrospinal fluid leak. Associated esophagus, trachea, or vertebral artery dissections at this level are common. Management is aimed at resuscitation, control of life threatening organ injuries, spinal stabilization, and rehabilitation.
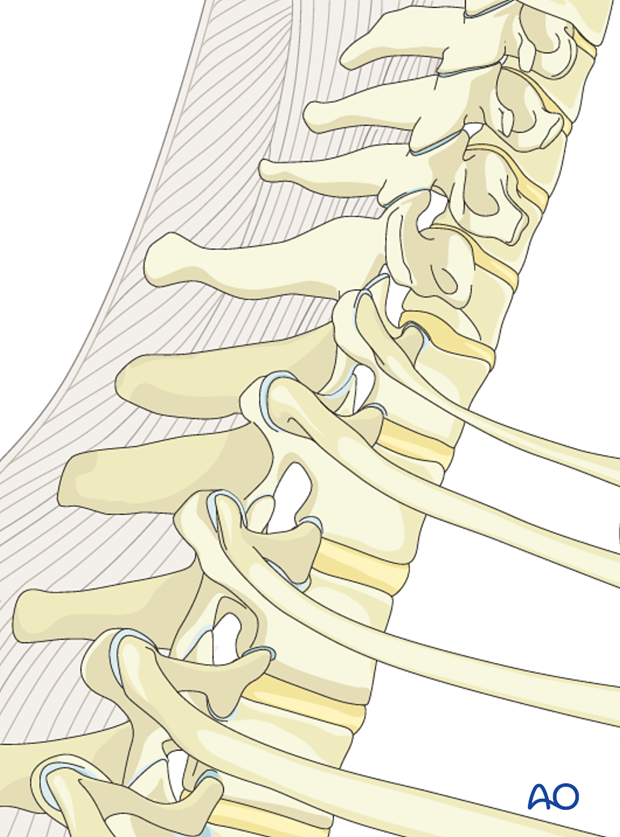
The cervico thoracic junction has a specific biomechanical behaviour. This is due to the sudden change from the extremely flexible cervical spine, to the more rigid thoracic spine.
The thoracic spine has a shorter elastic zone due to:
- The rigid rib cage
- The coronal orientation of the facet joints
- The overlapping of the spinous processes.
Biomechanically the cervico thoracic junction is vulnerable to kyphosis and sheer forces. Usually a long construct (2-3 levels above and 2-3 below the dislocation) is necessary to achieve adequate stability. That is why the anterior alone constructs at this level are not recommended because of high failure risks.
The anterior approaches might be difficult because of complex anatomy involving numerous essential anatomical structures at this level.
2. Positioning and approach
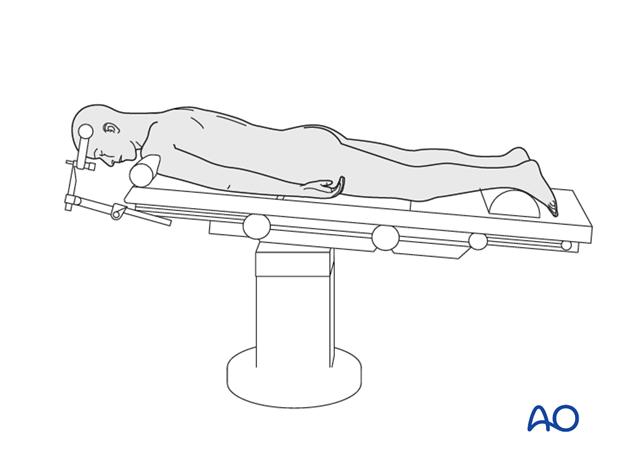
Posterior fixation is achieved with the patient in the prone position, through the posterior access to the thoraco cervical junction.
