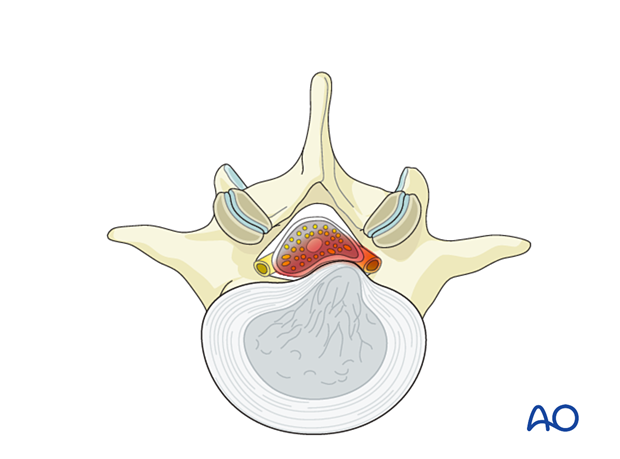
Interlaminar endoscopic lumbar discectomy (IELD)
1. Introduction
This procedure is analogous to the microscopic tubular procedure, though working through a smaller working channel (7 mm tube).
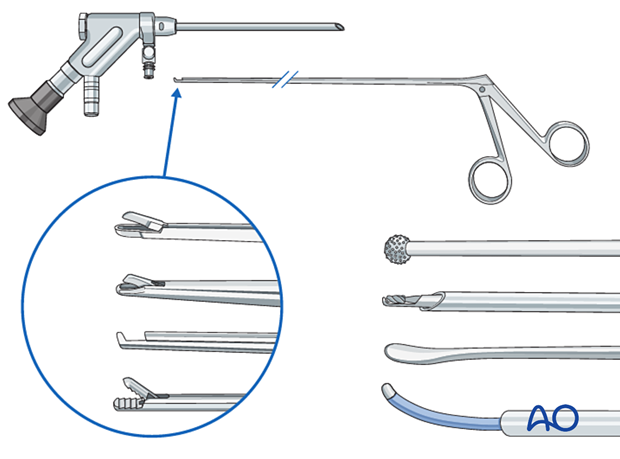
2. Required instruments
The following specialized instruments are recommended for this procedure:
- Endoscopy cart (video, pump, radiofrequency unit, drill)
- Interlaminar endoscope
- Blunt dissector/spatula
- Micro-punch
- Grasping forceps
- Kerrison rongeur
- Bipolar coagulator
- Burr
- C-arm
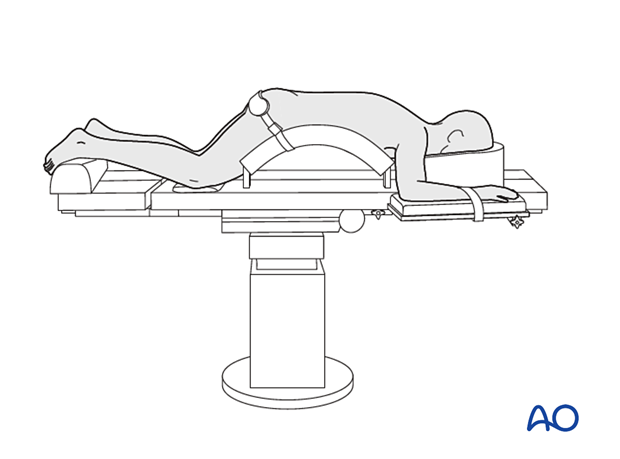
3. OR set up and patient positioning
The patient is placed prone on a Wilson frame or with pelvic and thoracic rolls.
4. Positioning of C-arm
In the AP view, adjust the C-arm until the:
- endplate of the caudal level is straight
- spinous process is centered on the disc space
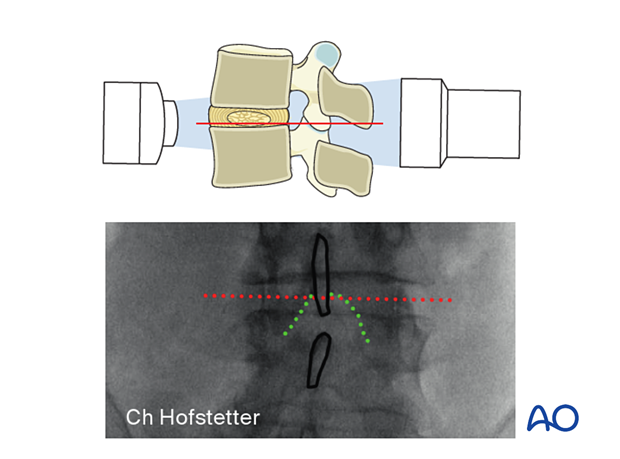
To obtain the largest window between the cranial and caudal lamina, tilt the C-arm to add 0–5° of kyphosis for the upper lumbar levels and 10–15° of kyphosis for the lower lumbar levels.
