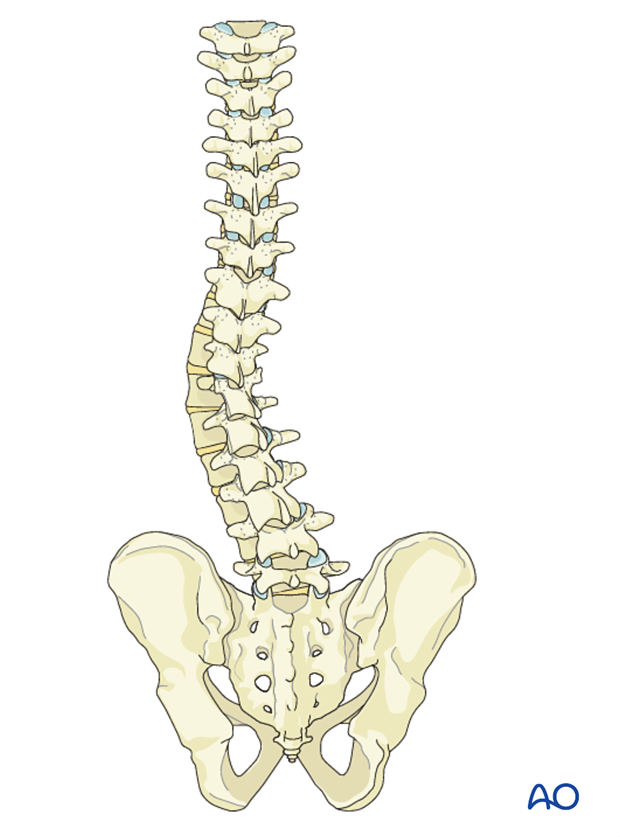
Anterior open
1. Introduction
The aims of surgery are to:
- improve the spinal curve,
- improve the three dimensional alignment of the spine,
- prevent progression of the curve in the future
- improve cosmesis
- reduce pain
- optimize pulmonary function
- maintain neurological integrity.
This is achieved by correction of the deformity and creation of a solid arthrodesis of the deformed part of the spine.
For this procedure we will assume a left lumbar curve.
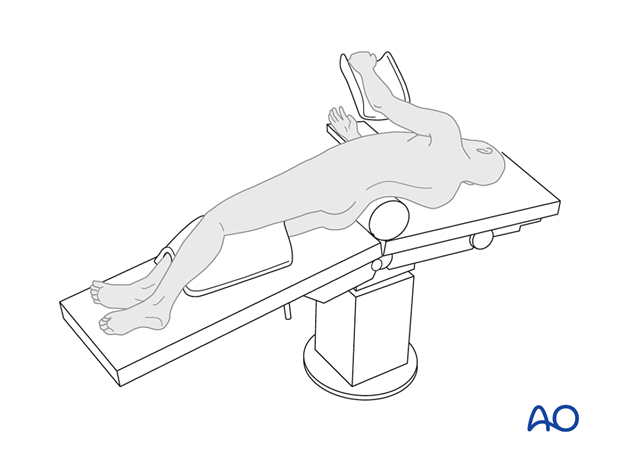
2. Approach and preparation
