Extraforaminal endoscopic lumbar discectomy (EELD)
1. Introduction
This procedure approaches disc pathology from a different trajectory than microscopic tubular and endoscopic interlaminar discectomy procedures.
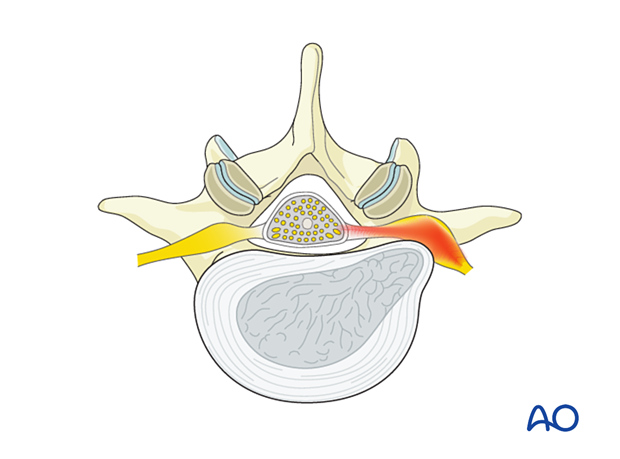
The goal of the procedure is to identify bony landmarks on the lateral aspect of the superior articular process (SAP) and pars to decompress the exiting nerve root in the extraforaminal zone.
This procedure can sometimes be more challenging than other discectomy approaches due to the lack of landmarks.
2. Required instruments
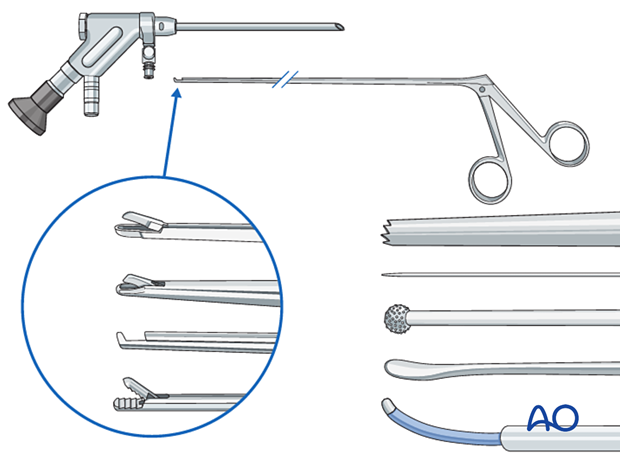
The following specialized instruments are recommended for this procedure:
- Endoscopy cart (video, pump (50 mmHg), radiofrequency unit, drill)
- Transforaminal endoscope
- Reamers
- K-wire
- 18 gauge spinal needle
- Blunt dissector
- Micro-punch
- Grasping forceps
- Kerrison rongeur
- Bipolar coagulator
- Burr
- C-arm
3. OR set up and patient positioning
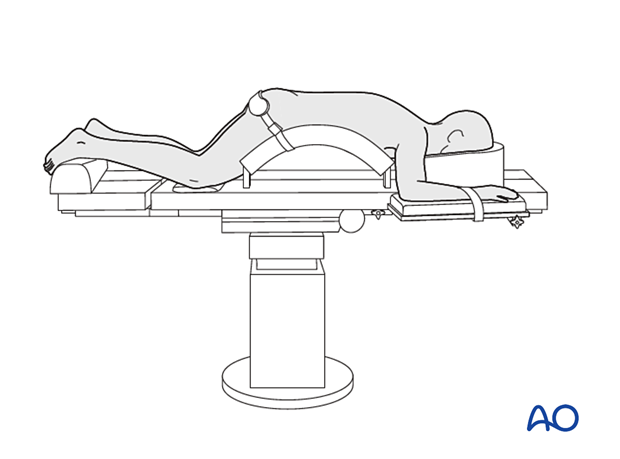
The patient is placed prone on a Wilson frame or with pelvic and thoracic rolls.
