Transforaminal endoscopic lumbar discectomy (TELD)
1. Introduction
This procedure approaches disc pathology from a different trajectory than microscopic tubular and endoscopic interlaminar discectomy procedures.
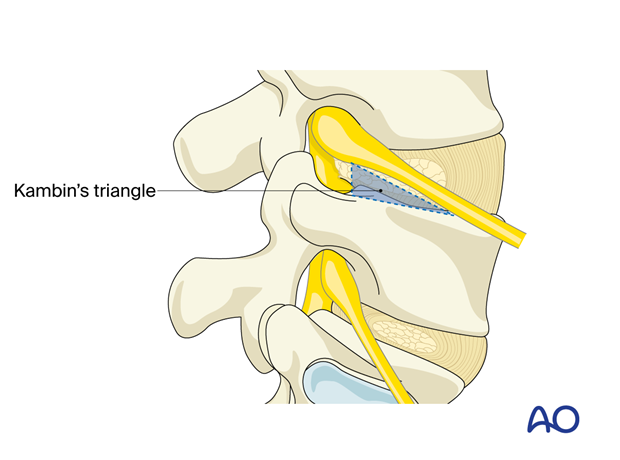
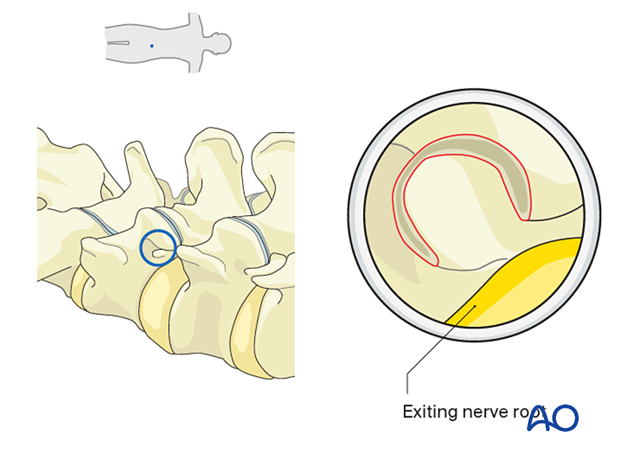
The goal is to enter the disc space through Kambin’s triangle, a safe corridor under the exiting nerve root.
This approach can be used to address posterolateral disc herniations and foraminal pathologies that do not require extensive facetectomy or fusion.
2. Required instruments
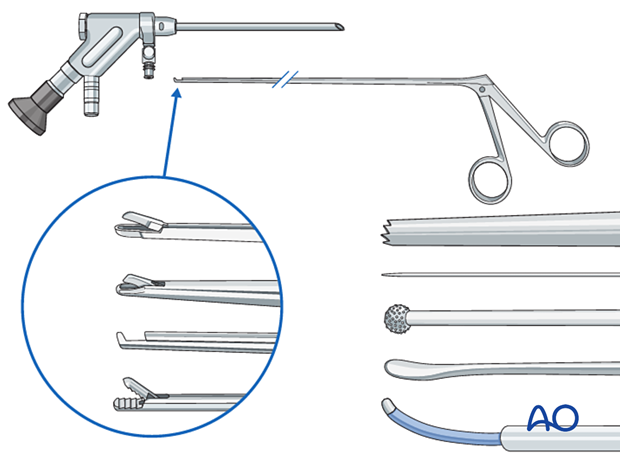
- Endoscopy cart (video, pump (50 mmHg), radiofrequency unit, drill)
- Transforaminal endoscope
- Reamers
- K-wire
- 18 gauge spinal needle
- Blunt dissector
- Micro-punch
- Grasping forceps
- Kerrison rongeur
- Bipolar coagulator
- Burr
- C-arm
3. OR set up and patient positioning
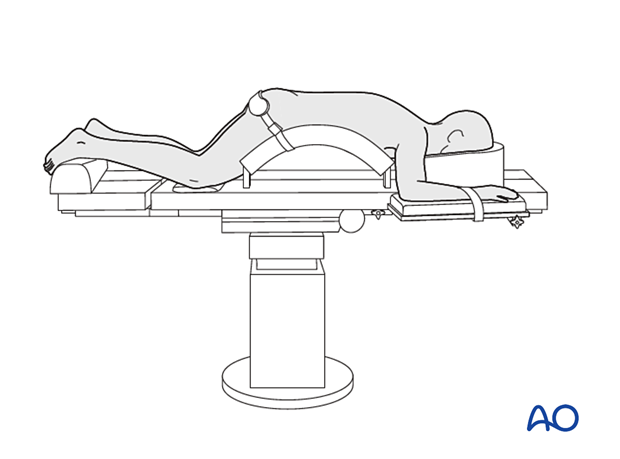
The patient is placed prone on a Wilson frame or with pelvic and thoracic rolls.