3. Screw insertion
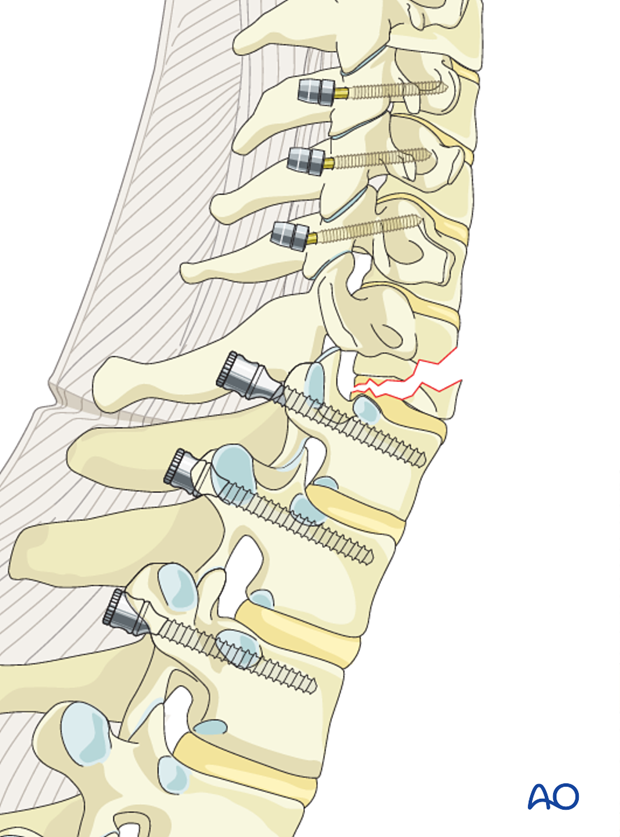
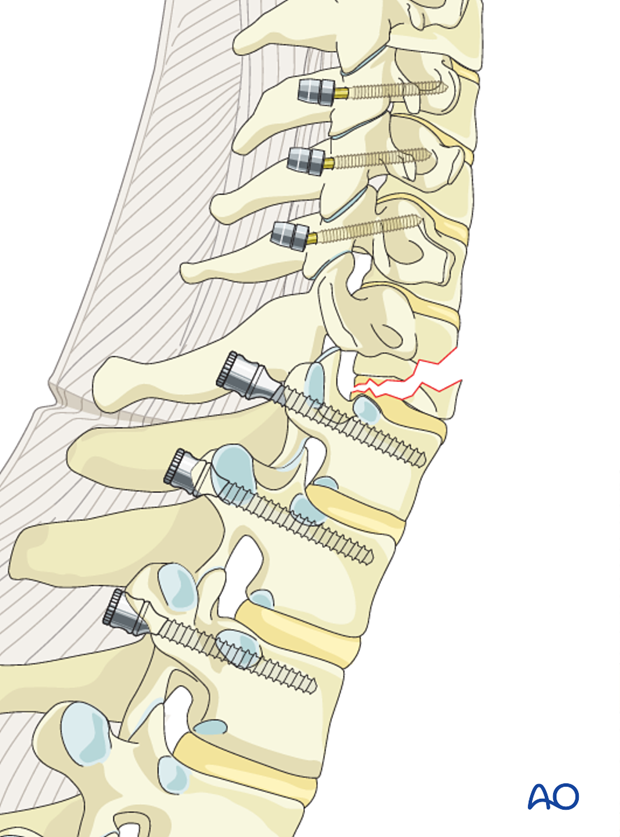
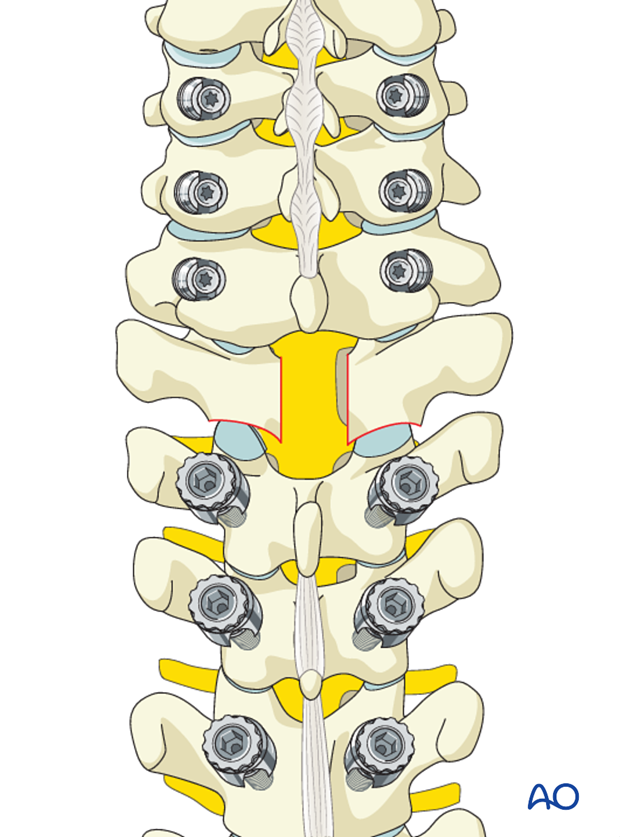
