Anterior C2–C3 fusion
1. Preliminary remarks
Anterior fixation is a useful technique to achieve sufficient decompression and interbody fusion. It is the best technique for restoring cervical lordosis.
Direct decompression from disc or bone material can be performed directly without mobilization of the neurological structures.
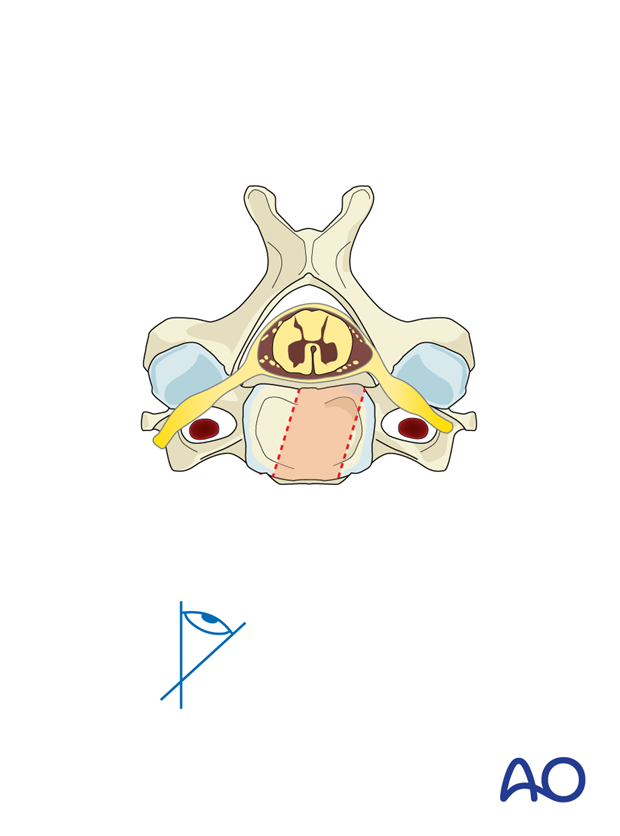
Visualization of the dura allows direct confirmation of complete decompression.
Nerve roots are better identified from a posterior approach, but experienced surgeons can also perform an anterior foraminotomy.
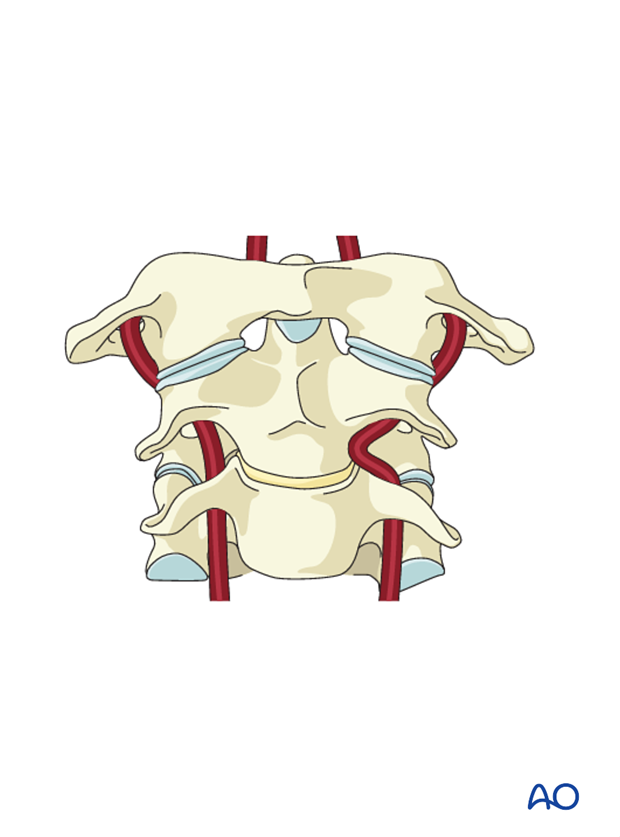
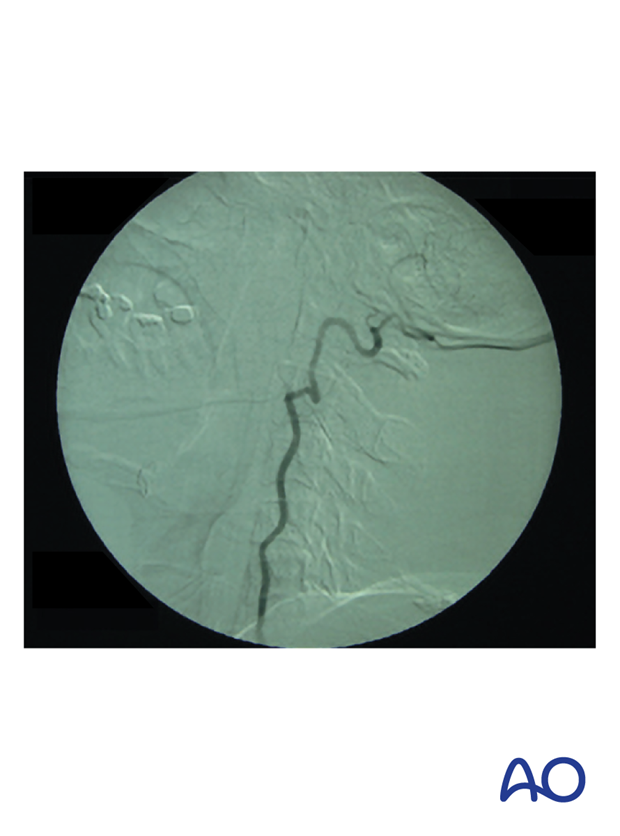
Preoperative evaluation of potential anatomic variations in the course of the vertebral artery is mandatory. Unidentified anatomical variations may increase the risk of compromising the artery during decompression.
The image is a preoperative angiography showing a suspected abnormal vertebral artery with tortuosity and medial migration of the vessel, protruding into the disc space.
Indications for anterior decompression