4. Fluoroscopic identification of insertion point and trajectory
AP view
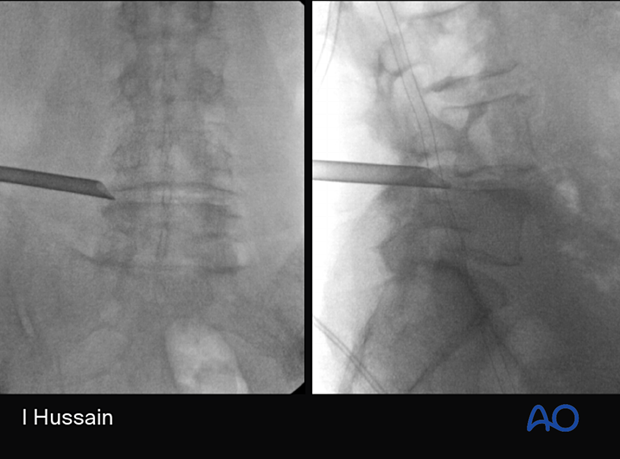
The C-arm is positioned to record the AP view of the patient's midline (spinous processes are equidistant to the pedicles) and adjusted to view a square endplate of the caudal level.
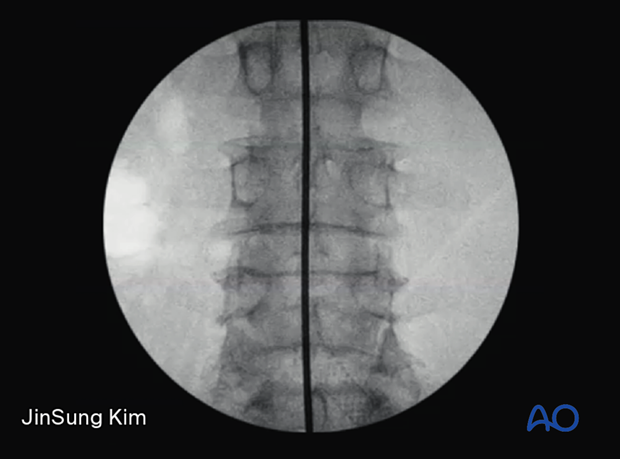
A horizontal line through the disc space is drawn.
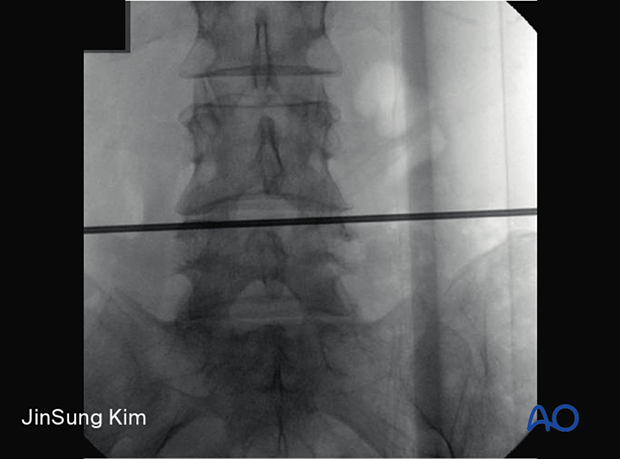
Place a radio-opaque object with the tip at the intersection of the horizontal marking and the superolateral aspect of the caudal index level pedicle.
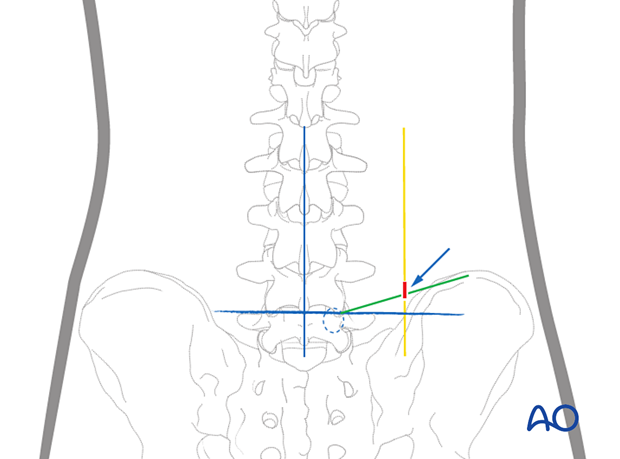
The wire is placed with a cranial-caudal angulation that is slightly less steep than used in the traditional transforaminal approach, at about 5°–10° relative to the horizontal line.
