ORIF - Suture or screw fixation
1. Principles
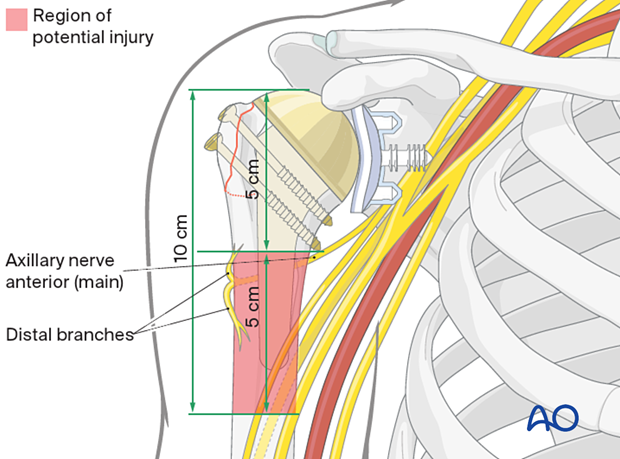
Shoulder pain and impingement are common with significant prominence of the greater tuberosity. Displacement of greater than 5 mm is currently recommended as the main indication for reduction and fixation in a stable humeral implant.
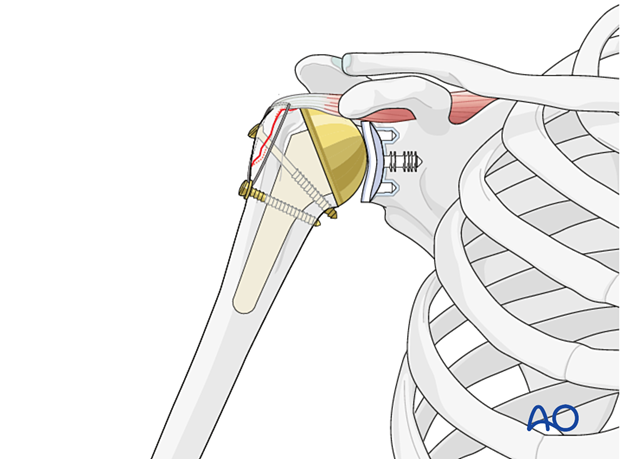
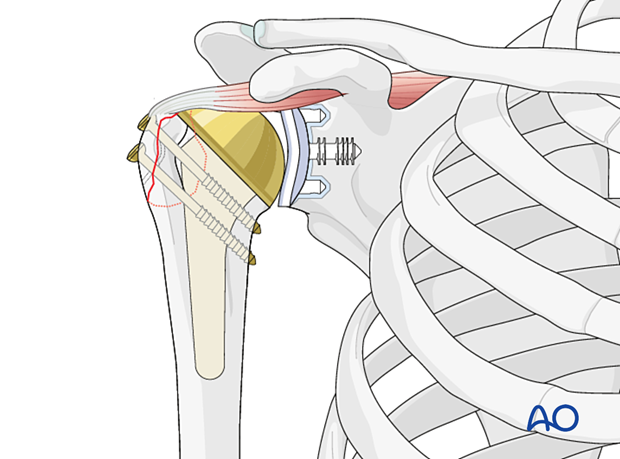
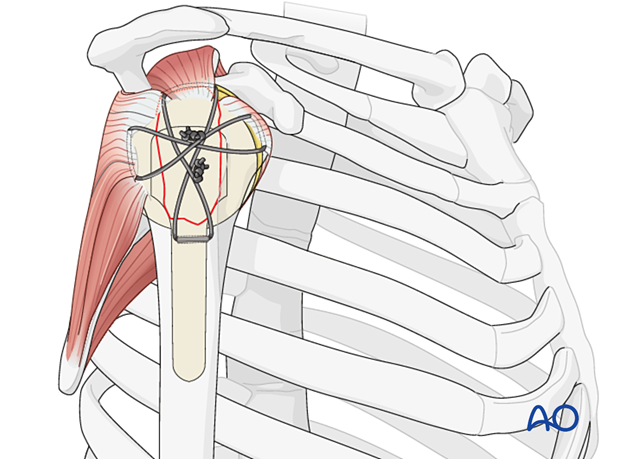
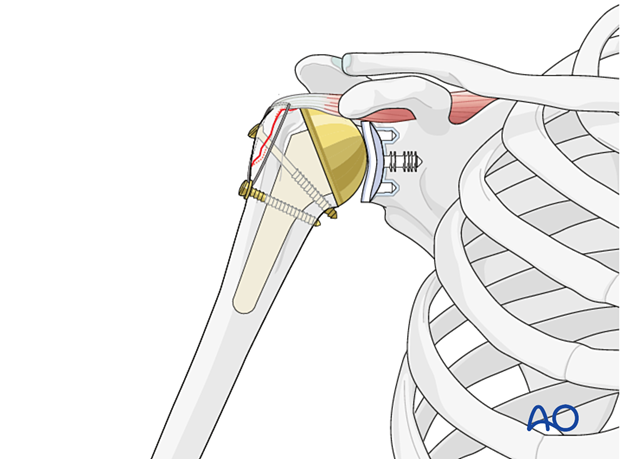
The presence of a humeral component means that there is often not enough available bone stock to perform an adequate screw osteosynthesis. For this reason, suture fixation is the preferred treatment option. An example of a completed construct is shown in this illustration.
