Spinopelvic fixation
1. Introduction
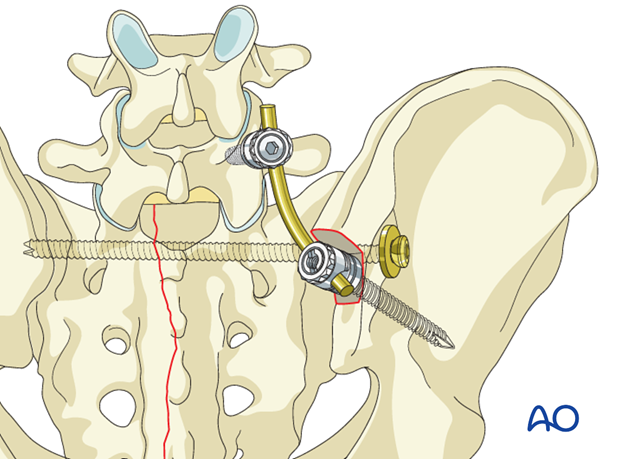
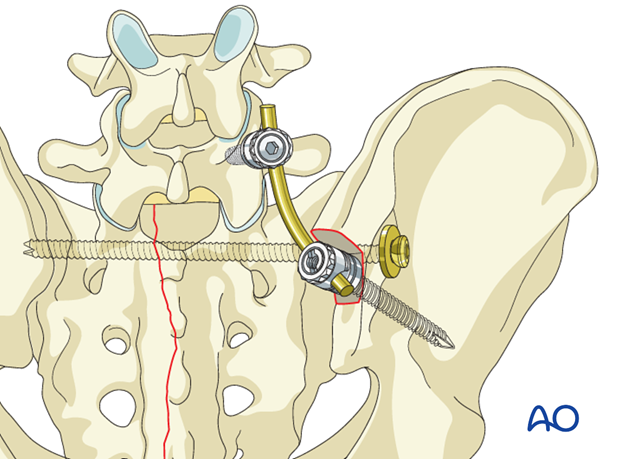
Triangular osteosynthesis is a subcategory of spinopelvic fixation. It combines
- lumbo-pelvic fixation ((usually unilateral) from the pedicle of L5 to the ipsilateral posterior ilium, and
- transverse sacral alar fracture fixation (iliosacral screw/s, sacral plate, etc.)
This technique offers mechanically better fixation for highly unstable, vertical shear sacral alar fractures. The lumbo-pelvic fixation, applied after reduction of the pelvic ring injury, helps prevent recurrent vertical displacement of the unstable hemipelvis.
As a result, early mobilization of the patient may be achieved, with avoidance of late deformity. However, prominent hardware, impaired healing, nerve root injury, and need for hardware removal are potential concerns. Improved techniques may reduce complication rates, especially reduction and fixation of the sacral fracture, with preliminary neural decompression, before applying distraction to the lumbo-sacral instrumentation.
For illustration purposes, we show here only the spinopelvic fixation which follows the IS screw insertion. Typically iliosacral screw fixation precedes spinopelvic fixation because of the tight anatomical constraints to iliosacral screw placement.
2. Positioning and approach
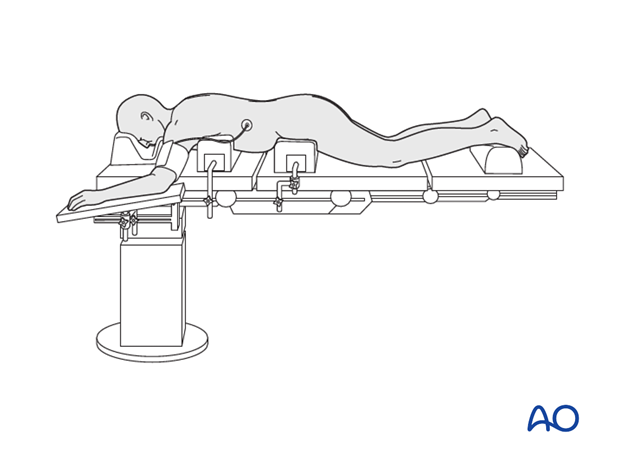
This procedure is performed with the patient placed prone through a midline or paramidline approach.
3. Reduction
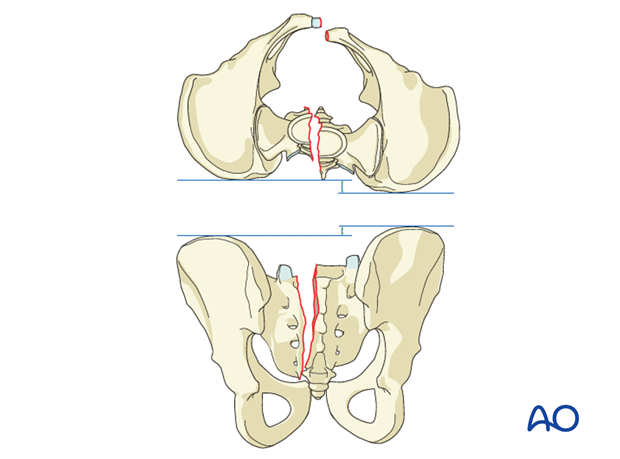
ISS fixation requires an essentially anatomically reduced sacral fracture. Significant residual displacement renders this procedure unsafe.