4. Fluoroscopic identification of target level after draping
Preoperative trajectory planning
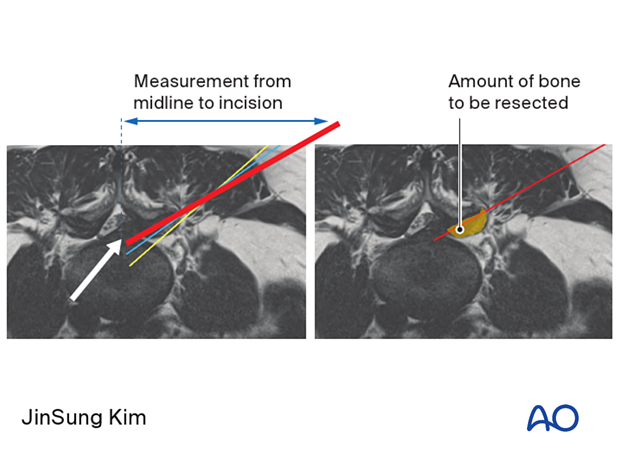
The axial MRI should be carefully evaluated. A line from the site of disc pathology through the superior articular process (SAP) to the skin should be drawn. Ideally, the line should be as ventral on the SAP as possible.
This will indicate how far off the midline the incision will be made and how much of the SAP needs to be resected.
Intraoperative trajectory planning
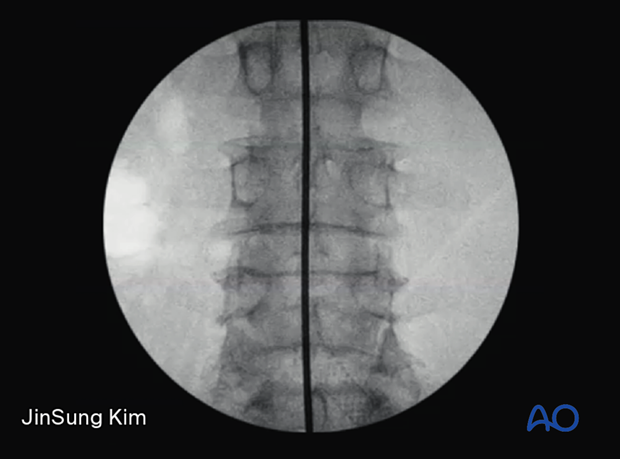
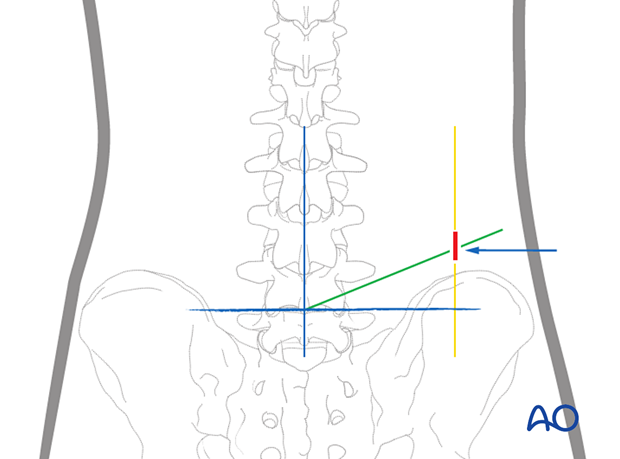
An AP x-ray is positioned to identify the midline (spinous processes are equidistant to the pedicles) and adjusted to view a square endplate of the caudal level.
Draw a horizontal line passing through the disc space on the index level on an AP X-ray.
