Lateral lumbar interbody fusion (LLIF)
1. Introduction
LLIF is one of the best minimally invasive surgeries for anterior support in the lumbar spine.
This procedure is mostly recommended for these levels:
- L2–L3
- L3–L4
Use of this procedure at level L4–L5 is debatable due to the anatomical configuration and the relationship of the vertebral space with the lumbar plexus, vascular anatomy, and shape and position of psoas muscles.

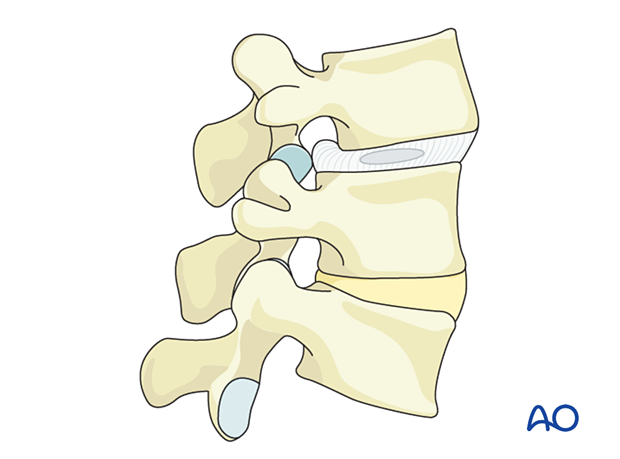
For this treatment description, we will use the L3–L4 level with spondylolisthesis with foraminal stenosis and degenerative disc disease.
2. Preparation
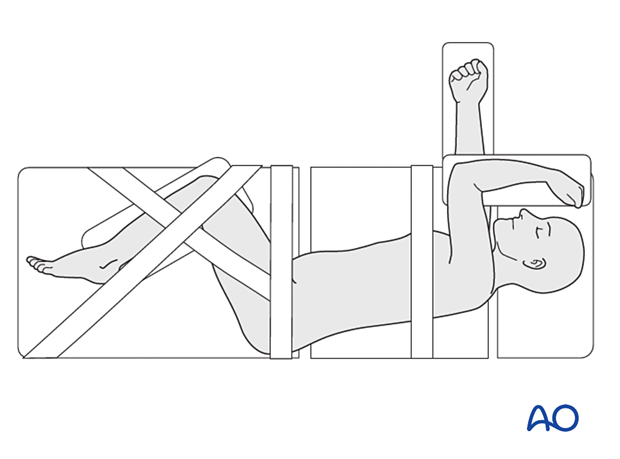
The patient is positioned in true lateral decubitus on a radiolucent surgical table. The side that the patient lies on should be chosen according to the pathology and the anatomical configuration.
3. Fluoroscopic identification of the target level before draping
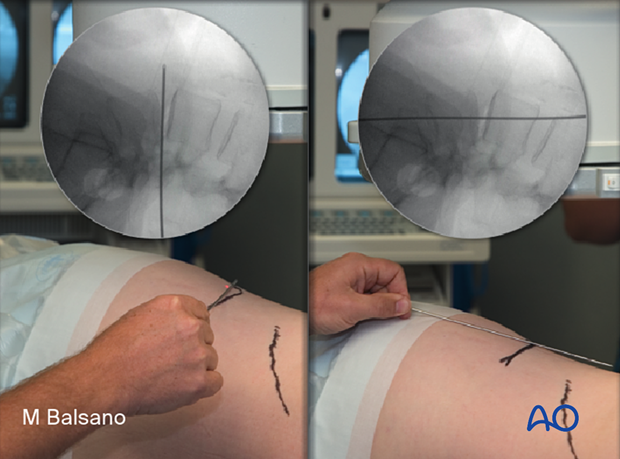
The correct operative level is determined using fluoroscopy.
The table should be adjusted so that the C-arm provides straight AP images at 0º and straight lateral images at 90º.
The position of the table may be adjusted at every level in deformity cases.
The spinous process and end plates must be aligned.
Alternatively, use 3D navigation to localize the correct level throughout the procedure.