Indications for decompression during anterior reconstruction include the following:
- The presence of a traumatic disc herniation causing neurologic injury (discectomy alone)
- The need to remove a portion or entire vertebral body followed by reconstruction for stability or relief of symptomatic neural compression
- Kyphotic angulation with ventral compression
Visualization
The procedure should be performed with adequate light and magnification, loupes, or a microscope.

2. Reduction
A trial closed reduction is attempted under image intensification before skin incision. Extension or flexion may be applied depending on the position of the fragments. The reduction should not include traction maneuvers because they may displace the fragments.
3. Approach and positioning
This procedure is performed using an anterior approach, with the patient in the supine position.
4. Discectomy
Before performing the discectomy, the level is confirmed with intraoperative fluoroscopy.
The following landmarks are identified:
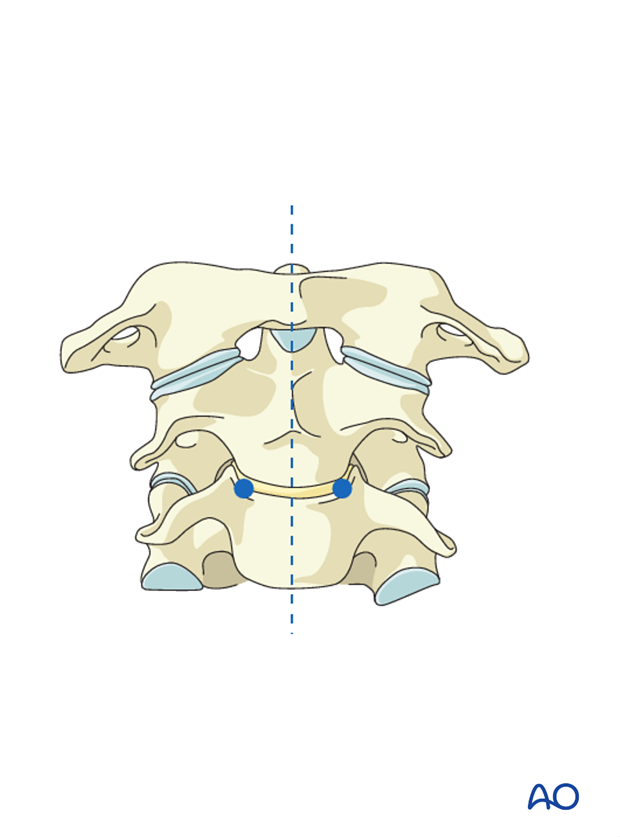
- Midline
- Unciform process
The midline will dictate the AP orientation of the discectomy.