Displacement may make it impossible to accomplish ISS fixation without causing nerve root injury or resulting in an extraosseous screw that threatens adjacent neurovascular structures.
If displacement remains significant after closed reduction, open reduction should be considered.
The typical displacements are cranial and posterior together with sagittal plane rotation.
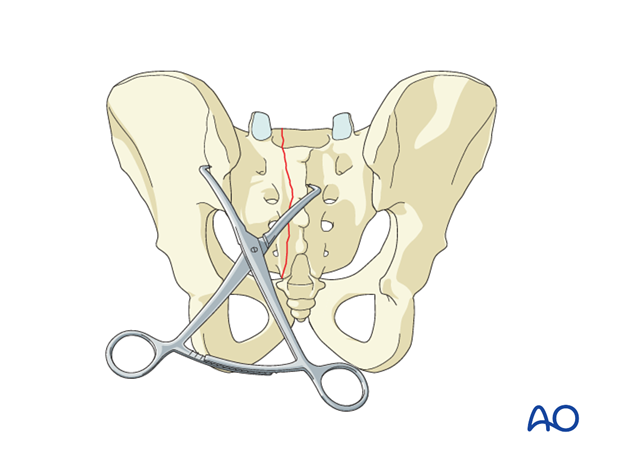
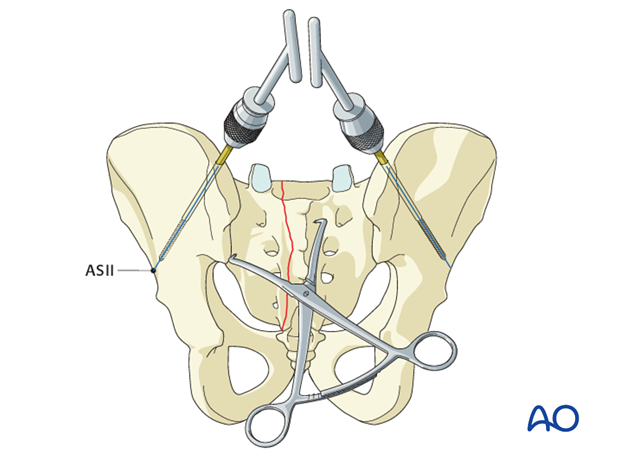
Preliminary fixation
Once the fracture edges have been debrided, the primary reduction maneuver typically involves the use of two pointed reduction forceps (Weber clamps).
These span from the spinous process to the lateral ilium and are used to incrementally obtain a step by step reduction by alternating translation and clamping.
Preliminarily fix the anatomic reduction with pointed reduction forceps.
Additional reduction techniques
If needed, insert Schanz screws into both posterior iliac crests as a reduction aid for better rotational reduction.
4. Insertion of the IS screws
Before beginning an ISS screw fixation procedure, appropriate preoperative planning for screw type and location needs to be completed.
Following reduction, the IS screw is inserted.
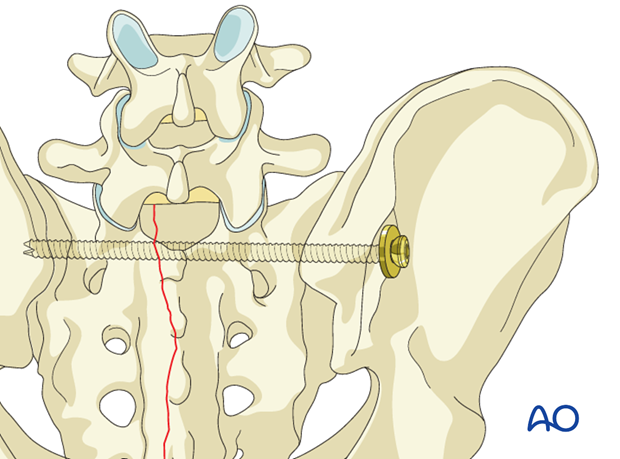
5. Insertion of the pedicle screws
Pedicle screws are inserted bilaterally in L5 and connected with the rod. If there is concern regarding fixation to L5, then more cranial fixation levels can be added.