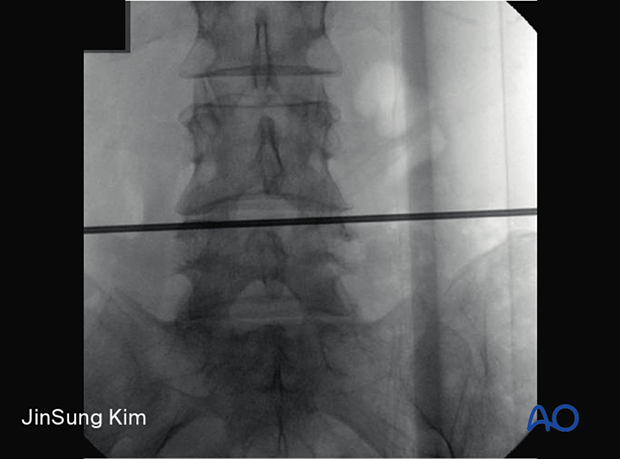
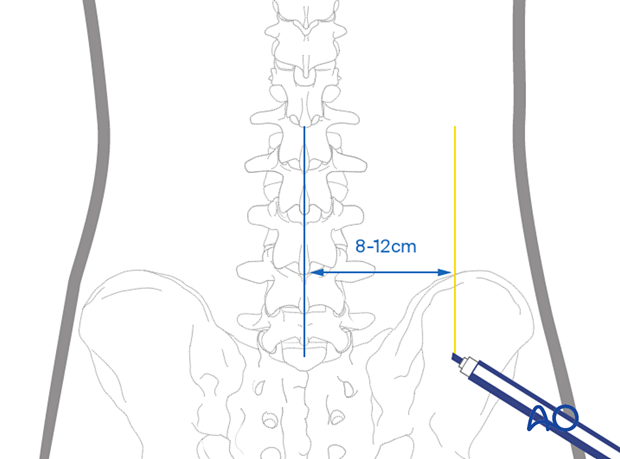
Vertical planning lines are drawn lateral to the midline. The distance from the midline is approximated based on the level.
- L3–L5 ca 8 cm
- L4–L5 ca 10 cm
- L5–S1 ca 12 cm
These approximate values depend on body habitus.
An alternative is to use the measurement obtained from preoperative imaging.
The cranial-caudal trajectory is planned by placing a radio-opaque object with the tip at the intersection of the midline and horizontal markings.
This trajectory is usually 10°–15° and should connect the upper aspect of the superior articular process with the medial pedicular line at the disc space level.
The incision is made where this line intersects the lateral vertical planning line (marked in yellow) at the predetermined distance from the midline.
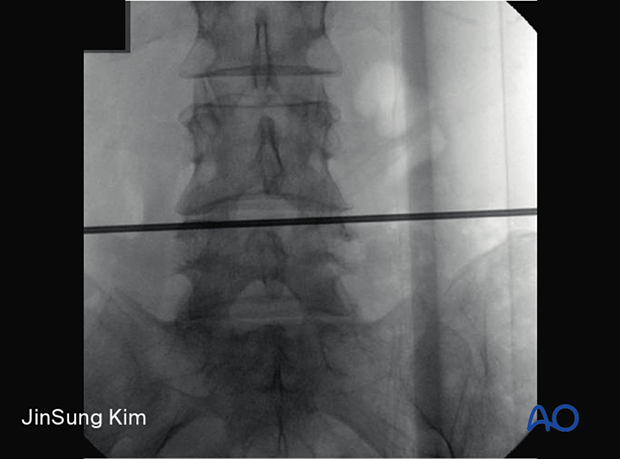
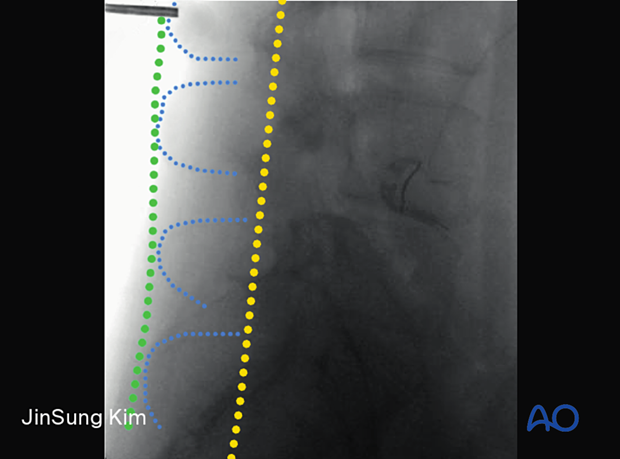
Place the radiological marker at the planned entry point and record a lateral X-ray.
When the correct entry point is chosen, the tip of the marker will typically lie between the posterior spinous line (green) and the posterior facet line (yellow). The planned entry point based on AP X-rays should not be more ventral than the posterior facet line, which may lead to a higher risk of entering the retroperitoneum.