The unciform processes dictate the lateral borders of the discectomy, establishing the safe area from the artery. This will leave a 3 mm safe zone to the normal anatomy of the vertebral artery.
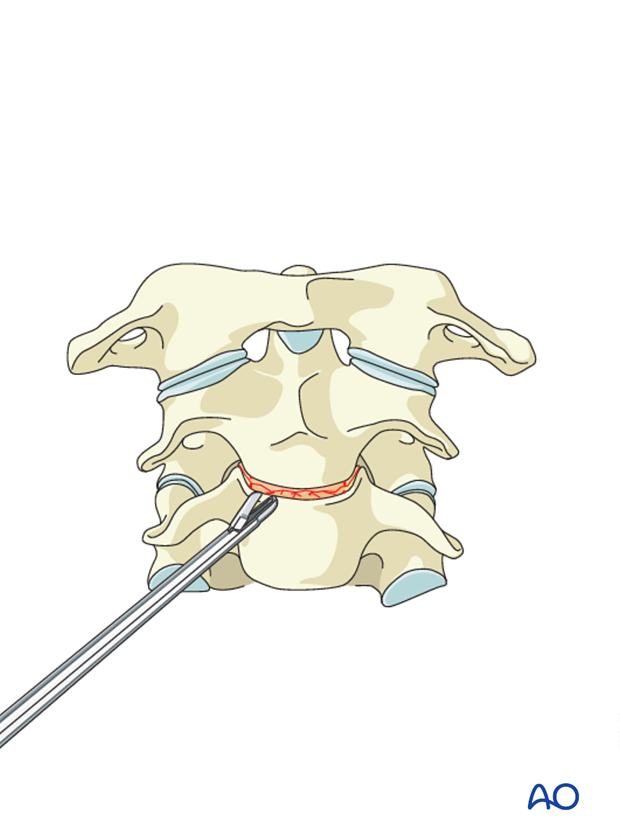
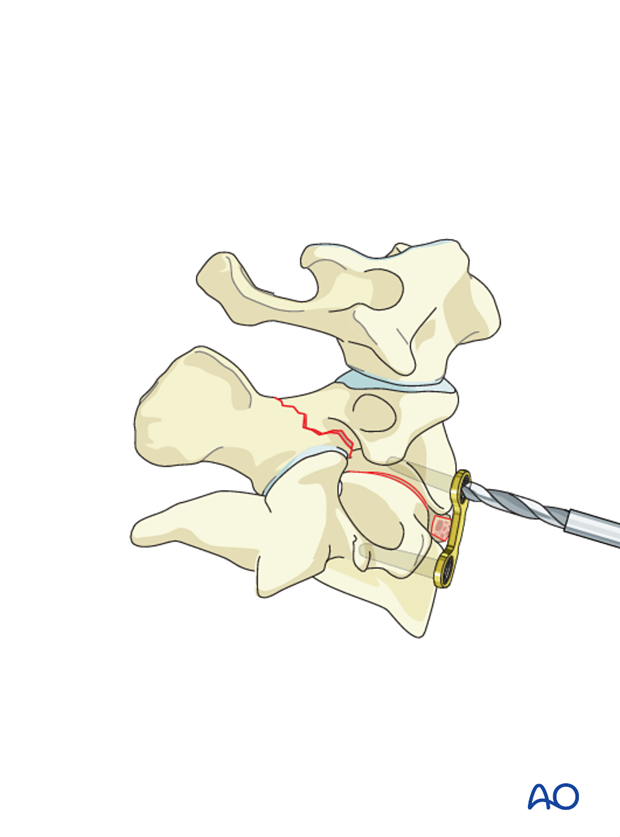
A small (No. 15) blade is used to open the annulus from uncinate to uncinate as close as possible to the endplates.