Perfect anatomical reconstruction is needed for an anatomical shoulder prosthesis as rotator cuff function is a necessity for function.
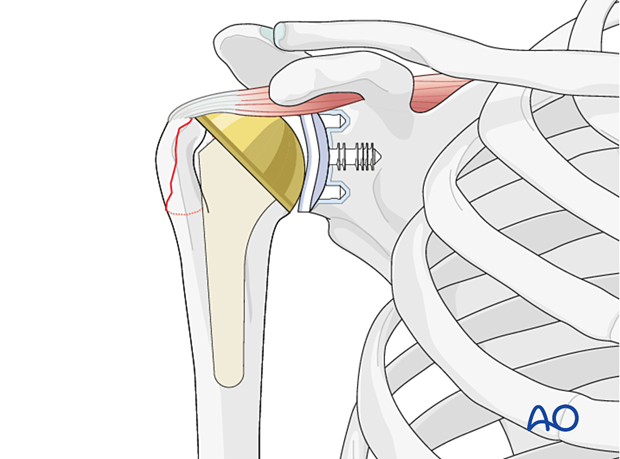
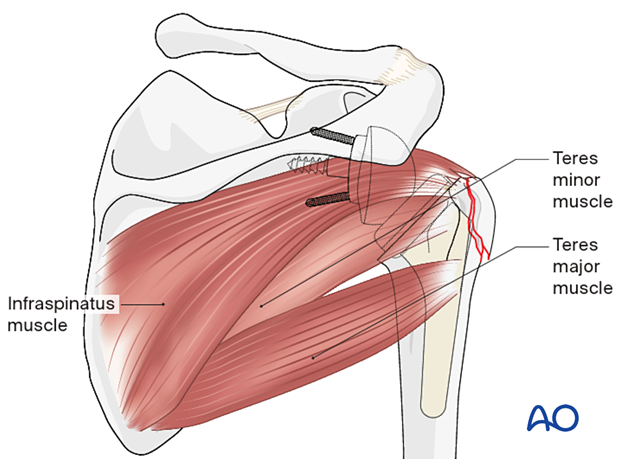
In the case of a reversed shoulder prosthesis, continuity of the infraspinatus/teres minor to the humerus is the objective, to keep strength in external rotation. A posteriorly displaced greater tuberosity may impinge between the humeral component and the scapula, blocking external rotation.
2. Patient preparation and approaches
Patient preparation
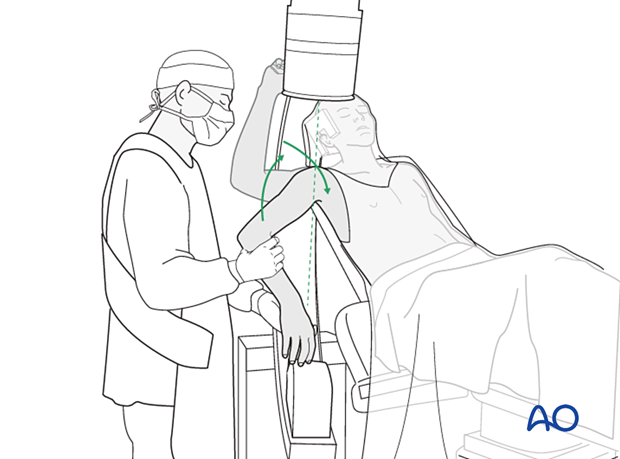
It is recommended that this procedure is performed with the patient in a beach chair position.
Patient positioning should be discussed with the anesthetist.

