Posterior fusion of L5-S1
1. Introduction
Basic principles
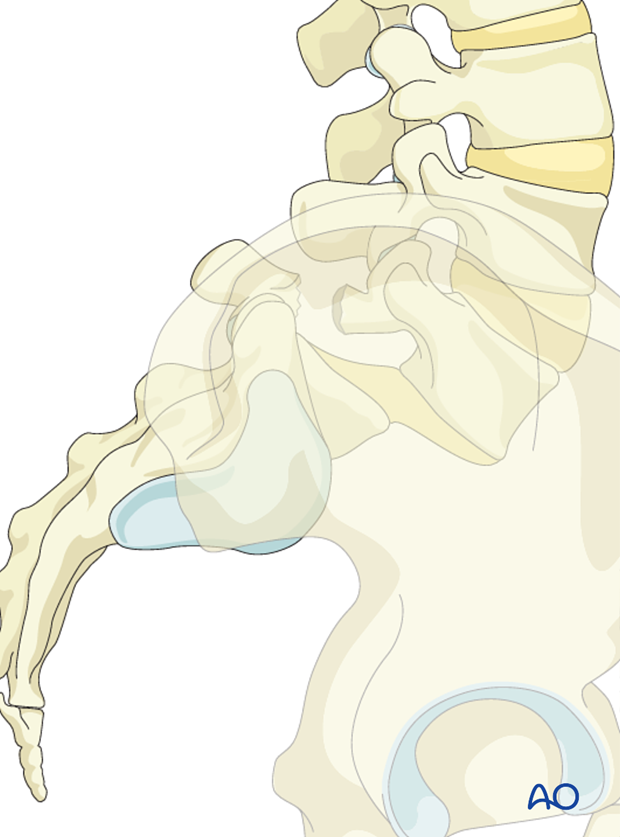
Managing spondylolisthesis requires good knowledge of lumbosacral anatomy.
The goals of the surgical management are:
- Solid fusion across L5-S1
- Neural decompression
- Ensure sagittal balance
- Prevent further slippage
- Reduce pain
- Maintain neurological integrity
Identification of anatomical landmarks
Due to the distorted anatomy care must be taken to confirm correct fusion levels. Typically the L5 pedicle is extremely anterior, hidden beneath the sacral alar.
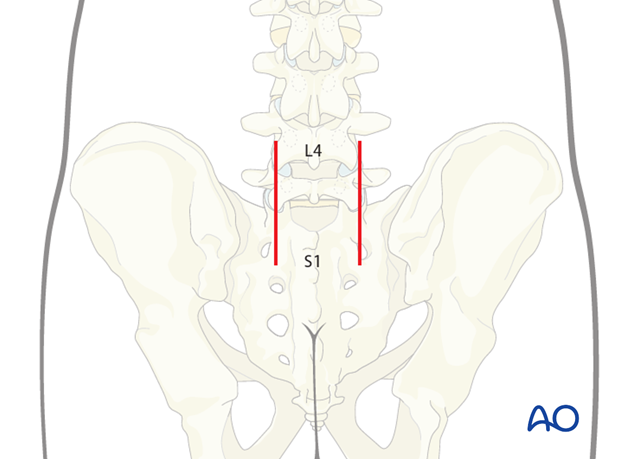
Intraoperative fluoroscopy or spinal navigation is used to facilitate identification of correct levels.
2. Prepartation and approach
This procedure is performed through the Wiltze approach with the patient placed prone.