The discectomy continues using pituitary rongeurs to remove the annulus, and small curettes to scrape the endplates.
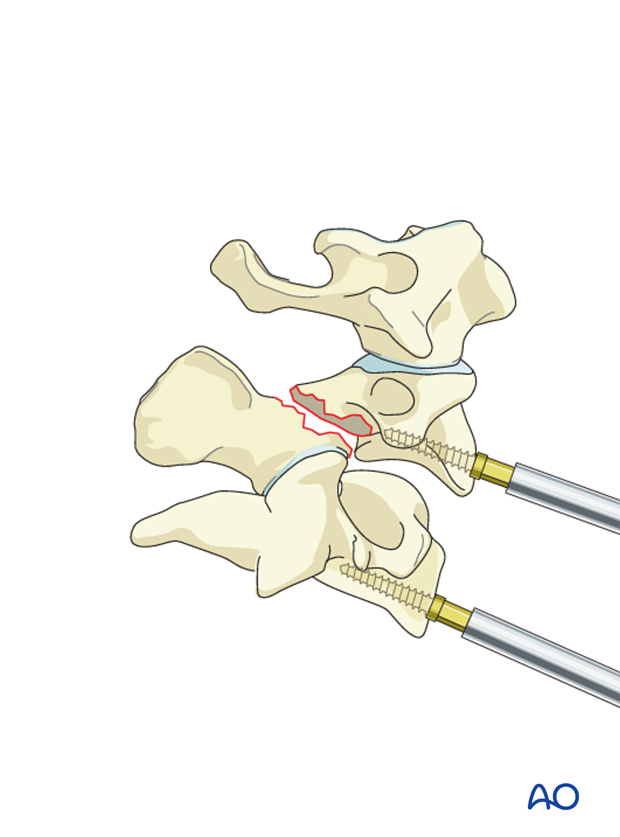
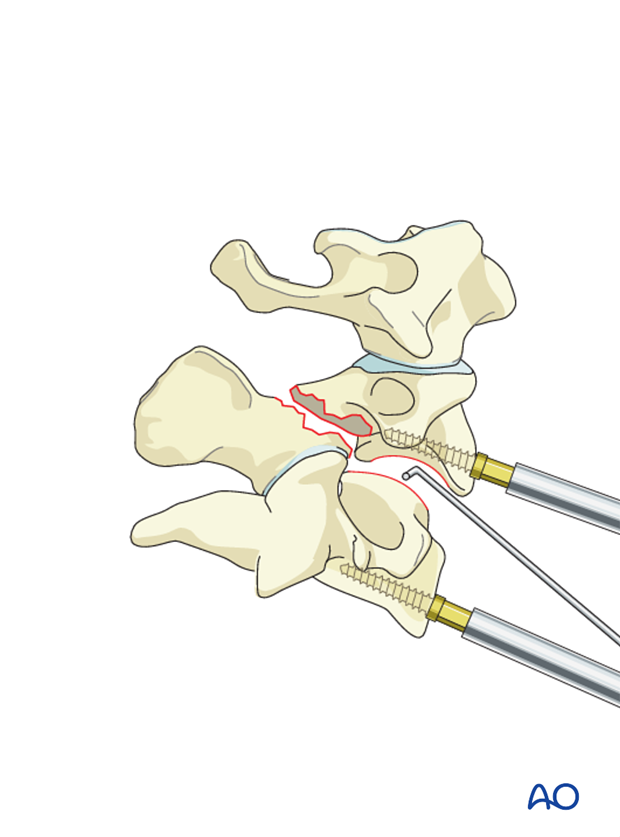
The use of a distractor or an intervertebral distractor will facilitate the removal of the posterior half of the disc and visualization of the posterior longitudinal ligament. However, it is difficult to place distractors at the C2–C3 level.
The normal height of the area should be reconstructed. However, care should be taken not to over distract.
A complete discectomy will allow good visualization of the spinal canal and enhance fusion.