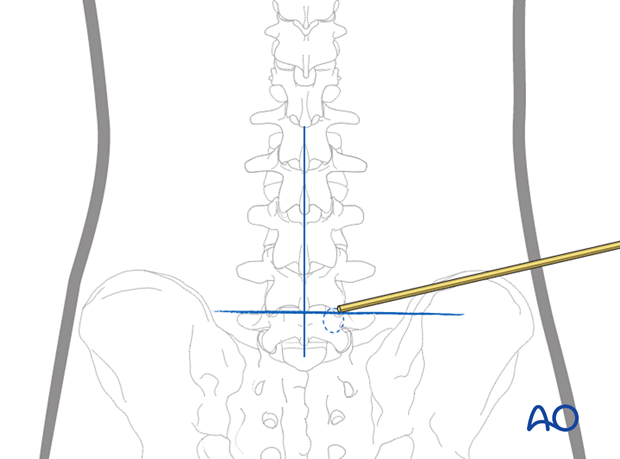
This is usually about 6–8 cm from the tip of the spinal process (the green line).
The entry point is located where the lateral vertical line (in yellow, usually about 6–8 cm from the midline) intersects a cranial-caudal angled line (green) from the pars/pedicle).
5. Insertion of working channel and endoscope
Insertion of the spinal needle
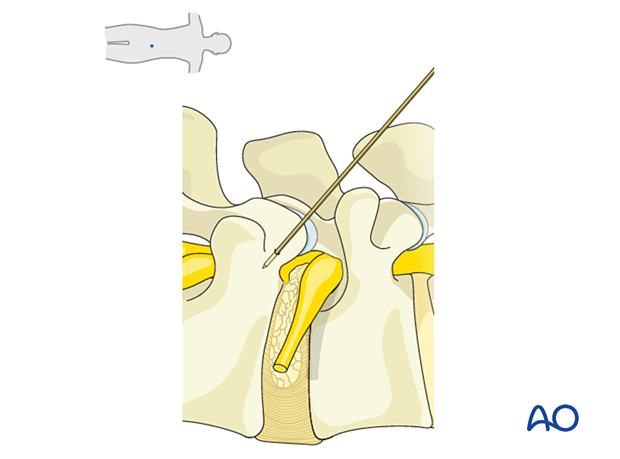
The spinal needle is inserted and angled towards the superolateral aspect of the caudal index level pedicle.
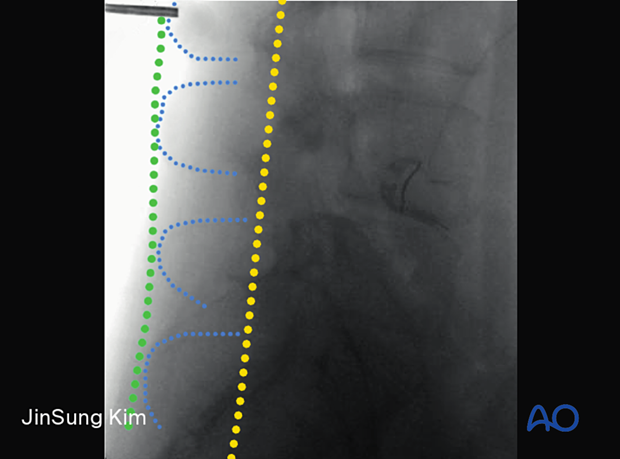
Verify the insertion vector frequently using lateral view x-rays.
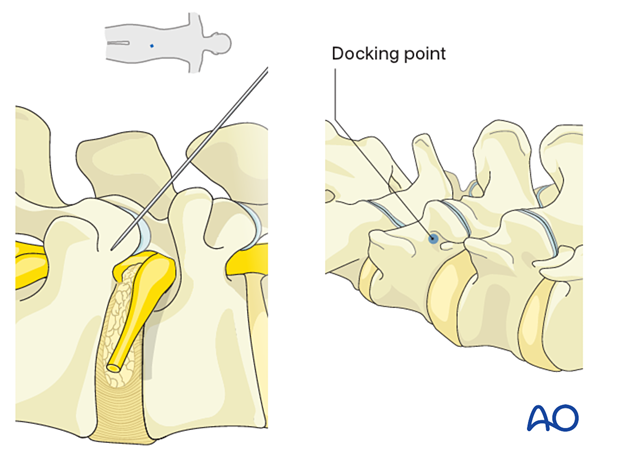
Once bone is encountered, final lateral and AP x-rays are made to confirm correct docking on the superolateral aspect of the pedicle.
Use a mallet to seat the needle firmly in the bone.
Insert the K-wire into the bone to ensure anchoring.
Insert dilators over the K-wire to expand the soft tissue corridor. Insert the working channel with the bevel facing cranially to avoid injury to the exiting nerve root.