The procedure is performed with the patient in lateral decubitus through one of the folloiwng approaches:
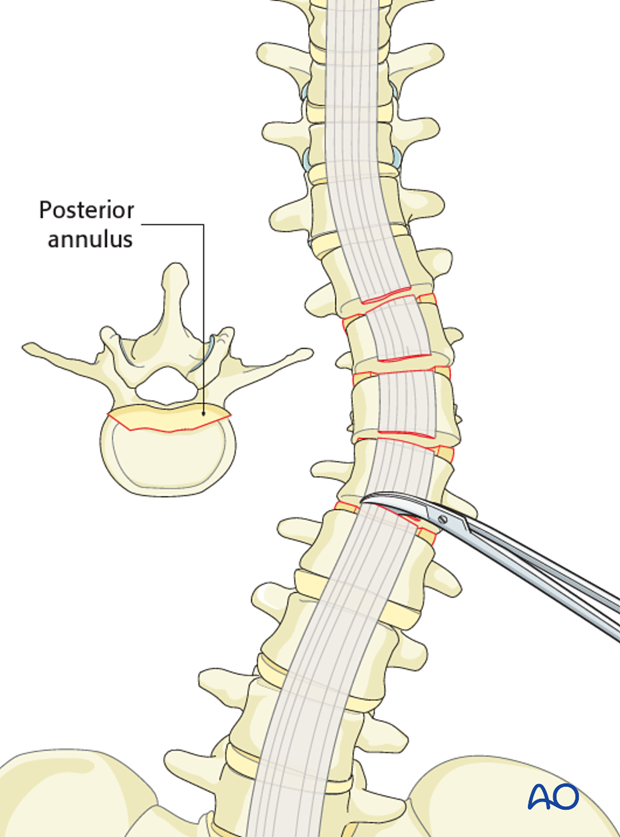
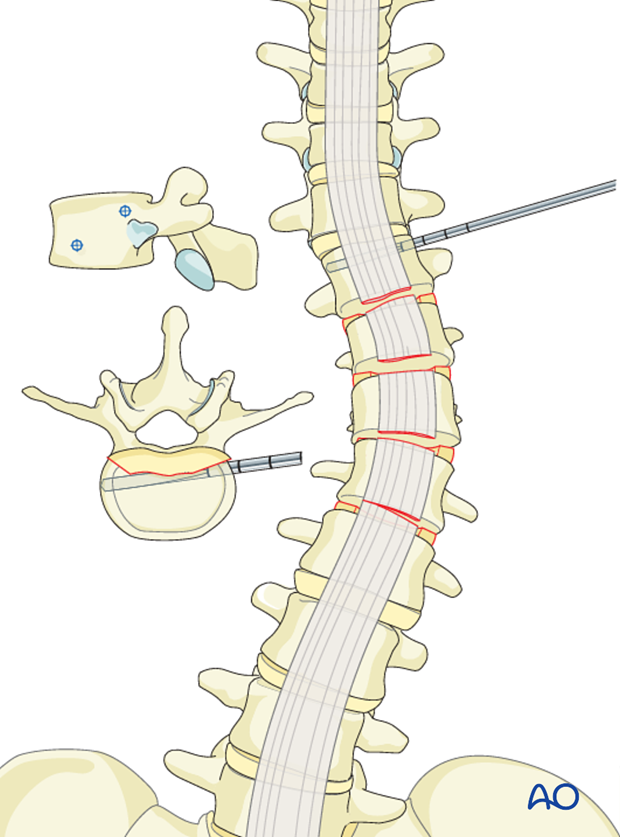
3. Release
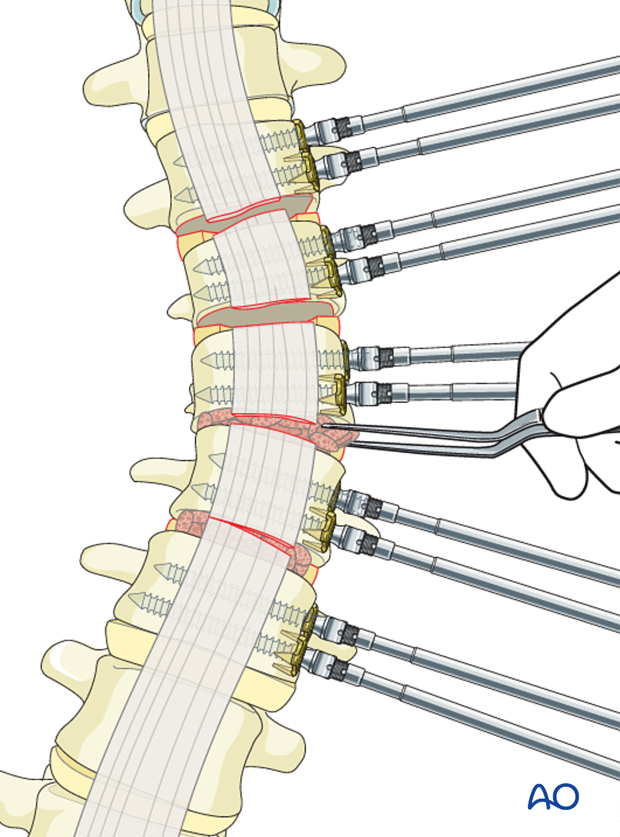
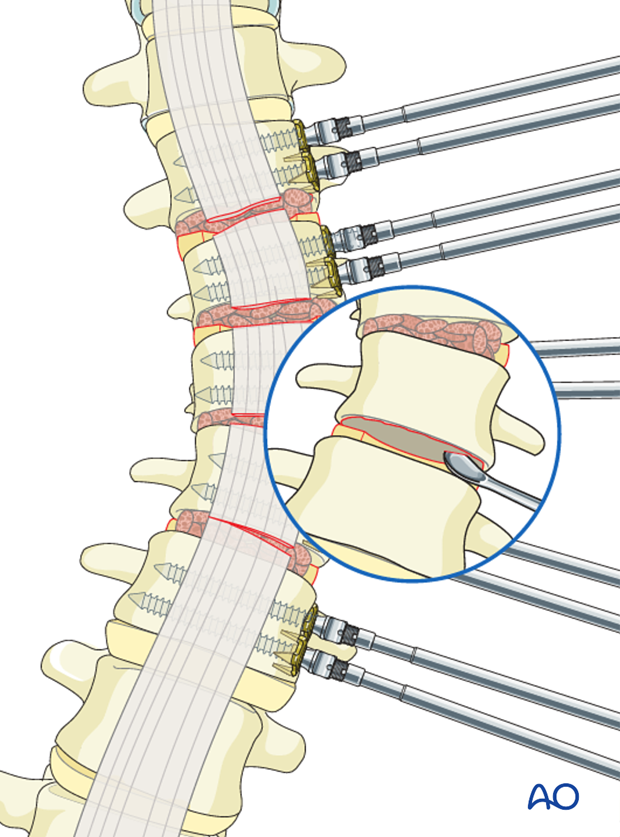
The anterior release consists of a thorough discectomy and resection of anulus of every intervertebral disk within the instrumented area of the spine.
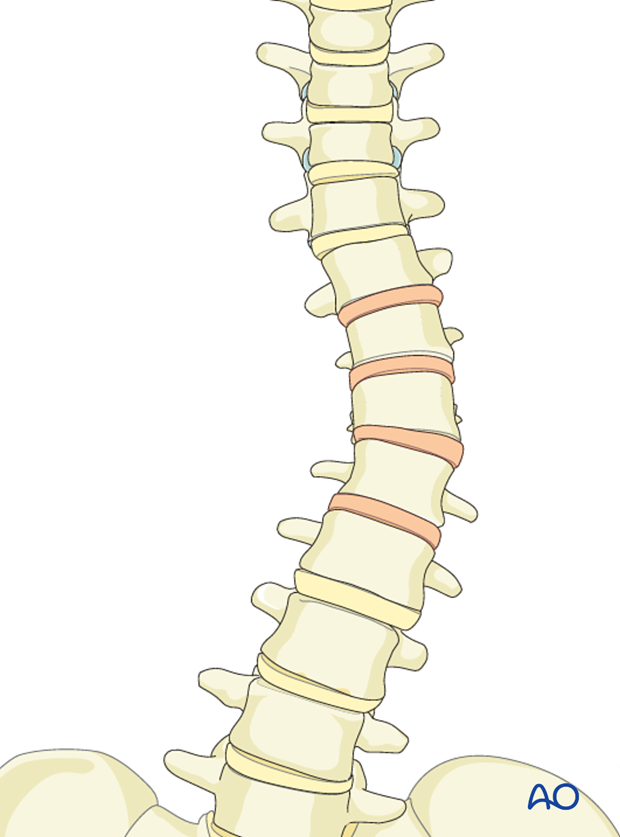
The annulus is incised from the lateral aspect of the spine, with curettes and rongeurs the disk is removed. The anterior longitudinal ligament is cut making sure that the anterior vessels (aorta and caval vein) are protected at all times. The posterior annulus may be removed in large rigid scoliotic curves but this may not be necessary for all cases, and it does increase the risk of inadvertent penetration into the spinal canal.
4. Instrumentation
Generally the curve is instrumented from end vertebra to end vertebra, with two bicortical screws at every level. Further details on selection of fusion levels can be found here.
A double rod construct is preferred because of increased biomechanical stability.
When a single rod construct is used, the screw is placed through the vertebra equator.