It is helpful to use a localizer on the skin to identify the level and the incision position.
The center of the disc space is the target of the approach.
4. Approach
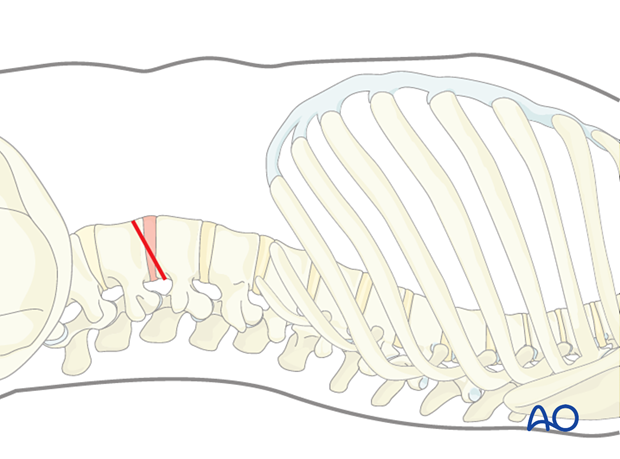
The incision line should be made exactly in the direction of the target. The incision length is usually approximately 3–4 cm (depending on how many levels will be treated).
A transpsoas approach is performed.
A tubular localizer is positioned through the muscle over the edge of the disc space. This position should be confirmed with AP and lateral views.


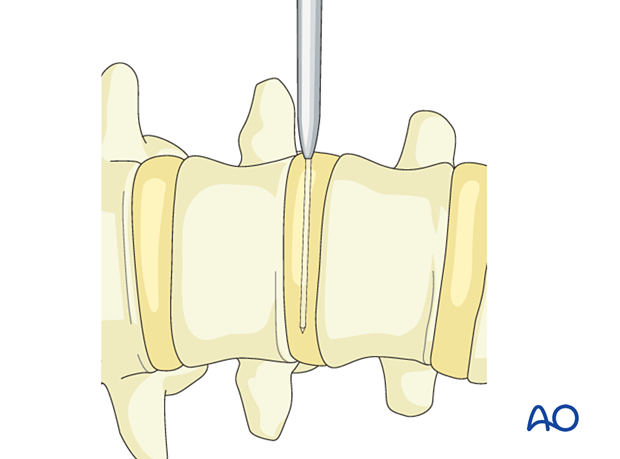
A K-wire is positioned inside the tube. This goes through the disc space and locks the tube in the correct position.
A series of dilators are used to increase the working area.
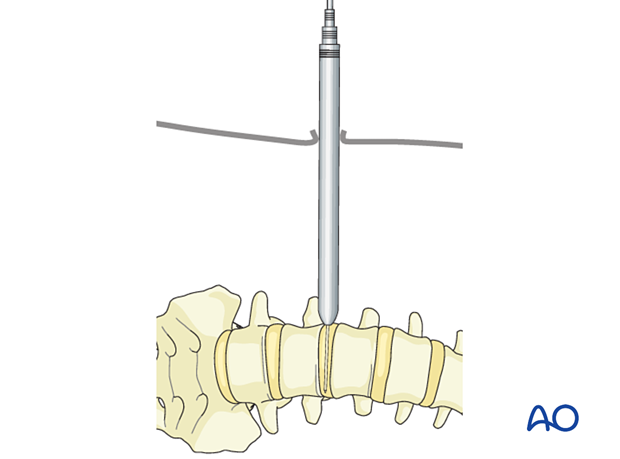
A self-retaining retractor system is highly recommended to lock the retractor in the correct position during the procedure, avoiding possible movements that can injure nearby structures (the peritoneum and vessels).
The length of the blades is adjusted according to the patient's size. The opening of the blades should not exceed the size of the instruments that are used for the disc preparation. This can protect the patient from bleeding and neurological issues.