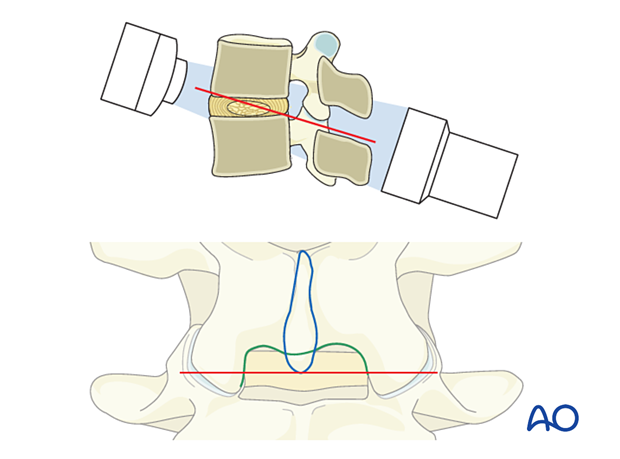
Optimizing the approach corridor to the lateral recess will minimize the need for bone resection.
5. Visualization of the surgical field
Incision
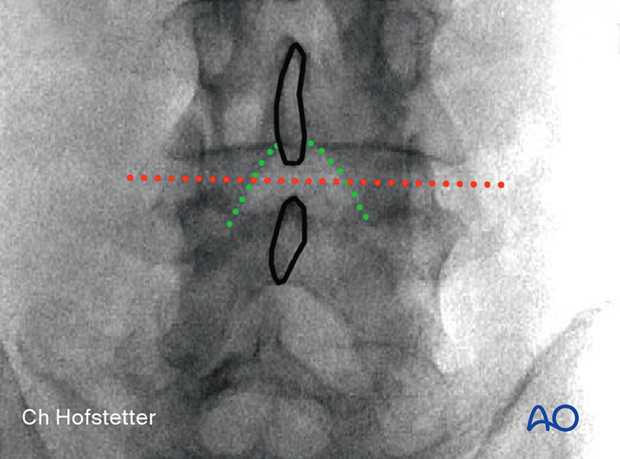
Use AP intraoperative imaging to identify the inferior medial edge of the cranial level on the ipsilateral side.
The incision line is marked at this line, centered over the disc.
The skin may be infiltrated as per the surgeon’s preference.
Use an 11-blade scalpel to make a 1 cm incision through the skin and lumbar fascia.
Insertion of dilators
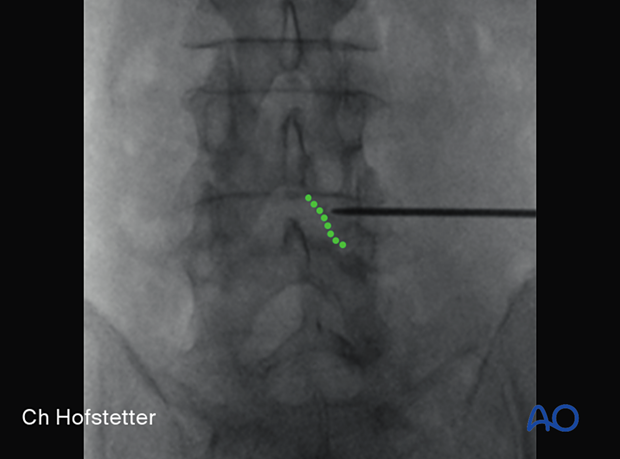
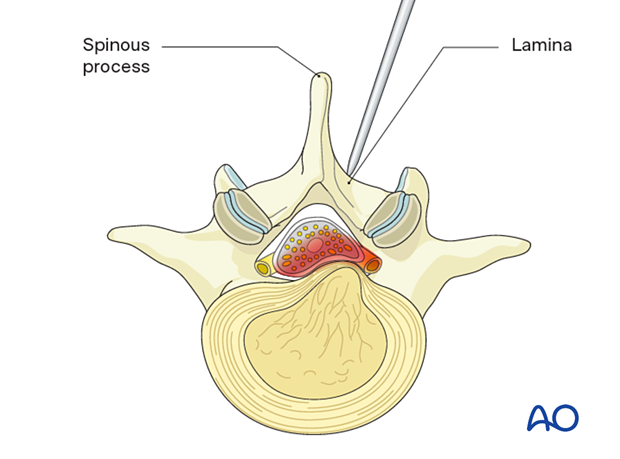
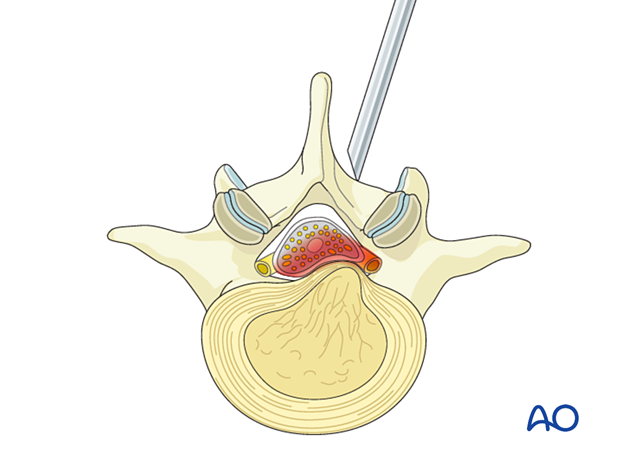
Insert the first dilator, angle it slightly medially, and “feel” for the spinous process and lamina base. The goal is to reach the inferomedial laminar edge.
After the first dilator has been positioned correctly onto bone, verify that it is located at the correct level using fluoroscopy.