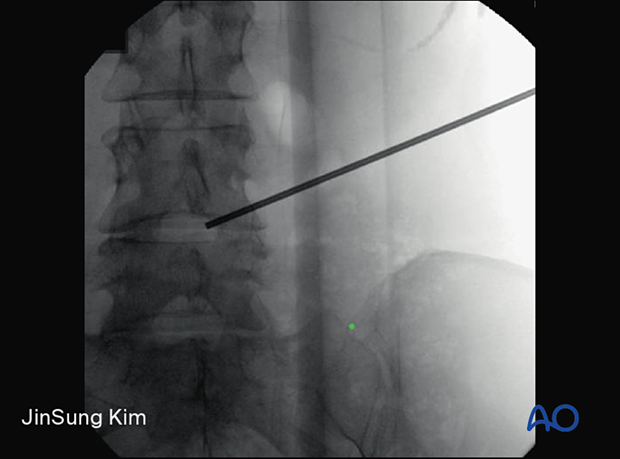
Insert the spinal needle at the predetermined entry site and follow the trajectory toward the SAP at the caudal level.
Ensure that the bevel is facing cranially towards the exiting nerve root.
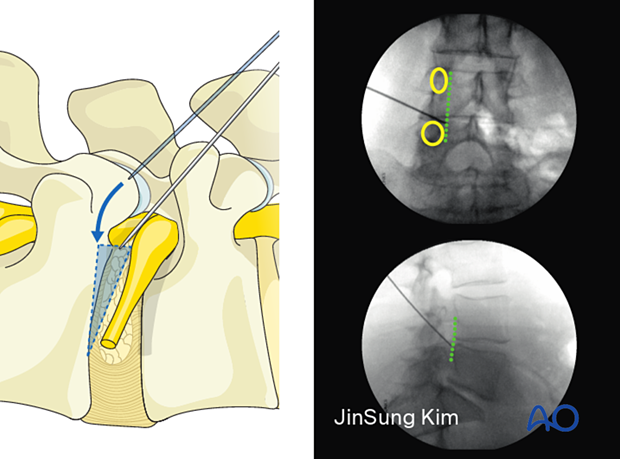
Advance the needle until the SAP is encountered and “walk the needle” ventrally until it “falls” into Kambin’s triangle.
The needle should not advance past the posterior vertebral line in the lateral X-ray or past the medial pedicle line in the AP X-ray.
Once the needle is in position (as confirmed in both lateral and AP views), insert the K-wire and advance it into the disc. Then remove the needle.
Dilation and reaming
Use serial dilators to expand the working corridor.
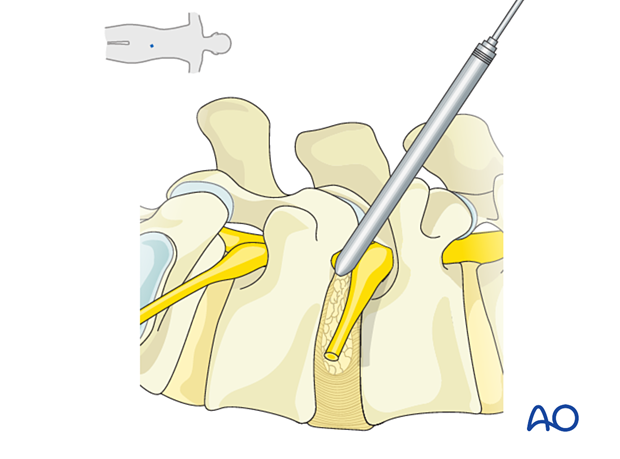
Reamers of increasing size are used to perform a foraminoplasty by resecting portions of the SAP.
This creates a wider working corridor in the bottom half of the foramen and lessens the risk of injury to the exiting nerve root, which usually resides in the top half of the foramen under the cranial pedicle.
None of the instruments should pass the medial pedicle line on AP X-rays.
The beveled working channel is inserted with the bevel facing cranially. A final AP and lateral X-ray is recorded to verify optimal positioning.
With the transforaminal approach, there can be irritation of the dorsal root ganglion, which can cause dysesthesias. If the awake patient complains of this during surgery, an alternative trajectory should be attempted to prevent further pressure on the DRG. In asleep patients, firing on the EMG may also indicate pressure on the nerve root, and a different trajectory should be considered.