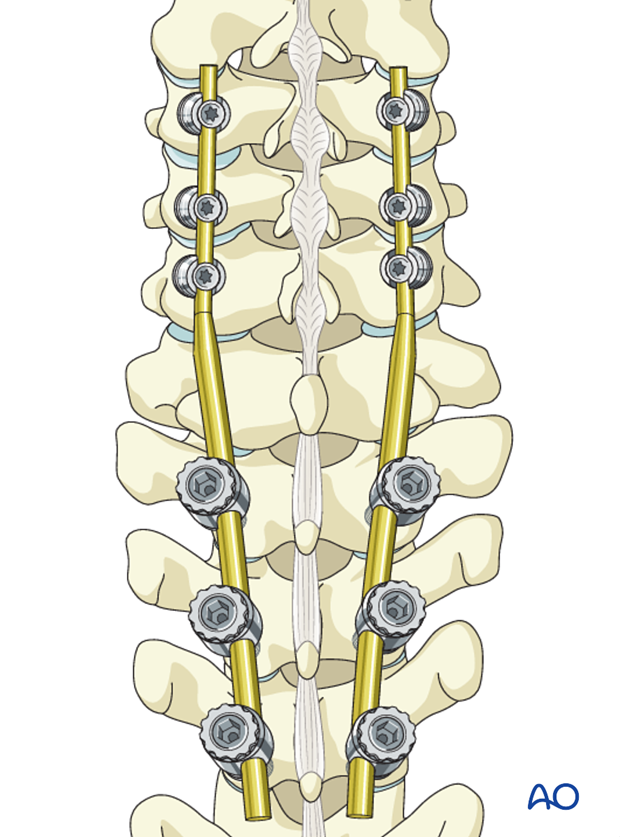
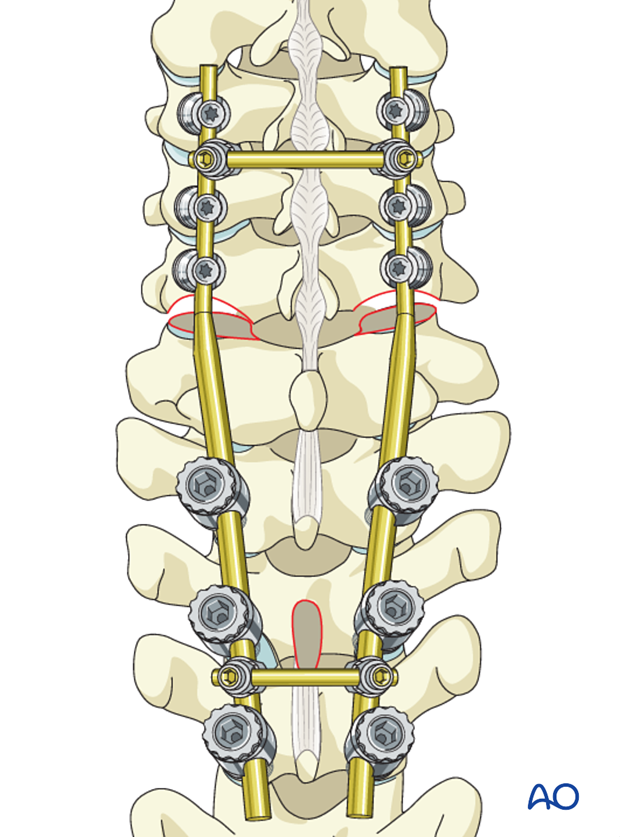
Screws are inserted at least two or three segments above and below the dislocation.