Insert sequential dilators onto the inferomedial lamina edge.
Palpate to ensure that the dilators are docked on bone at all times.
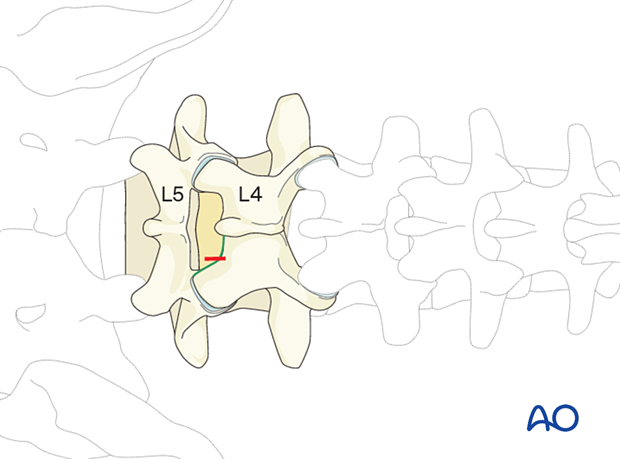
Once the desired dilation is achieved, insert the working sleeve onto the inferomedial lamina.
Ensure that the bevel of the working channel (ie, the shortest end) is facing medially. This will reduce the risk of dural injury if the working channel slips.
Use fluoroscopy to verify the correct position of the working channel in the AP and lateral view.
Visualization
Insert the endoscope into the working channel.
Use the bipolar coagulator and pituitary rongeurs to dissect tissue and identify the ligamentum flavum and the inferior medial edge of the lamina.
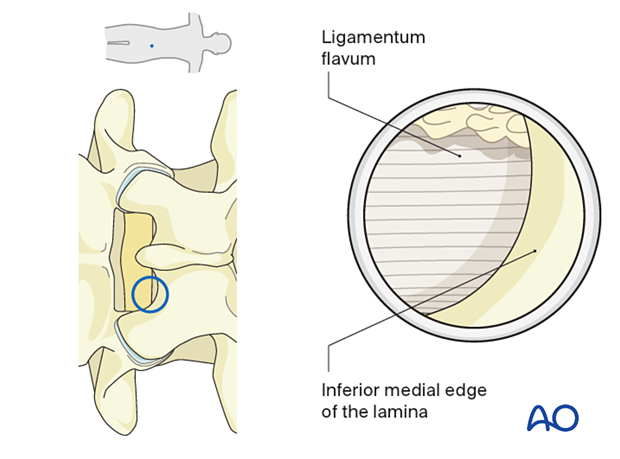
Laminotomy and medial facetectomy (if needed)
A laminotomy and medial facetectomy may need to be performed in upper lumbar levels or with posterolateral disc herniations.