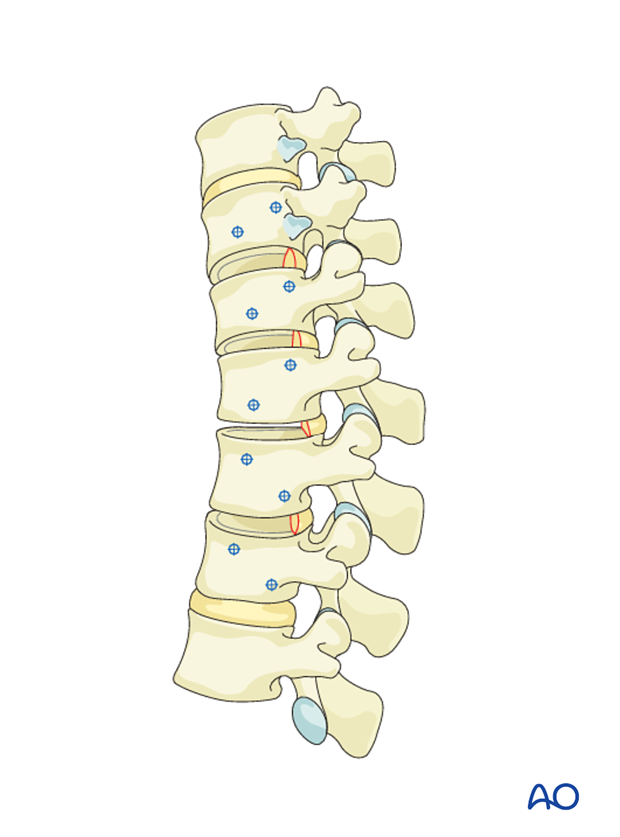
Screw placement
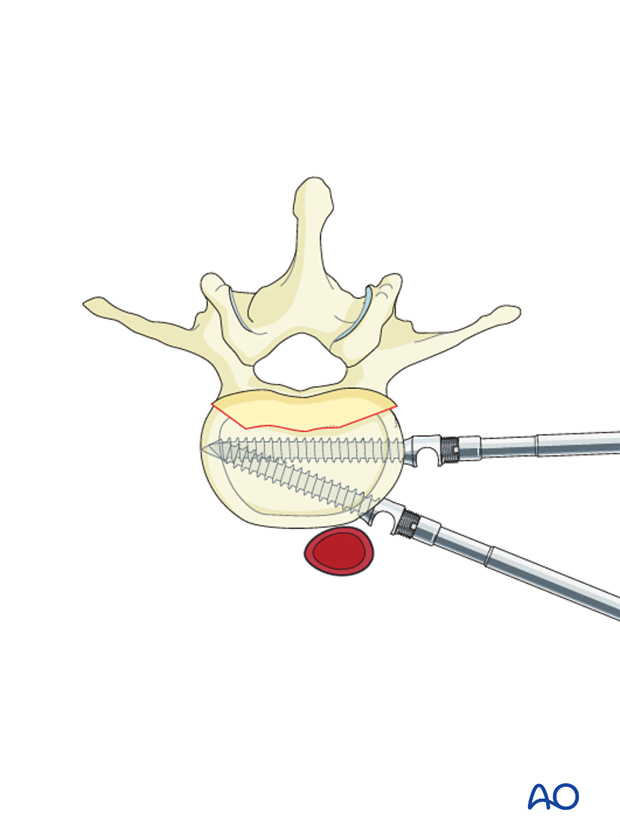
The screw holes are prepared using an awl and a probe. Generally a drill is not required. The screws are inserted transversely from one lateral cortex to the contralateral cortex.
On the contralateral side of the vertebrae lies the psoas muscle, and a few mm prominence of the screw tip can be tolerated.
Posterior screw
In the thoracic spine 1 cm of rib head will need to be resected with a rongeur to be able to insert the posterior screw.
The posterior screw is aimed slightly anteriorly to avoid the spinal canal and placed parallel to the end plates.
If the posterior annulus has previously been removed, the spine canal can readily be visualized thus ensuring correct placement of the screw.