Cervical screws
In the lower cervical levels the following screws can be used:
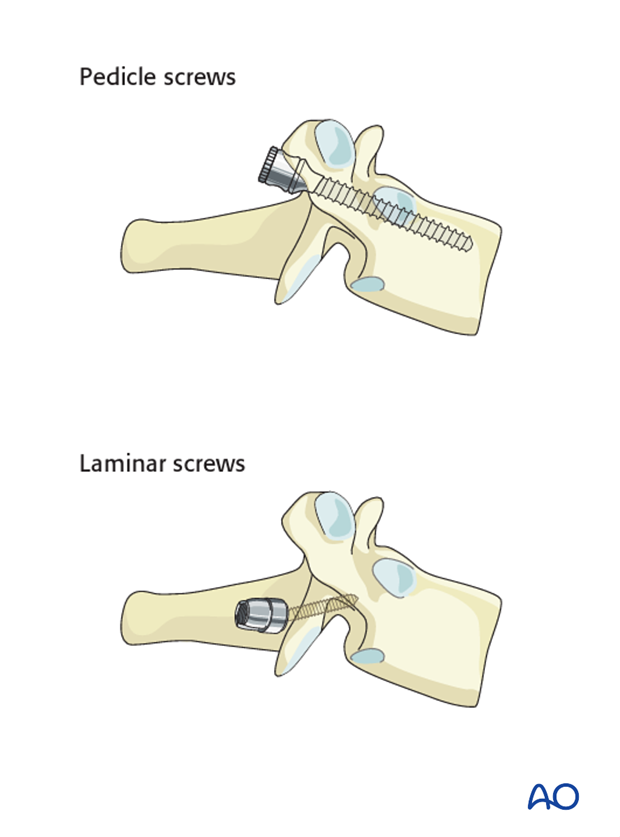
Due to safety, lateral mass screws are preferred from C6 to cranial. If the lateral mass is compromised an additional level can be included in the fixation or pedicle screws may also be considered.
A lateral mass screw can also be used at the level of the fracture if the lateral mass is intact.
Thoracic screws
In the upper thoracic spine the following screws can be used:
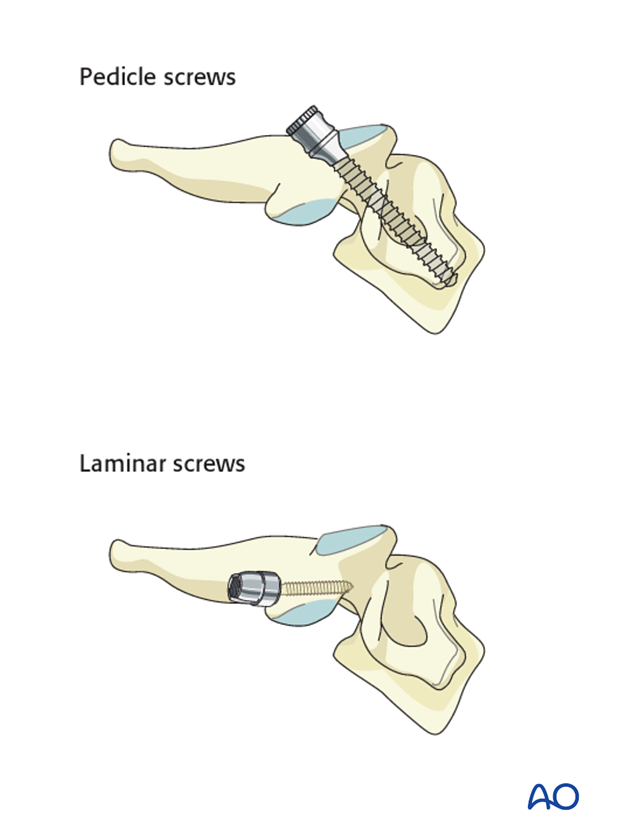
Pedicle screws are biomechanically stronger and preferred; however, if the pedicles are too small, laminar screws can be used as an alternative at the level of T1-T2.