Meticulously remove all cartilage from the endplates. Pieces of cartilage may inhibit fusion if present either on the endplates or in the bony material used for the fusion.
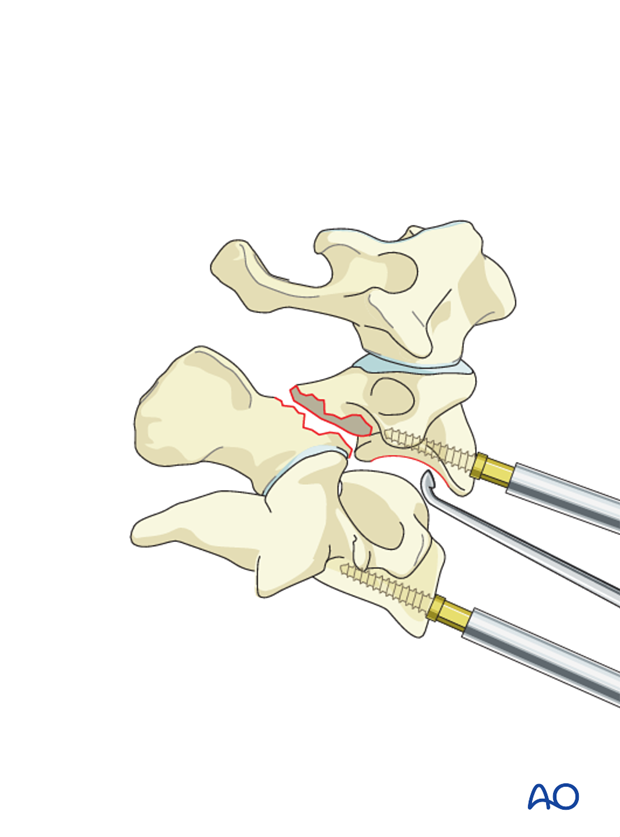
A small probe is used to ensure that no fragments are left in the area behind the vertebra, which is not directly visualized, or in the foramen.
Magnification and correct illumination are essential to make the final decompression.
5. Fusion
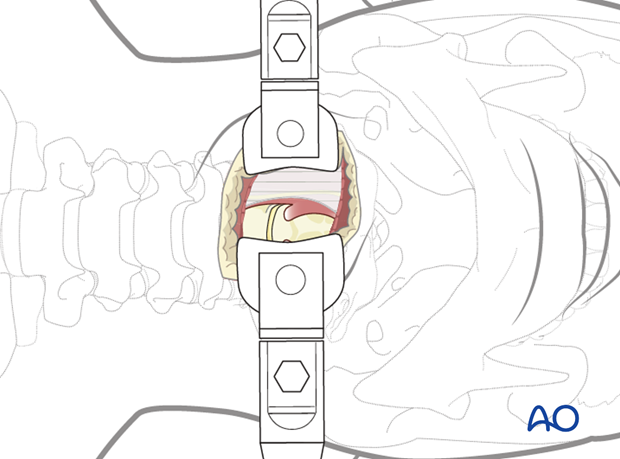
A tricortical graft is harvested from the iliac crest and inserted into the empty disc space. Great care must be taken to trim the graft so that it shares the axial load with the plate. Alternatively, a cage filled with either bone graft or bone substitute can be used.
Care should be taken not to over-distract the segment with the implant, as this may compromise postoperative stability.