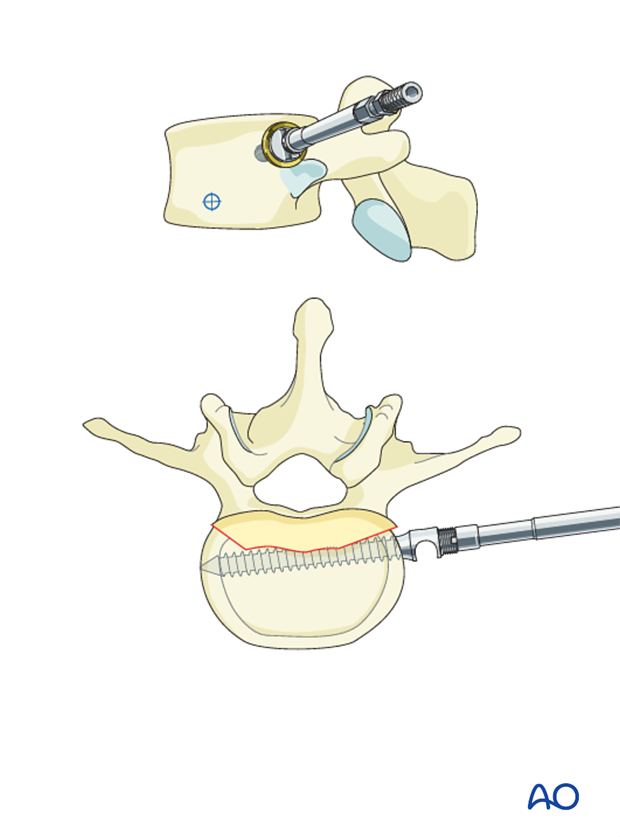
Anterior screw
The anterior screw is aimed slightly posteriorly and also parallel to the endplate. In this way the screws are triangulated and the pullout strength is improved.
Pitfall: Excessive anterior placement may impinge on the great vessels which needs to be avoided at all times.
This could be related to a too anterior insertion of the posterior screw eg. if the rib head has not been resected.
5. Bone grafting
Grafting of the lumbar spine
The arthrodesis (spine fusion) is achieved through an interbody fusion. In the lumbar spine it is essential to achieve lordosis and therefore structural interbody graft material is mandatory.
Structural rib graft supplemented with bone substitutes or iliac crest bone graft is placed in the interbody space.
As an alternative, a structural cage can be used to contain morsalized bone and provide structural support to create lumbar lordosis.
Eccentric placement of the cage (eg. More in the anterior concavity of the scoliotic curve) may help improve both coronal and sagittal correction.
It essential to fill the rest of the disk space with some form of morzalised bone graft or material to ensure a good fusion.
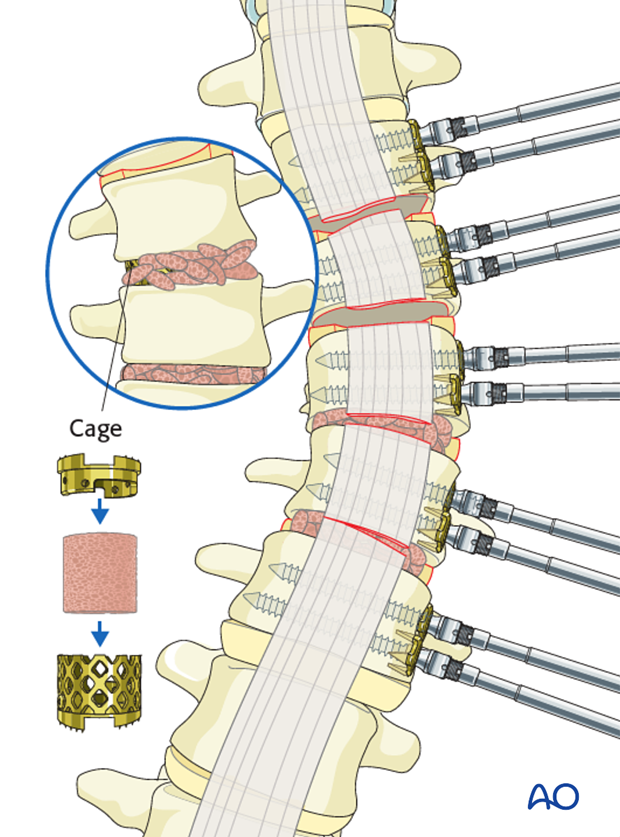
Grafting of the thoracic spine
In the thoracic spine, interbody cages are generally not required and bone on bone endplate contact with limited interbody morsalized bone graft is usually sufficient.
Pitfall: If the endplate cartilage is insufficiently curetted out, then bone fusion may not occur, increasing the chance of pseudarthrosis.