Inserting of the screws before decompression is recommended to prevent extensive epidural bleeding.
4. Decompression
If the spinal cord needs to be decompressed or a fractured lamina needs to be removed, this should be performed after screw insertion.
5. Reduction
Rod selection
For this procedure there are two rod options:
- Double diameter tapered rod (6mm at the thoracic end, 3.5 mm at the cervical end) may be used if available. In this case no rod connectors are needed.
This is the preferred option as it easier to install and reduces operating time.
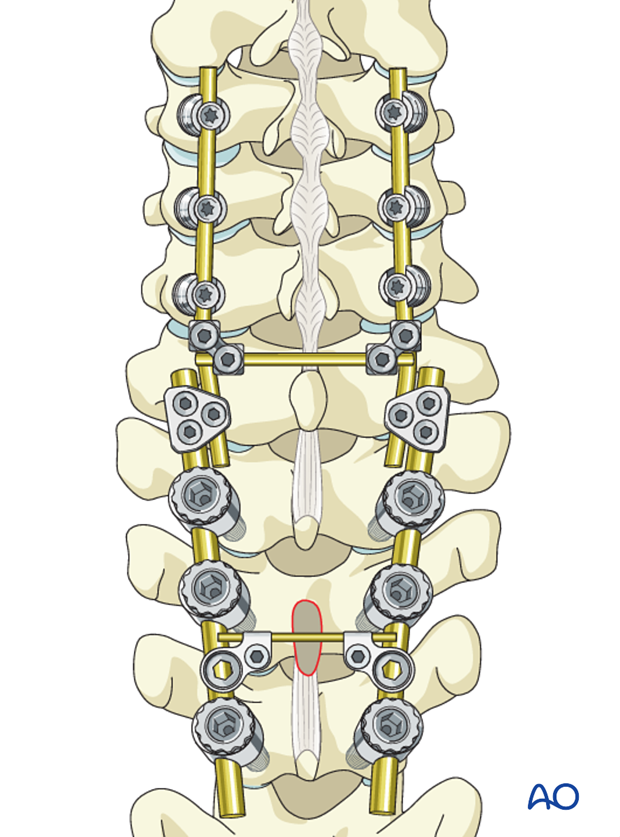
- A rod with a uniform diameter (3.4 or 4.0 mm) combined with a site to site connector between the cervical and thoracic spine. The rod connectors will have different diameters.
The rod connectors at this level are usually bulky and may cause problems with the wound closure.
Transverse connectors can be used in case of severe torsional instability, but they also may cause problems with wound closure at this level.
Rod contouring
Rods should be contoured in such a way that hyperextension can be reduced. This means that the rod should produce more kyphosis than the shape of the spine.
Ideally the correct contouring should be achieved in the first attempt. Continuous adjustments will eventually lead to material fatigue.