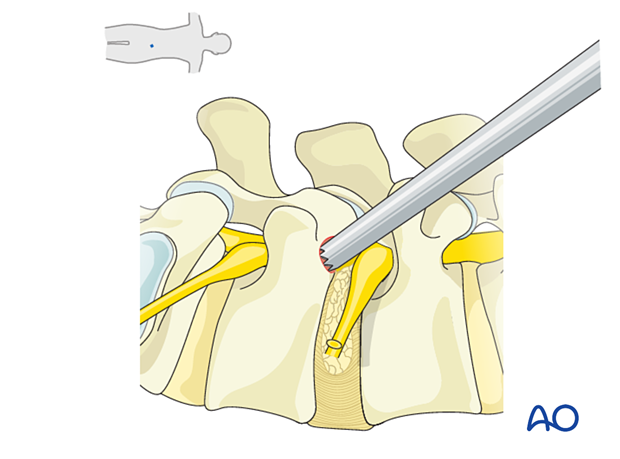
Remove the dilators and K-wire and insert the endoscope.
5. Visualization of the surgical field
The target areas to visualize are the SAP and the cranial aspect of the caudal pedicle.
If required, further SAP resection can be carried out with a diamond burr to gain access to the lateral recess.
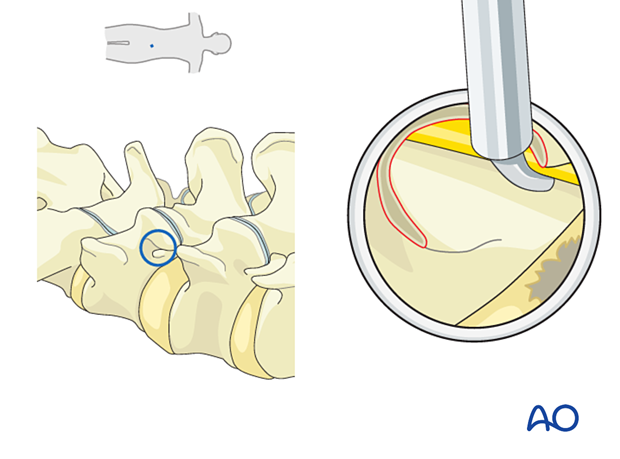
Foraminal disc herniation
Use a dissector and bipolar coagulator to clear away soft tissue and dissect into the epidural space.
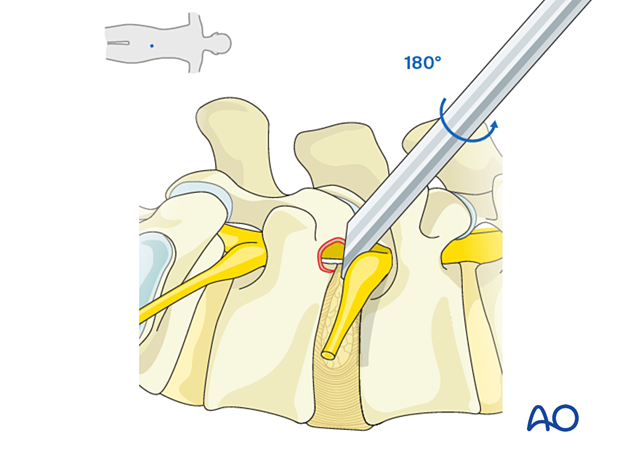
The exiting nerve root may be identified at the cranial aspect. The working channel bevel can be rotated 180° to protect the exiting nerve root for true foraminal disc herniations.