5. Disc removal
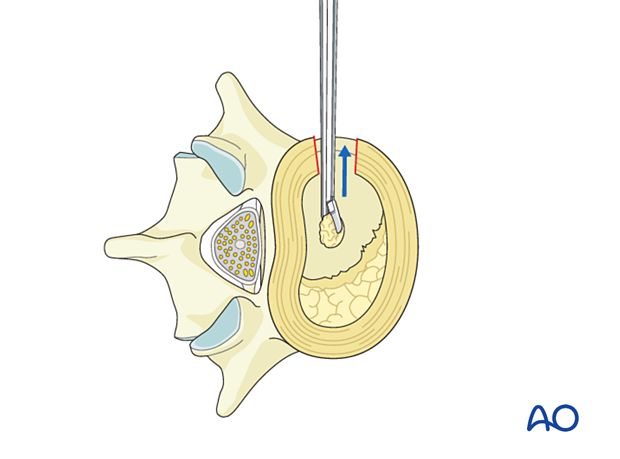
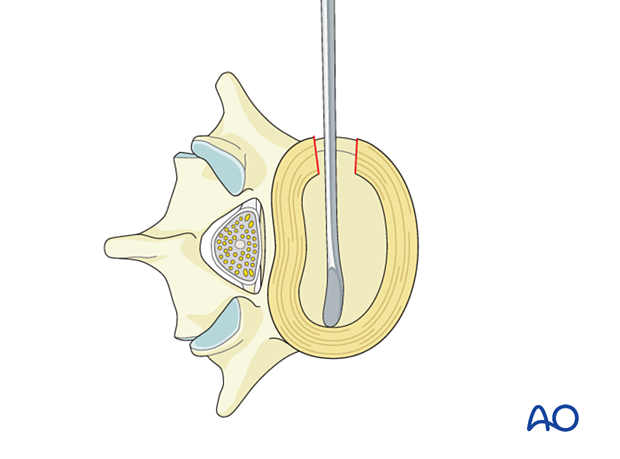
The annulus is opened in a small square using a sharp blade, avoiding injury to the anterior longitudinal ligament (ALL) and the posterior longitudinal ligament (PLL). The size of the incision should not exceed the size of the planned cage.
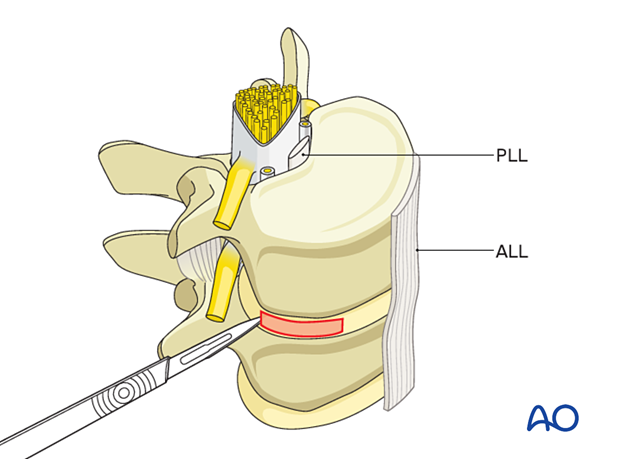
A pituitary punch is used for enucleation.
A Cobb elevator is moved into the created space until it reaches the contralateral annulus.
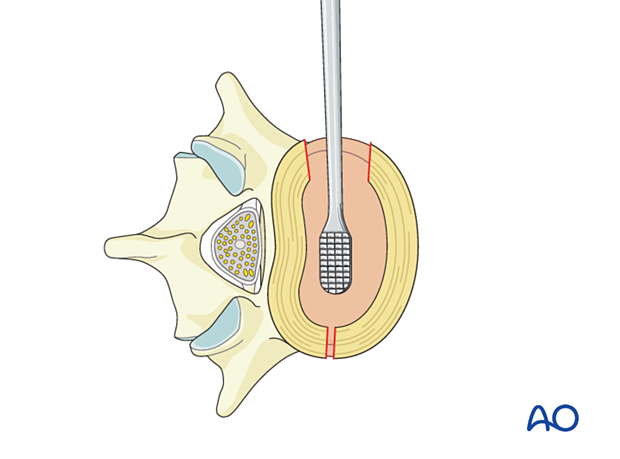
Gentle pressure is applied to the top of the Cobb elevator so that it passes through the contralateral annulus.