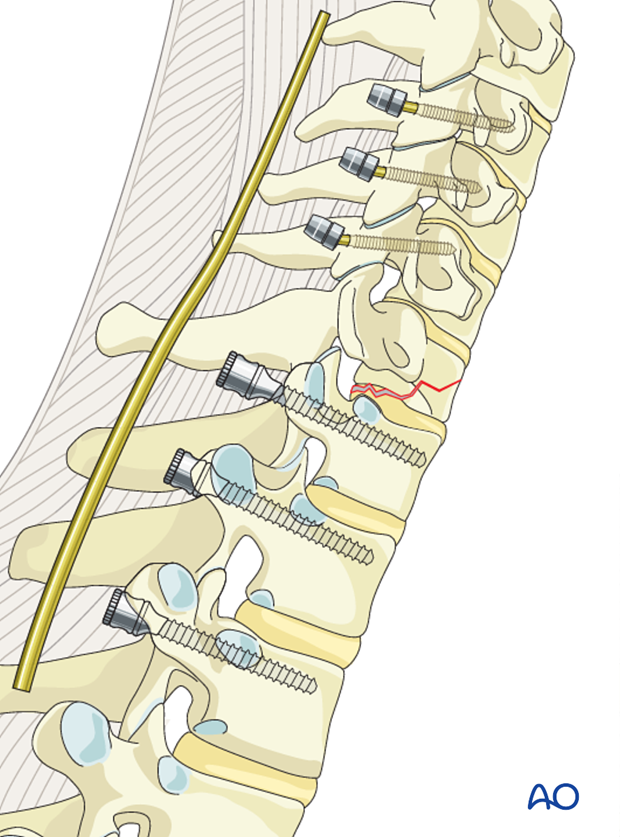
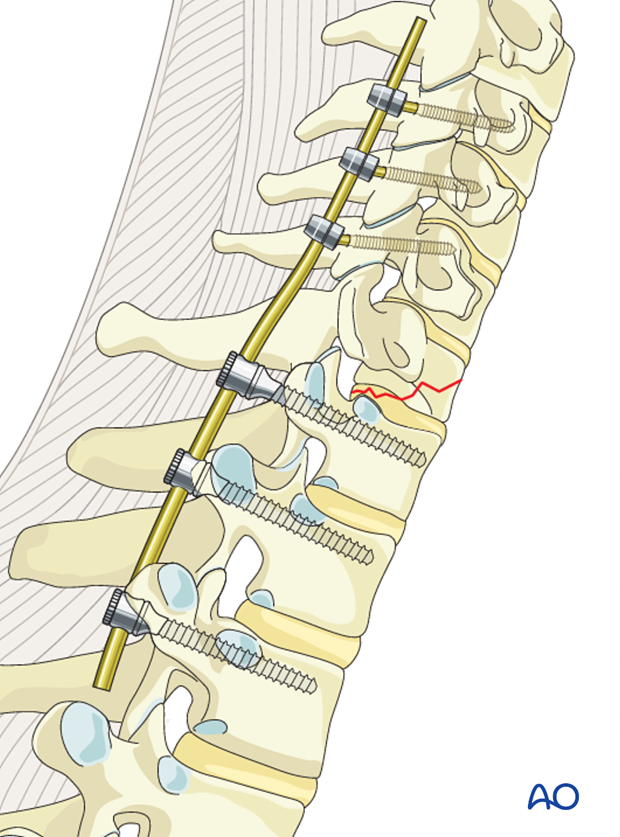
Reduction and fixation
The fracture is reduced by attachment of the rod to the screws. As the rod approaches the screw heads, the rod will exercise a gentle push on the cervical spine and reduce the fracture.
Complete reduction of the hyperextension position is not necessary.
