Cervical disc herniation
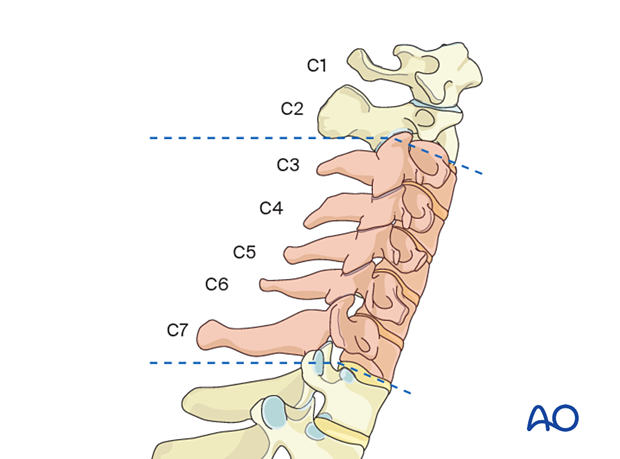
Cervical disc herniations occur in the subaxial region. Typical presentation includes symptoms of cervical spinal cord or nerve root compression. These include radiculopathy, sensorimotor deficits, and neck pain. These most often manifest in the upper extremities. However, they can also cause occipital neuralgia and pain or discomfort in the scapular regions.
High-grade spinal cord compression can result in spondylotic cervical myelopathy. This presents upper motor neuron pathology symptoms, including fine motor deficits, hyperreflexia, clonus, and gait imbalance. In some situations, these findings can present without any associated pain.
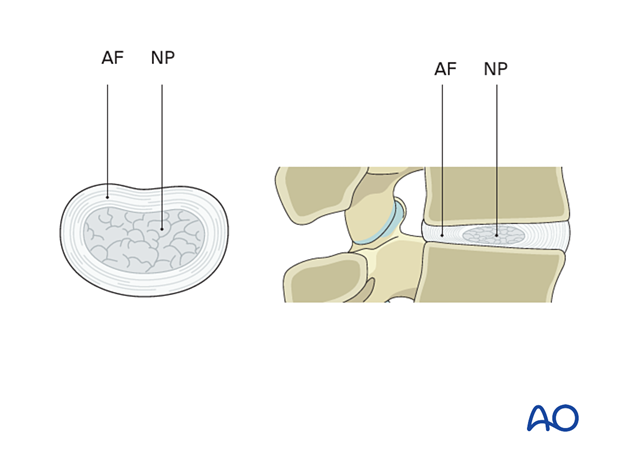
The intervertebral disc is built up of a thick collagen-rich annulus fibrosis (AF) containing a gelatinous proteoglycan-rich nucleus pulposus (NP).
Tears or weakening of the AF can result from degenerative changes or trauma and result in bulging or expulsion of NP material, leading to compression of surrounding neural structures.
The consequences of disc herniation will depend on the neural structures at the location of the disc herniation.
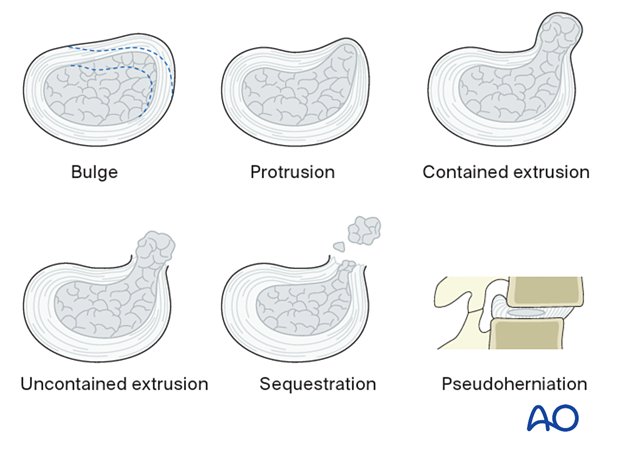
Six different types of disc pathologies can be seen:
- Bulge (without herniation)
- Protrusion (prolapse): the displaced material is less than the base of the displaced material
- Contained extrusion: the displaced material is wider than the base of the displaced material, and annular fibers are intact
- Uncontained/defect extrusion: materials extrude beyond an annular defect
- Sequestration – discontinuous with native disc
- Pseudoherniation – the appearance of a bulging disc due to spondylolisthesis. Note that the disc material does not extend posterior to the posterior spinal line.
Protrusion, extrusion, and sequestration are collectively referred to as disc herniations.