Pitfall: In the lumber spine, insufficient interbody grafting and support will lead to lumbar kyphosis and poor long term results as was seen with the early Dwyer and Zielke anterior instrumentations.
6. Correction of the deformity
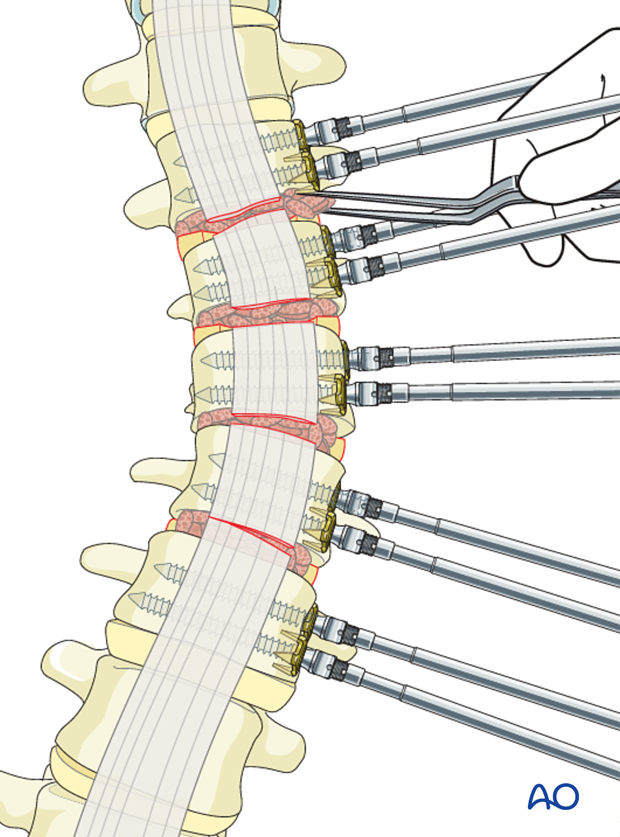
The discectomy shortens the anterior column of the spine and makes the motion segments more mobile. Because of these two mechanisms there is significant spontaneous correction of the scoliotic deformity.
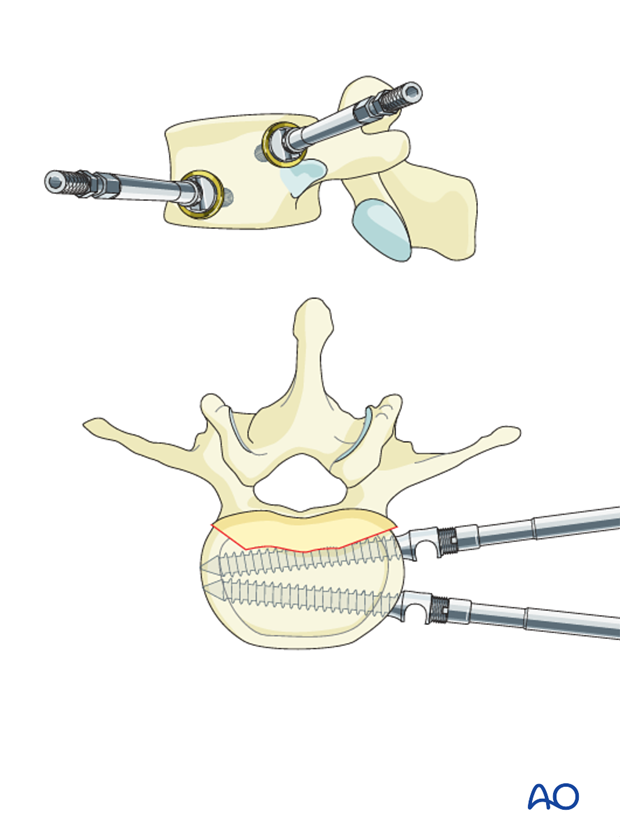
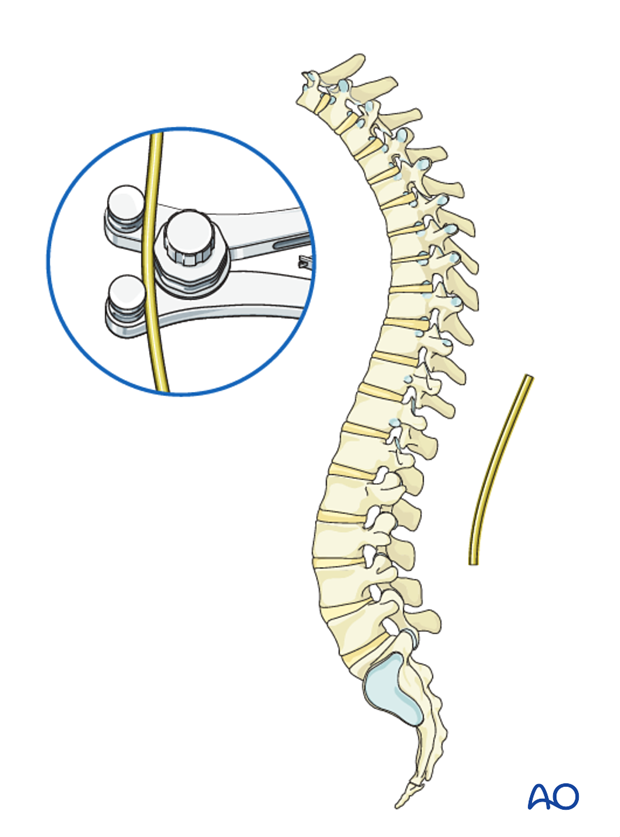