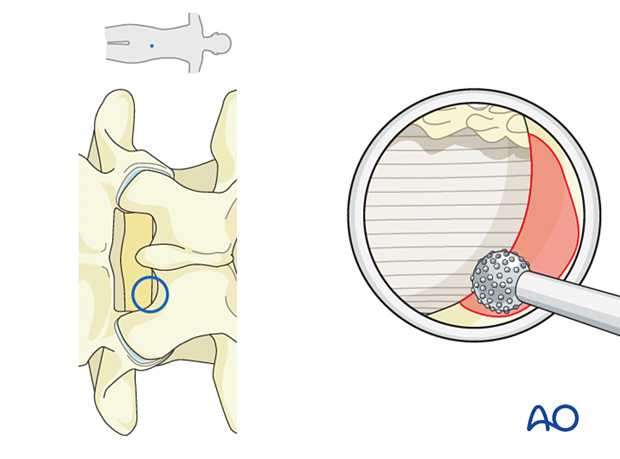
This can be achieved using a diamond burr and Kerrison rongeurs. Drilling is started at the inferior edge of the lamina.
This will provide adequate exposure to the traversing nerve root.
6. Enter the epidural space
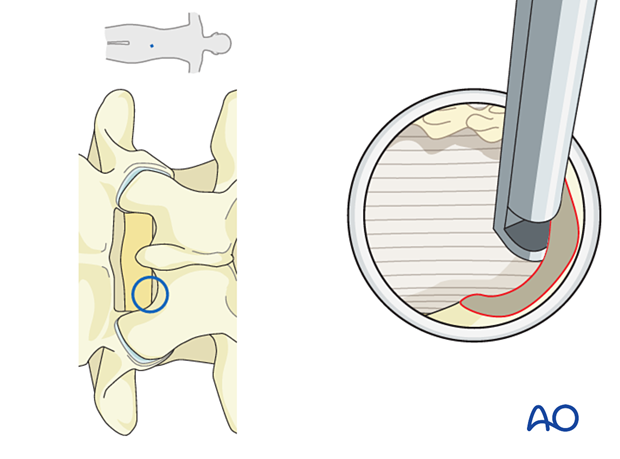
Once the ligamentum flavum is clearly visualized, use one limb of the micro-punch to pierce through the ligamentum flavum carefully.
Epidural fat should be observed at this point. Take small bites, first with the micro-punch …
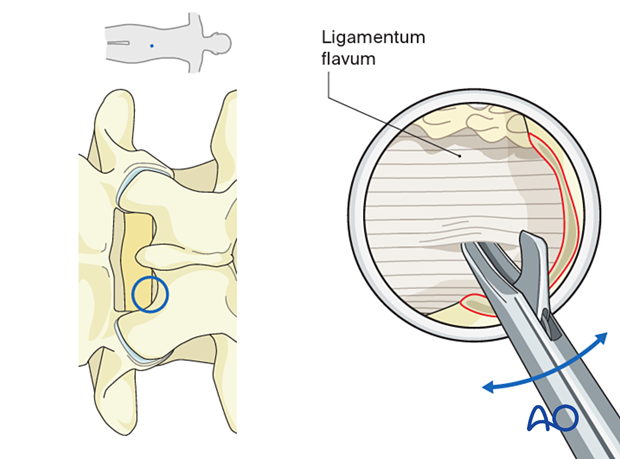
… then, with a Kerrison rongeur to expand the window through the ligamentum.
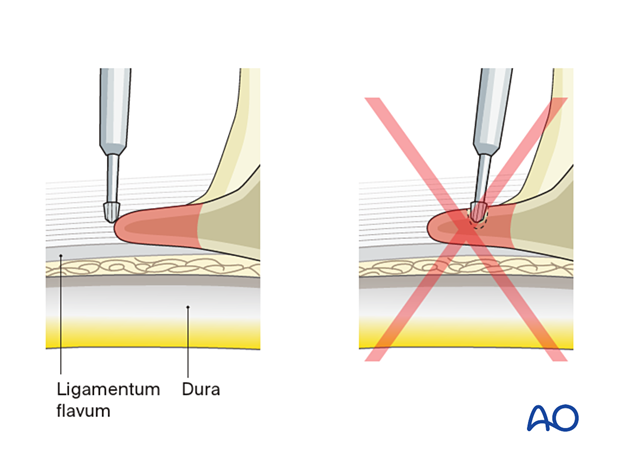
Care should be taken to visualize every bite to prevent dural injury.