Insert the endoscope.
Visualize the superior articular process (SAP) and the cranial aspect of the caudal pedicle.
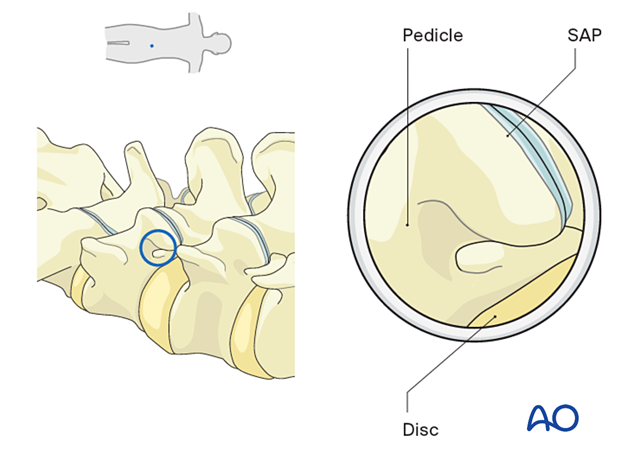
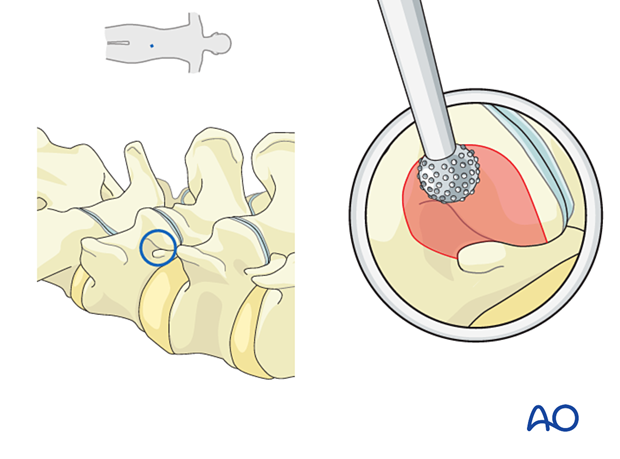
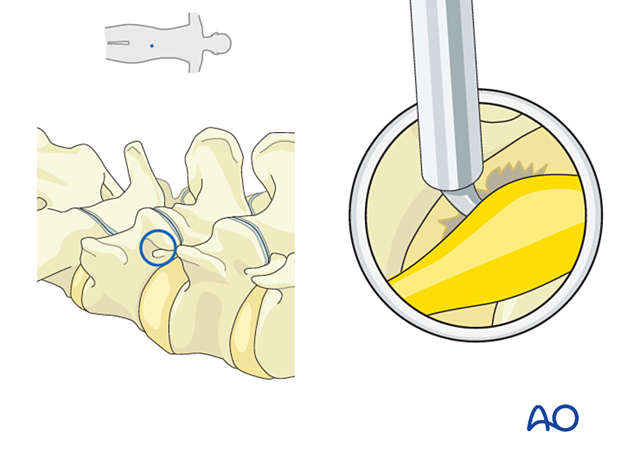
6. Superior articular process resection
Depending on visualization at this point, reamers or a diamond burr may be used to resect a portion of the SAP.
This creates a wider working corridor in the bottom half of the foramen. Doing this lessens the risk of injury to the exiting nerve root. The nerve root usually resides in the top half of the foramen under the cranial pedicle and may be displaced inferiorly by the far lateral disc herniation.
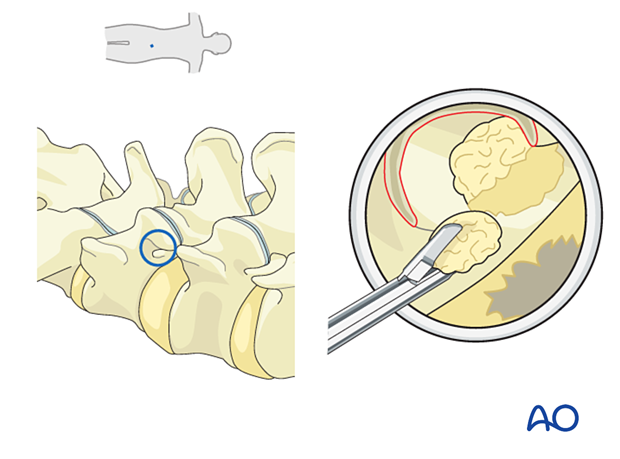
7. Decompression
Usually, with extraforaminal disc herniation, following the superior aspect of the pedicle and the posterosuperior aspect of the caudal level endplate will lead to the disc fragment. Once identified, it can be resected using pituitary rongeurs.