Rod bending
The rods need to be bent into the correct sagittal profile, which is a means a mild thoracic kyphosis and lumbar lordosis.
Rod insertion
First correction can be achieved by introducing one or both rods, locking the rods proximally in the screw heads and cantilevering the rods down into each subsequent level below.
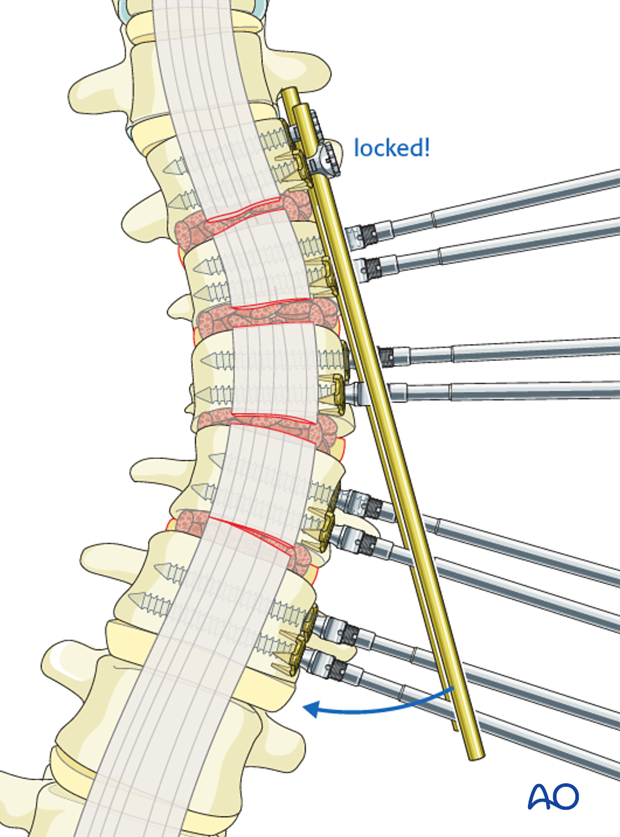
Pitfall: In case a single screw has been used in the UIV, it is best to lock the rod into the proximal two vertebrae before starting to cantilever, otherwise the proximal screw may pull out.