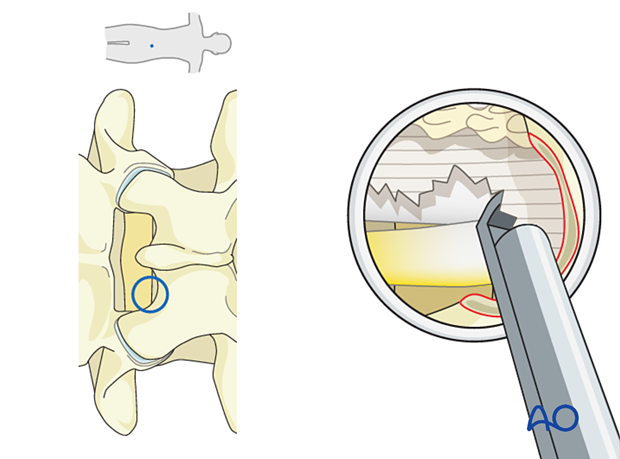
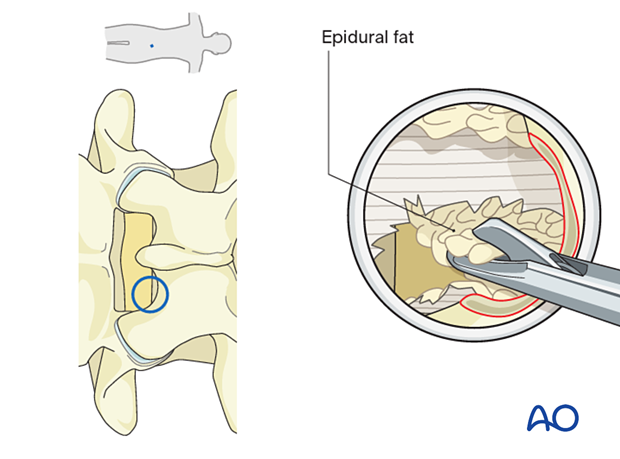
Coagulate any epidural veins and dissect epidural fat until a clear view of the neural elements is achieved.
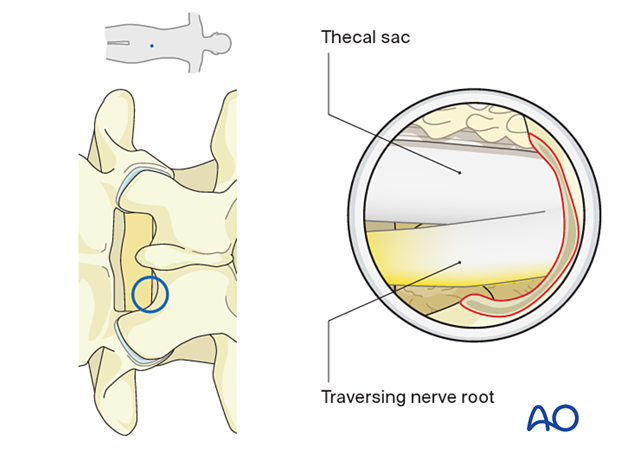
Identify the lateral margin of the traversing nerve root and mobilize it medially with a blunt dissector.
In some situations, the disc fragment is obvious at this point and can be resected with a pituitary rongeur.
If there is difficulty in mobilizing the neural elements, then additional lateral recess bony decompression may be required.