At this point, a standard preparation of the disc space is performed, and the remaining nucleus is removed.
The frontal area of the annulus corresponding to the size of the planned cage is also removed.
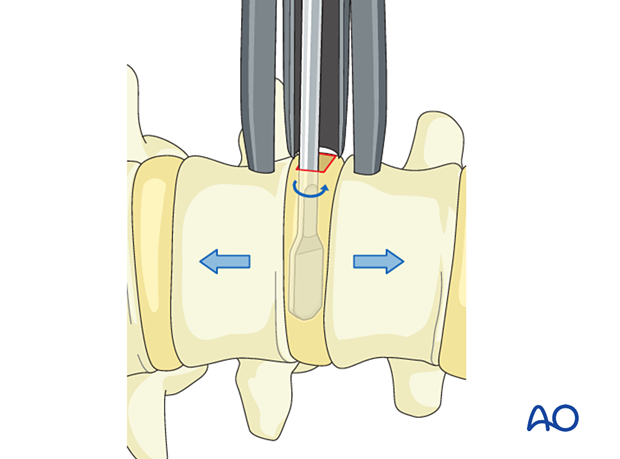
Using proper instrumentation, gently distract the disc space without harming the end plate.
6. Cage selection
The preoperative selection of a suitable cage (considering size and material) is mandatory. The most commonly used width is 22 mm. The height and shape of the implant depend on many factors:
- Previous height of the disc space
- Osteophytes
- Condition of facet joints
- Deformities
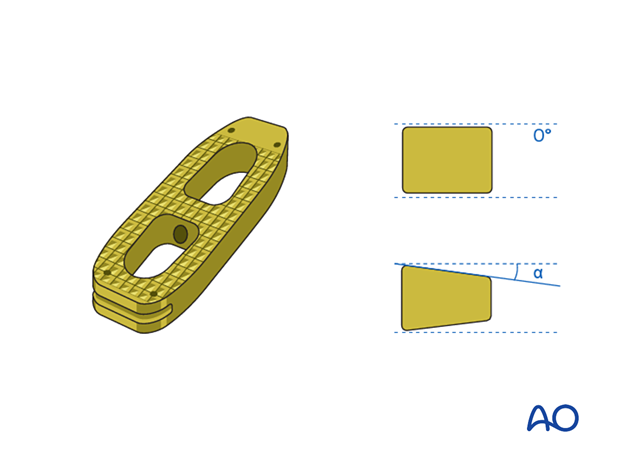
The cage must be filled with bone graft or bone substitute to ensure a valid fusion.

7. Cage insertion
The cage must be securely attached to the cage inserter to avoid misplacement. The cage is then inserted, and a press-fit is achieved.
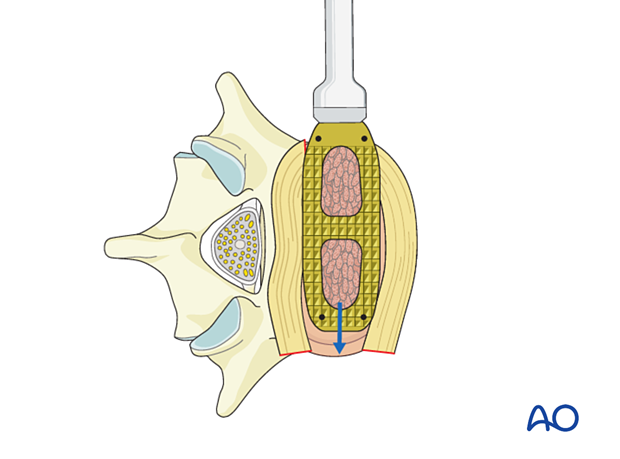
The use of correctly sized cages that reach the contralateral ring apophysis is recommended.

The final cage position should always be checked with the C-arm in AP and lateral views.
8. Additional instrumentation
Stand-alone cages should only be used in carefully selected cases.
Different types of additional fixation can be used according to the preoperative planning:
- Open or percutaneous screws
- Plates

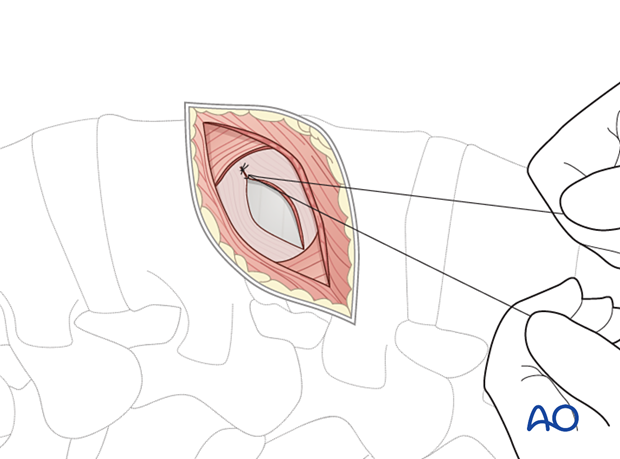
9. Closure
Suture of the wound should be done in a standard fashion, usually without using drainage.
10. Aftercare
Patients can usually stand on the first day after surgery and can be discharged on the second day after surgery.
For the first month after surgery, it is recommended that a brace is used to reduce the movements of the lumbar spine.
Postoperative physiotherapy is not essential but can be useful in some selected cases.