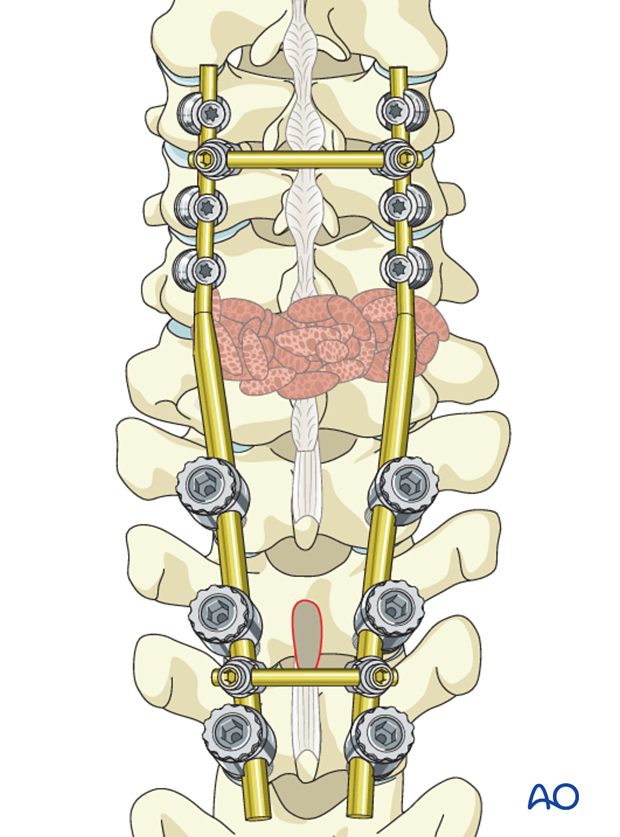
6. Fusion
Although fusion was routinely performed for all spinal fractures, its indications are now being restricted to fractures that are highly unstable.
Fusion is routinely performed for B3 injuries as they are unstable injuries with extensive soft tissue and ligamentous disruption.
If the surgeon plans for a fusion, the facet capsule is excised and the joint cartilage surfaces are denuded/curetted.
Pieces of bone graft (autograft, allograft) are inserted into the decorticated facet joint for fusion.
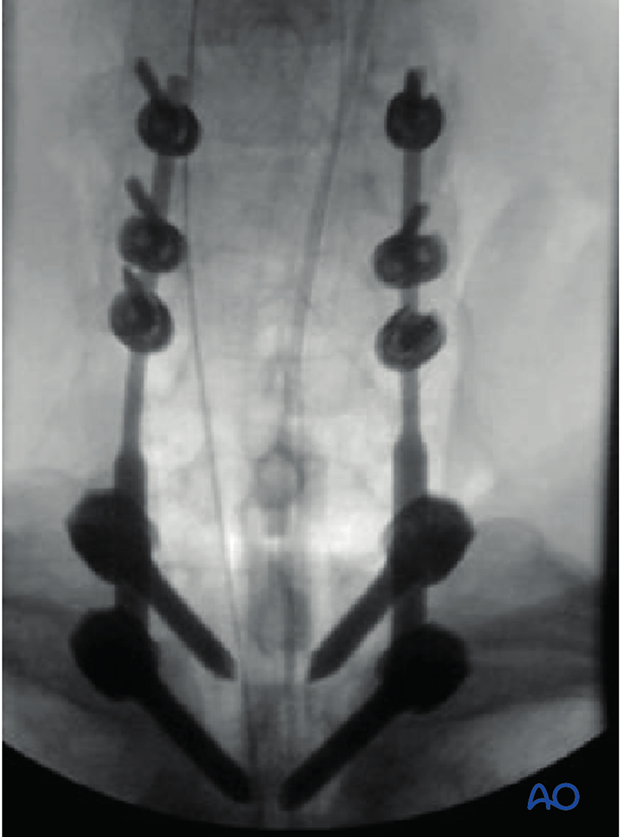
7. Postoperative imaging
Postoperative AP views should be obtained. As lateral views are not available in this area, a CT scan should be obtained as soon as possible after surgery to confirm the placement of the instrumentation and sufficient reduction.
8. Aftercare
Patients are made to sit up in bed on the first day after surgery.
A collar is commonly used following surgical stabilization to moderate patient activity.
The purpose of a collar is to prevent ranges of motion outside of limits deemed unfavorable for fracture healing. Collar is optional.
Patients with intact neurological status are made to stand and walk on the second day after surgery. Patients can be discharged when medically stable or sent to a rehabilitation center if further care is necessary. This depends on the comfort levels and presence of other associated injuries.
Patients are generally followed with periodical x-rays at 6 weeks, 3 months, 6 months, and 1 year.