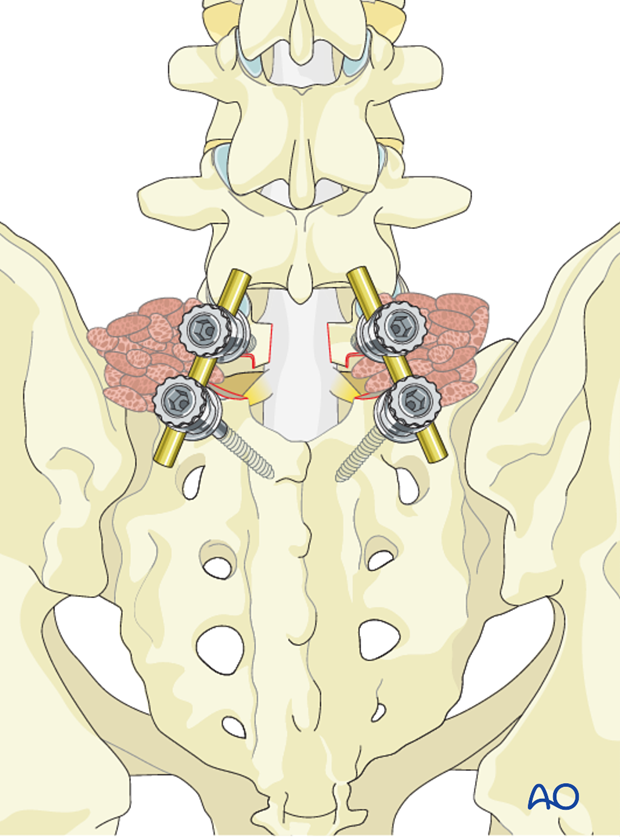
3. Pedicle screw insertion
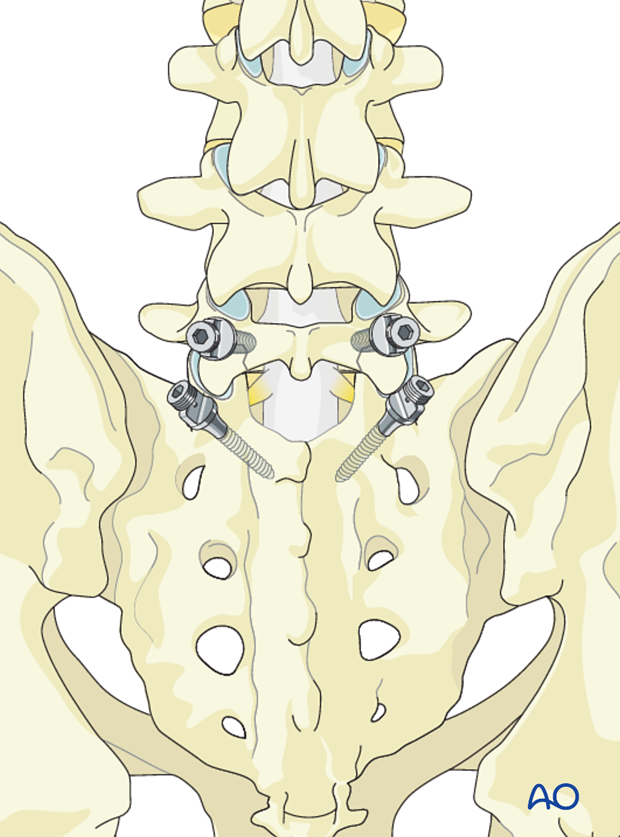
Pedicle screw insertion in L5 and S1 is performed in a standard fashion, ensuring that the proximal facet is not breached by the pedicle screw.
4. Interbody fusion
Interbody fusion is performed via a transforaminal approach.
Due to the anterior listhesis the course and location of L5 nerve root places it at risk. Great care is therefore taken to identify and protect it during facet and disk removal.

Facet removal
Facet removal may be performed if wide decompression is needed.
The inferior facet of L5 and part of the S1 superior facet is removed bilaterally to give access to the L5-S1 disk space.
Care is taken not to injure the L5 nerve.