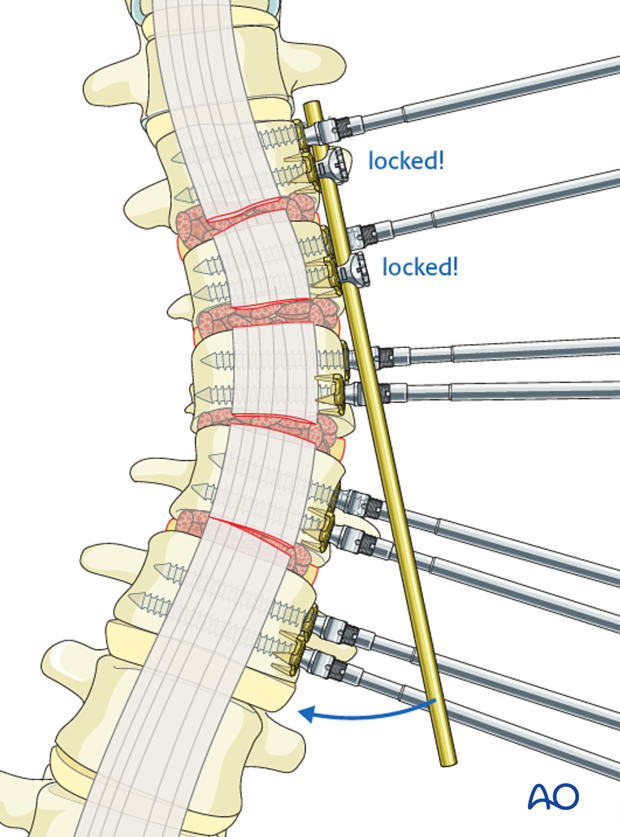
Compression
Second step consists of sequential compression across each disk space, and locking of the rods in each screw head, thereby improving correction and placing the interbody graft under compression.
Pitfall: Depending on the flexibility of the compensatory thoracic curve, usually the aim is maximal correction in the coronal plane.
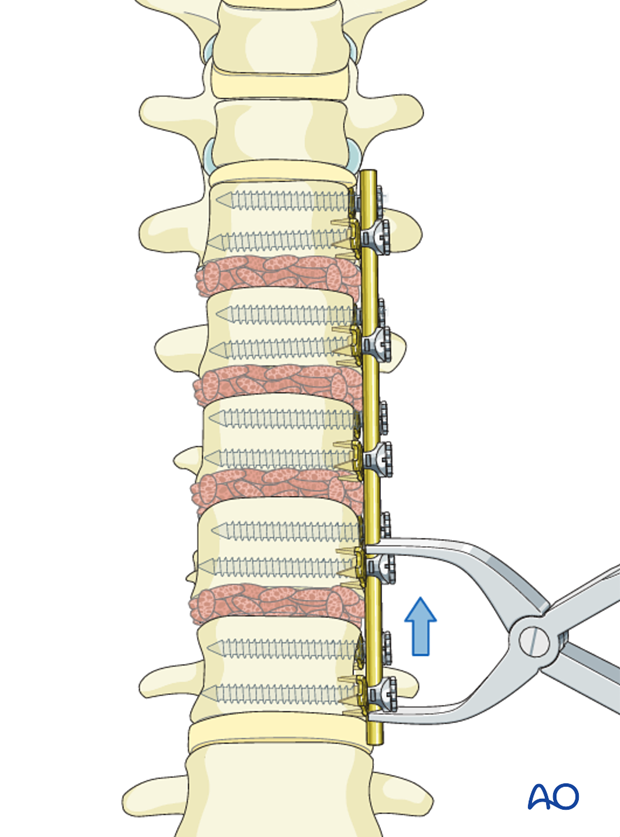
After the correction is completed, the rod will usually be a little longer than necessary.
This can be avoided by anticipating the necessary final length of the rod. At the beginning of the compression, the rod will not be long enough; however, at the end of the compression it will be long enough.

7. Aftercare following correction of spinal deformity
Immediate postoperative medication
Intravenous antibiotics are administrated for at least 24 hours, depending on hospital protocol. The use of an epidural pain catheter vs. intravenous patient controlled analgesia (PCA) are utilized for acute pain management.
Mobilization
Early mobilization out of bed, is preferably started the day after surgery. Generally a postoperative brace/orthosis is not required.
Postoperative imaging
It is appropriate to obtain upright PA and Lateral xrays of the patient at some point early postoperative either before the patient is discharged from the hospital or at the 1st postoperative visit as an outpatient
Restriction of activities
To allow the bone to heal and form a solid arthrodesis, some restriction of sports activities, especially contact sports, is usually advised for 6 months.
Postoperative complications
Early postoperative complications include:
- Postoperative wound infection
- Urinary tract infection
- Respiratory complications such as pneumonia
Late postoperative complications include:
- Pseudarthrosis with loss of correction
- Late deep wound infections
- "Adding on" which is progression of scoliotic deformity in the non-instrumented spine.
- Crankshaft phenomenon (progression of scoliotic deformity within the instrumented spine).
- Implant failure or other implant related complications
In the long term adjacent segment degenerations above and below the instrumented spine may occur.