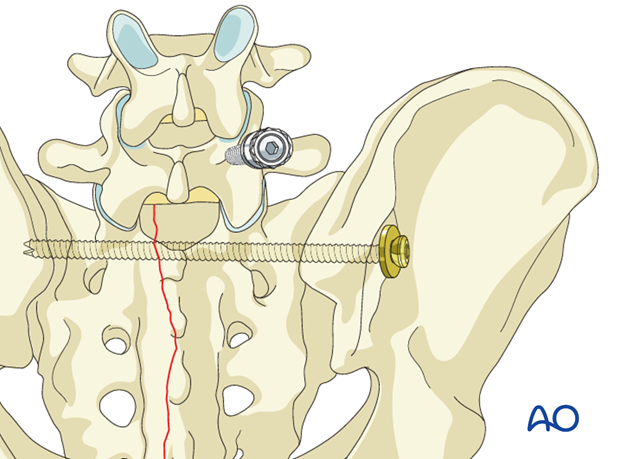
6. Insertion of iliac screw
Iliac screws are inserted in either of the three potential locations
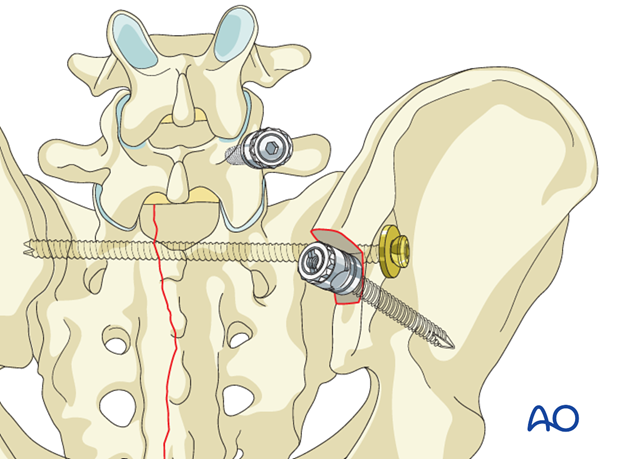
7. Insertion of the connection rod
It is important that the iliac screw head and connecting rod lie flush to the bone. Avoiding prominent hardware prevents soft tissue irritation.
With a sacral entry point for the iliac screw there is less concern with screw prominence compared to iliac starting points.
Cut the rod to the appropriate length. Attach it to the screw per the hardware system.
8. X-rays
After completion of internal fixation, confirm the final reduction and hardware position intraoperatively by AP, inlet and outlet radiographic imaging.

9. Aftercare following open reduction and fixation
Postoperative blood test
After sacral surgery, routine hemoglobin and electrolyte check out should be performed the first day after surgery and corrected if necessary.
Analgesics
Adequate analgesia is important. Non pharmacologic pain management should be considered as well (eg. local cooling and psychological support).
Anticoagulation
Prophylaxis for deep vein thrombosis (DVT) and pulmonary embolus is routine unless contraindicated. The optimal duration of DVT prophylaxis in this setting remains unproven, but in general it should be continued until the patient can actively walk (typically 4-6 weeks).
Drains
Drains, if used, are usually removed after 48 hours.
Wound dressing
Dressings should be removed and wounds checked after 48h, with wound care according to surgeon's preference.
Physiotherapy
The following guidelines regarding physiotherapy must be adapted to the individual patient and injury.
- It is important that the surgeon decide how much mechanical loading is appropriate for each patient's pelvic ring fixation. This must be communicated to physical therapy and nursing staff.
- For all patients, proper respiratory physiotherapy can help to prevent pulmonary complications and is highly recommended.
Upper extremity and bed mobility exercises should begin as soon as possible, with protection against pelvic loading as necessary. - Mobilization can usually begin the day after surgery unless significant instability is present.
Generally, the patient can start to sit the first day after surgery and begin passive and active assisted exercises. - Patients who are treated with spino pelvic fixation constructs are typically allowed to bear weight as tolerated unless precluded by other injuries.
The following applies to patients treated without spinopelvic fixation:
- For unilateral injuries, gait training with a walking frame or crutches can begin as soon as the patient is able to stand with limited weight bearing on the unstable side.
- In unstable unilateral sacral injuries, weight bearing on the injured side should be limited to "touch down" (weight of leg). Assistance with leg lifting in transfers may be necessary.
- Progressive weight bearing can begin according to anticipated healing. Significant weight bearing is usually possible by 6 weeks but use of crutches may need to be continued for three months.
- Fracture healing and sacral alignment are monitored by regular X-rays every 4-6 weeks until healing is complete.
Bilateral unstable sacral fractures and spinopelvic dissociation
Extra precautions are necessary for patients with bilateral unstable sacral fractures and spinopelvic dissociation. Physiotherapy of the torso and upper extremity should begin as soon as possible. This enables these patients to become independent in transfer from bed to chair.
Patients with bilateral unstable sacral fractures and spinopelvic dissociation who are treated with spino pelvic fixation constructs are typically allowed to bear weight as tolerated unless precluded by other injuries.
The following applies to patients treated without spinopelvic fixation:
- For the first few weeks, wheelchair ambulation may be necessary. After 3-4 weeks walking exercises in a swimming pool are started.
- After 6 weeks, if pain allows, the patient can start walking with a three point gait, with less weight bearing on the more unstable side.
Full weight bearing is possible after complete healing of the bony or ligamentous legions, typically not before 12 weeks.