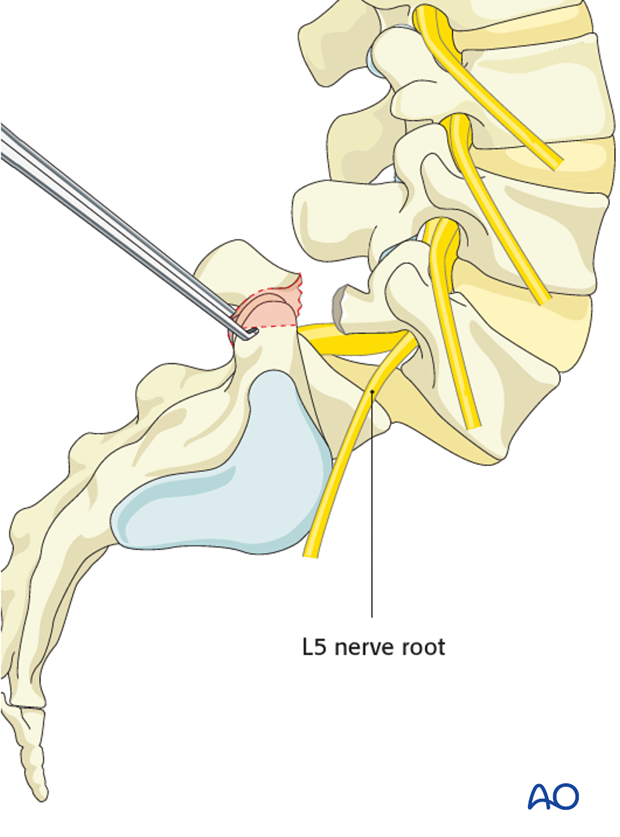
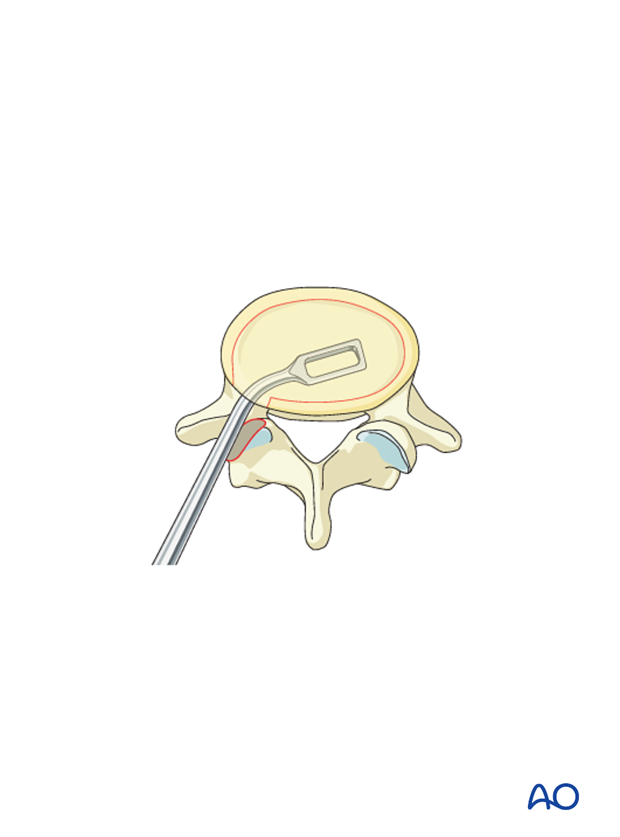
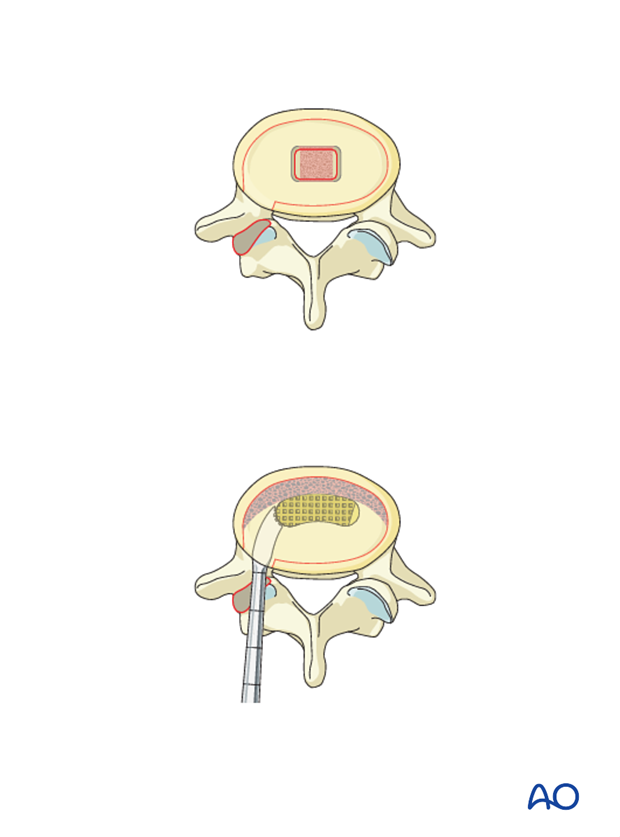
Disk removal
The disc is removed by incising the anulus fibrosis and using a series of Kerrison rongeurs and curettes forward to the anterior anulus. Care is taken not to disrupt the anterior anulus.