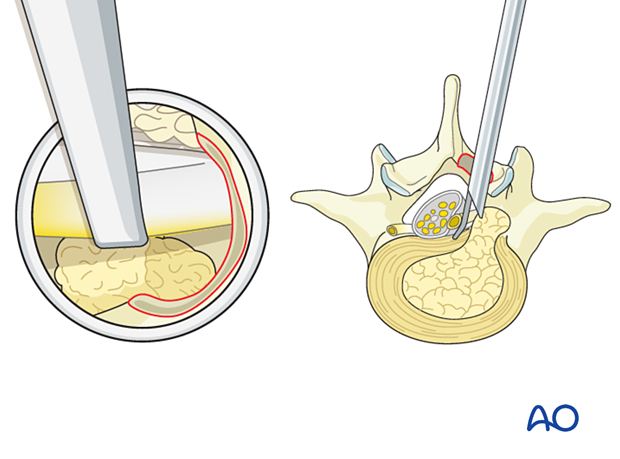
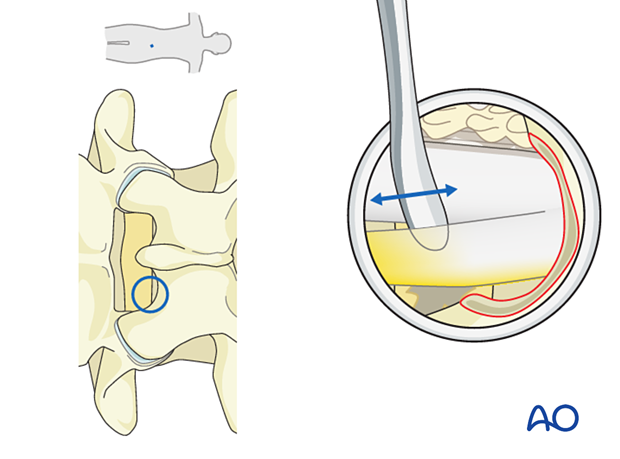
For further exploration or a contained disc fragment, rotate the working channel 180° so that the long end of the bevel protects the neural elements medially.
The disc should be fully visualized at this point.
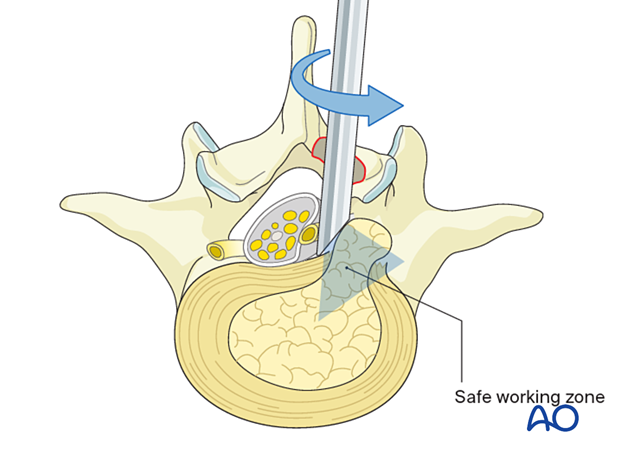
Use a pituitary rongeur to resect the disc sequestration and to explore the annular defect in cases of a contained disc fragment.
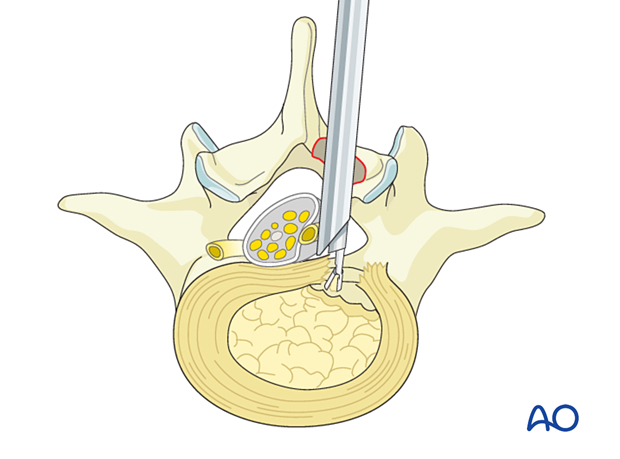
Use a dissector to verify that the nerve is easily mobilized.
If a dural tear occurs, no repair and bedrest may be sufficient for small tears, while larger tears and tears with extrusion of nerve roots may require fibrin sealant and an inlay graft. Sometimes conversion to open or tubular surgery with direct repair of the dura may be necessary.
7. Working sleeve removal and closure
Hemostasis is achieved with hemostatic agents or bipolar cautery.
The tube is removed, and a deep dermal stitch can be placed at the surgeon’s discretion. A subcuticular stitch is used to close the skin.
8. Aftercare
The patient can usually be discharged on the day of surgery or the following day with a short course of pain medication and muscle relaxants.
Lumbar immobilization is not required.
Patients may feel incisional or muscular pain that usually subsides within a few days.
Patients can develop postoperative pain and muscle spasms in a delayed fashion.