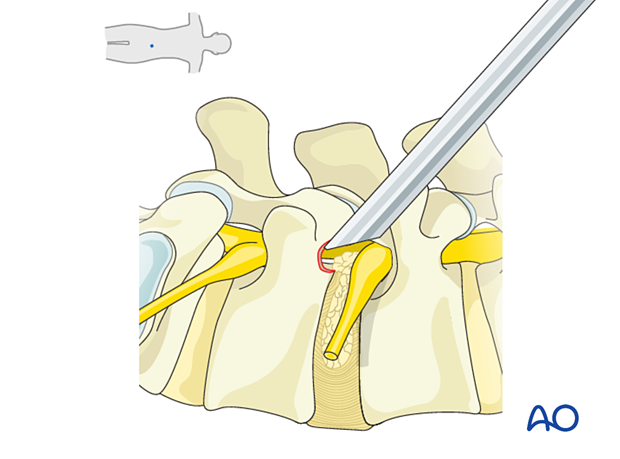
Central and posterolateral disc herniations
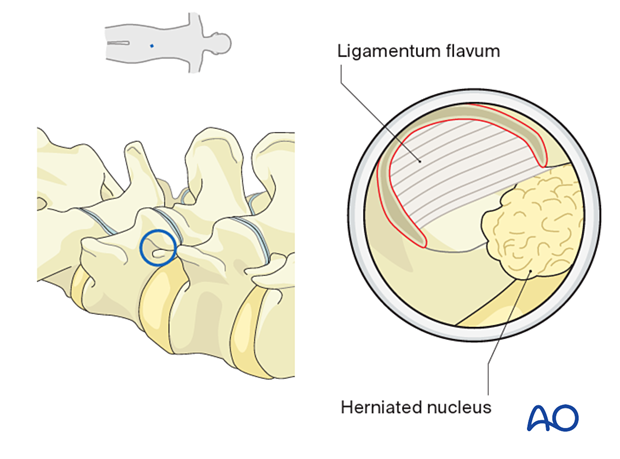
For central and posterolateral disc herniations, A Kerrison rongeur can be used to resect the lateral aspect of the ligamentum flavum and identify the transversing nerve root.
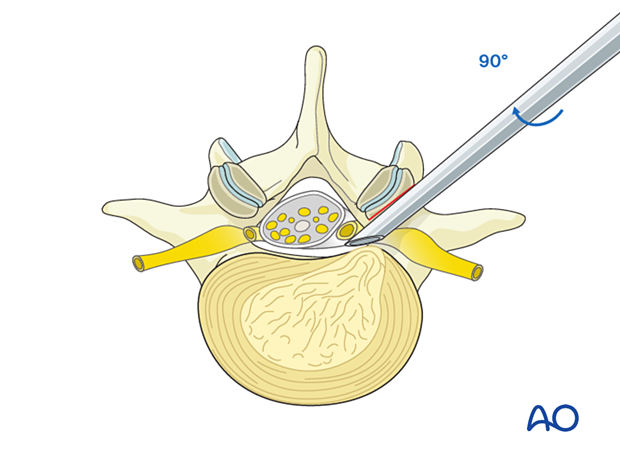
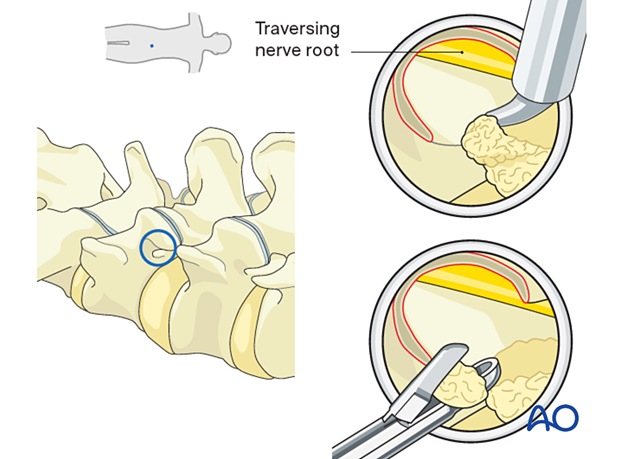
The bevel can be rotated 90 degrees clockwise (from the original position) and advanced medially and ventrally - securing the traversing nerve root dorsally and allowing direct access to the lateral recess.
6. Removal of disc fragments/decompression
A dissector or bipolar coagulator probe can be used to mobilize any disc fragments in the lateral recess, which are then removed with pituitary rongeurs.
Mobilization of neural elements
Rotation of the bevel back to its original position can allow inspection of the traversing and exiting nerve roots. Use a blunt dissector or a curved ball tip probe to verify that neural elements are easily mobilized.
7. Endoscope removal and closure
Hemostasis is achieved with hemostatic agents or bipolar cautery.
The endoscope is removed, and a deep dermal stitch can be placed at the surgeon’s discretion. A subcuticular stitch is used to close the skin.
8. Aftercare
The patient can usually be discharged on the day of surgery or the following day with a short course of pain medication.
Lumbar immobilization is not required.
Patients may feel incisional or muscular pain that usually subsides within a few days.
Patients can develop postoperative pain and muscle spasms in a delayed fashion.
There can be irritation of the dorsal root ganglion, which can cause dysesthesias. These typically get better with time.