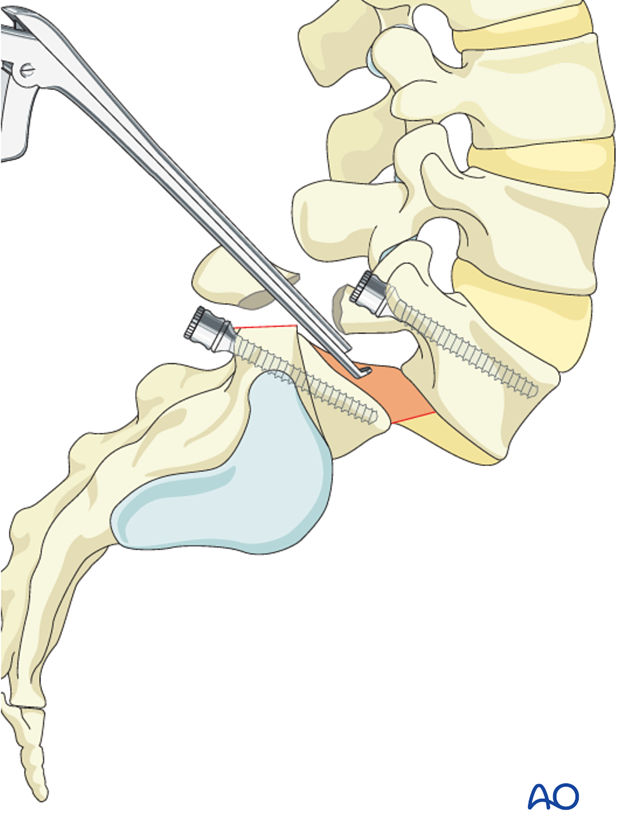
The endplates are cleared for all traces of cartilaginous material to ensure fusion.
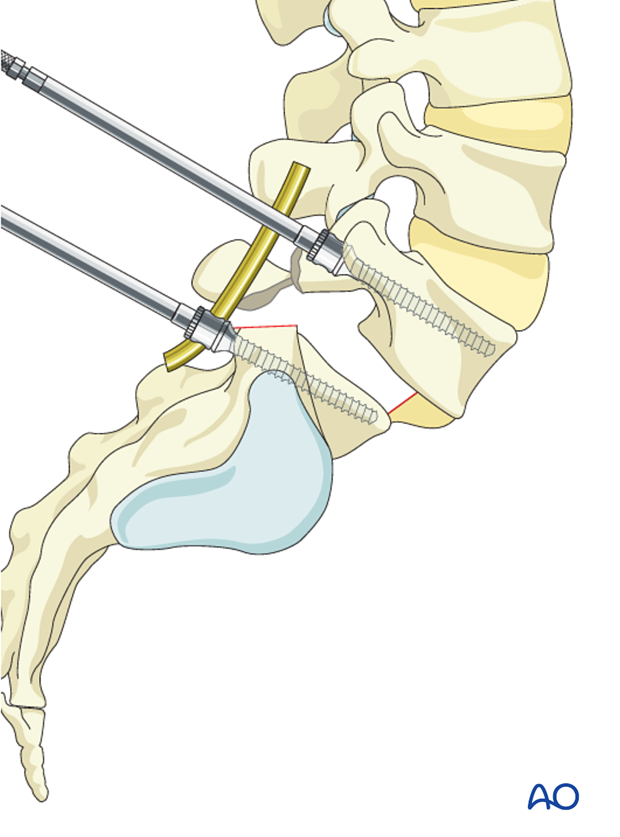
Reduction
Careful reduction maneuvers can be applied to bring back the L5 vertebra. Anatomical reduction is not always necessary.