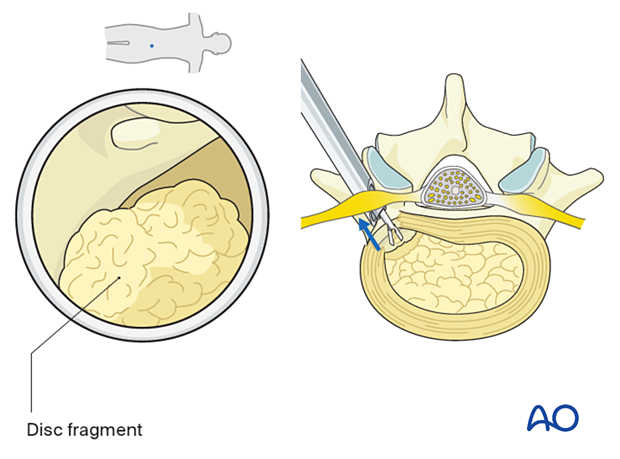
Typically, as disc fragments are removed, the exiting nerve root (mostly surrounded by perineural fat) descends from the cranial aspect into the surgical field.
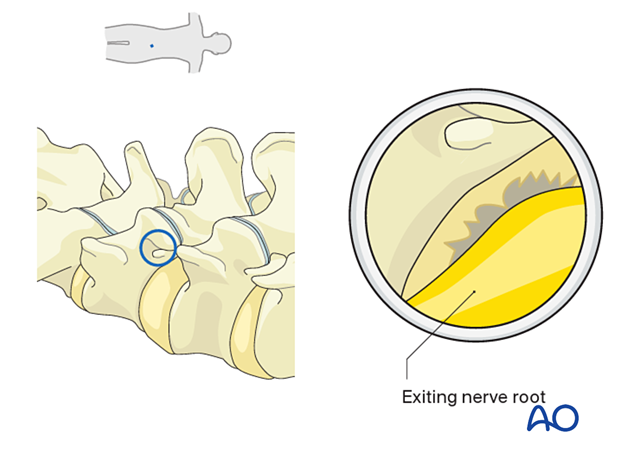
Once the exiting nerve root is identified, rotate the working channel 180° to lateralize the exiting nerve root.
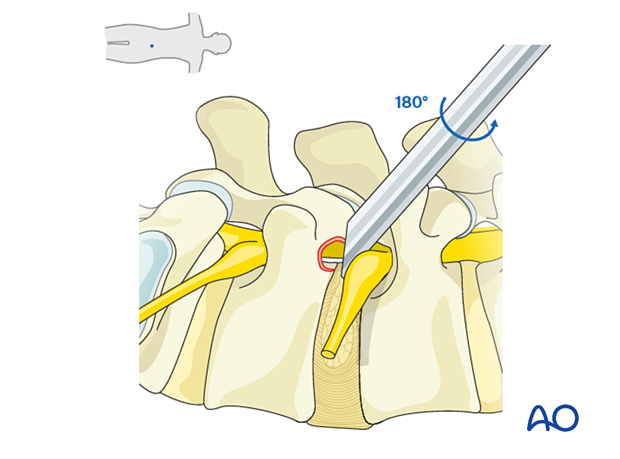
Any additional disc fragments can then be safely removed using pituitary rongeurs.
The annular defect can be explored for any contained disc fragments.
Rotate the working channel back to the original position (bevel facing cranially) to visualize the neural elements.
Use a blunt dissector or a bipolar coagulator probe to verify that neural elements are easily mobilized.
8. Endoscope removal and closure
Hemostasis is achieved with hemostatic agents or bipolar cautery.
The endoscope is removed, and a deep dermal stitch can be placed at the surgeon's discretion. A subcuticular stitch is used to close the skin.
9. Aftercare
The patient can usually be discharged on the day of surgery or the following day with a short course of pain medication.
Lumbar immobilization is not required.
Patients may feel incisional or muscular pain that usually subsides within a few days.
Patients can develop postoperative pain and muscle spasms in a delayed fashion.
There can be irritation of the dorsal root ganglion, which can cause dysesthesias. These typically get better with time.