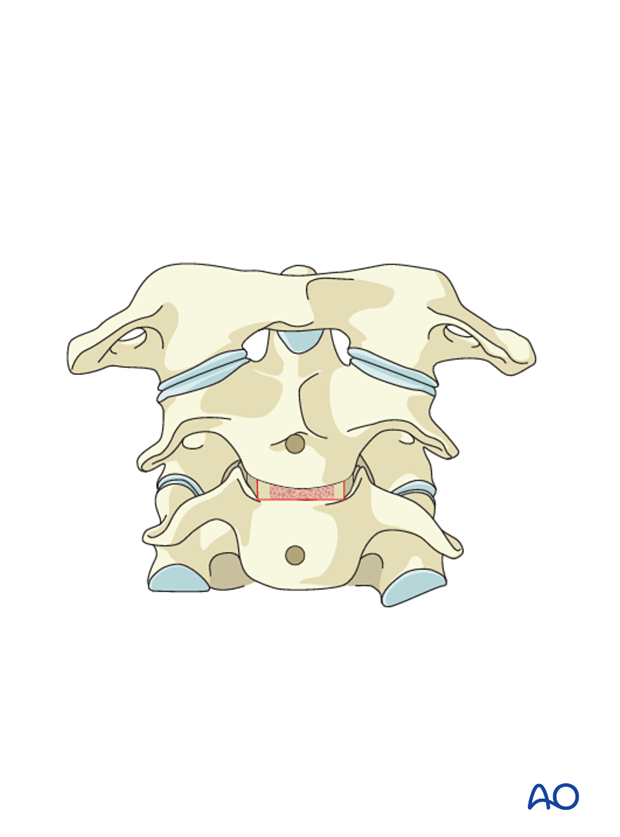
When choosing the plate length, care must be taken to prevent it from damaging the mobile discs below. The necessary plate length (blue) is confirmed under image intensification.
Ideally, the plate should extend as little as possible above and below the endplates of the injured level.

The plate is bent to accommodate the patient's lordosis and fixed in place with two temporary pins placed in holes diagonal to each other.
The appropriate positioning of the plate is verified in AP and lateral views.

Malrotation of the plate is commonly seen on the AP view and can be adjusted by temporarily removing one pin while adjusting the rotation.

Based on a preoperative measurement of vertebral body depth, screw holes of the appropriate depth are prepared. This is done under lateral fluoroscopic guidance.
Screws are inserted but not fully tightened until all screws have been applied.
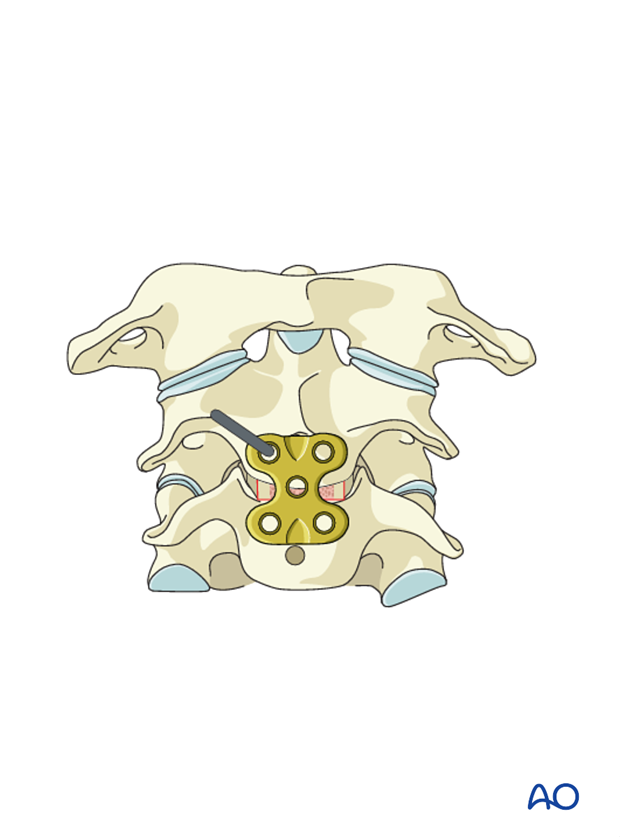
Final hardware positioning is verified in lateral and AP view.

6. Aftercare
Patients are made to sit up in bed in the evening after the operation.
A collar is commonly used following surgical stabilization to moderate patient activity.
The purpose of a collar is to prevent ranges of motion outside of limits deemed favorable for fracture healing. The collar is optional.
Patients with intact neurological status are made to stand and walk on the first day after surgery. Patients can be discharged when medically stable or sent to a rehabilitation center if further care is necessary. This depends on the comfort levels and presence of other associated injuries.
Patients are generally followed with periodical x-rays at 6 weeks, 3 months, 6 months, and 1 year.