The rods are contoured to accommodate both the S1 and L5 pedicle screws. The rods must respect the achieved L5-S1 lordosis.
During this maneuver the L5 nerve roots EMG's must be monitored to avoid postoperative foot drop.
Grafting
Once the intervertebral disk space has been mobilized, and (if necessary) reduction performed, the disk space is packed with cancellous bone.
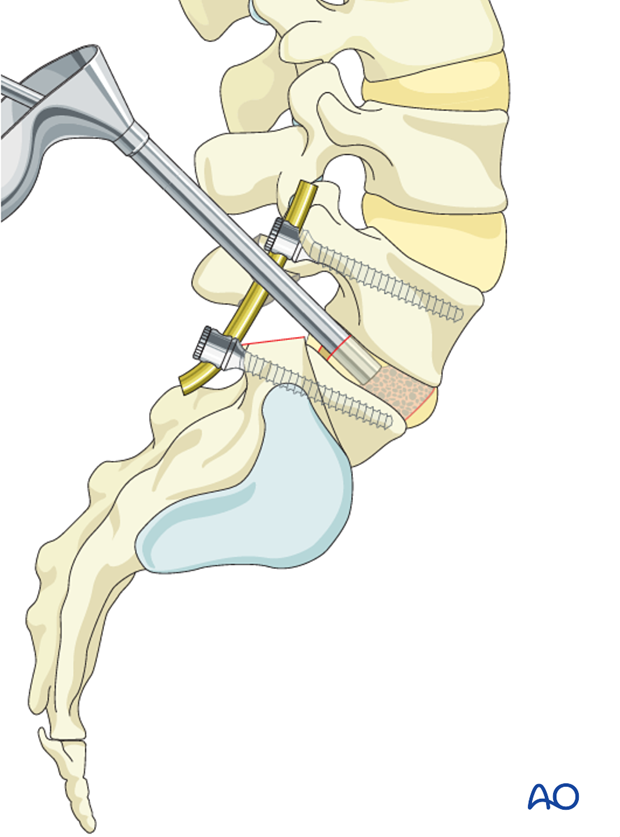
Anterior interbody structural bone graft is impacted providing anterior structural support.
The structural graft should be placed as anterior as possible in order to achieve more lordosis.
Care must be taken to ensure that the structural graft is resting between both endplates.
A cage can be used instead of the structural bone.
High grade listhesis are at higher risk of graft extrusion.
5. Posterior lateral fusion
Posterior lateral fusion should be carried out across the transverse process of L5 to the sacral ala.
Bone graft is impacted in the lateral gutters.
6. Aftercare
Detailed postoperative neural assessment must be conducted, specifically looking at the integrity of the L5 nerve root as well as sacral nerves controlling bowel and bladder.
Patients with high grade spondylolisthesis that have been reduced are at high risk of postoperative foot drops secondary to neuro traction injury. To minimize such injuries patients are immediately placed in bed with knees and hips flexed. As long as no neuro injury can be identified the leg can be gradually extended after day two. If neuro injury can be identified, the period of flexion should be extended.
Patients are made to sit up in the bed on the first day after surgery. Bracing is optional. Patients with intact neurological status are made to stand and walk on the second day after surgery. Patients can be discharged when medically stable or sent to a rehabilitation center if further care is necessary. This depends on the comfort levels and presence of other associated injuries.
Patients are generally followed with periodical x-rays at 6 weeks, 3 months, 6 months, and 1 year looking for spinal fusion.
Patients with a diagnosis of dysplastic spondylolisthesis run a higher risk of cauda equina and require closer monitoring of their neurological status during and after surgery.