Approaches
The preferred option utilizes previous incisions for the shoulder replacement. The options include:
3. Reduction and preliminary fixation of the greater tuberosity
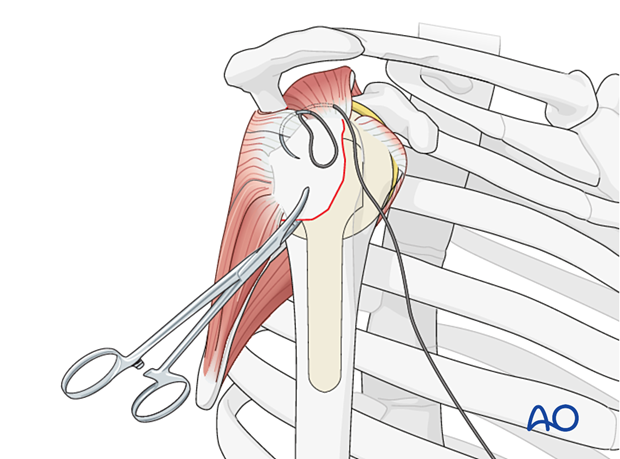
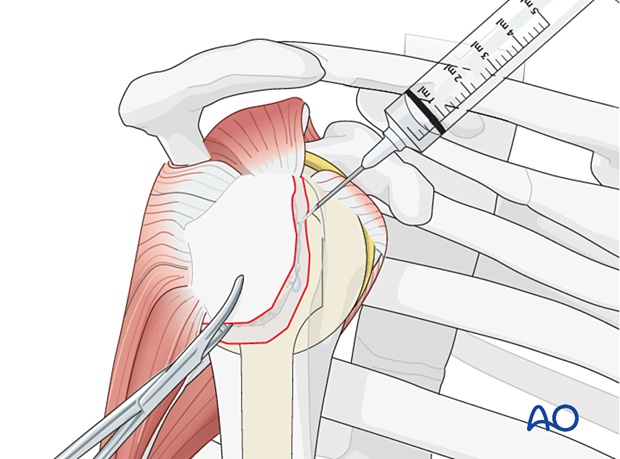
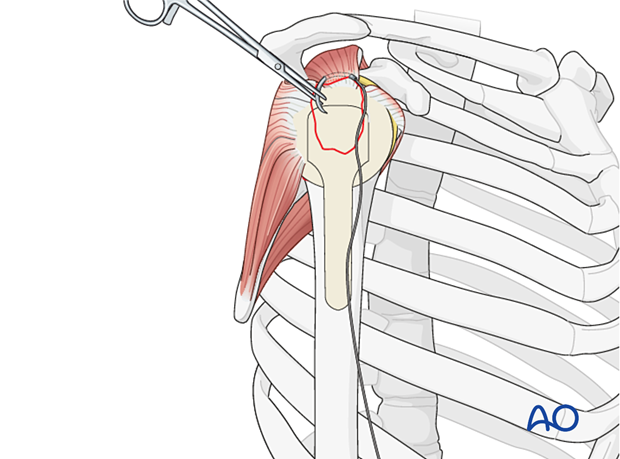
Stay sutures
Insert stay sutures through the supraspinatus and the infraspinatus tendon if necessary.
Cleaning the fracture bed
Irrigate the fracture bed and remove any hematoma. Prepare the margin of the fracture by removing or reflecting the periosteum, 2–3 mm back from the fracture line.
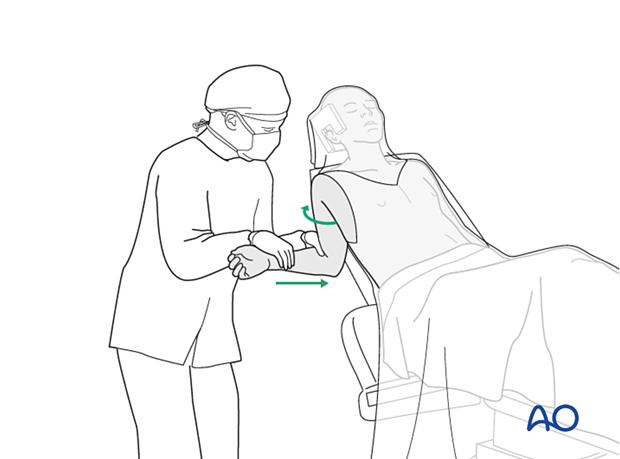
Reduction
Reduce the greater tuberosity by traction on the stay suture(s).
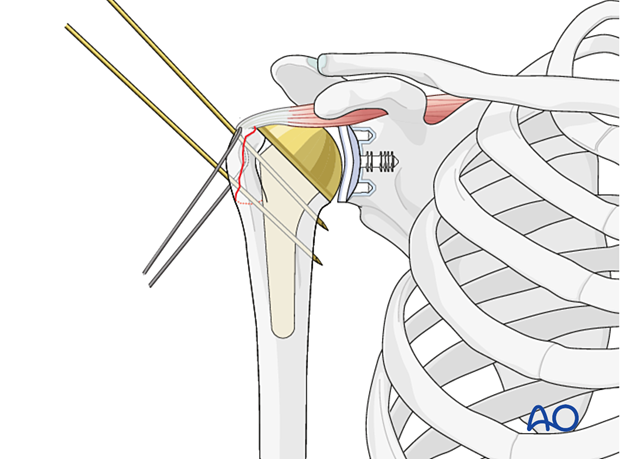
Preliminary fixation
An attempt can be made to temporarily secure the reduction with one or two K-wires. However, the presence of the humeral component may make this problematic. In such cases, manually holding the fragment in place may be necessary.
4. Fixation
General considerations
There are several techniques for fixing the greater tuberosity. The choice depends on the following:
- Size of the fragment
- Bone quality (osteoporosis)
- Degree of fragmentation
- Available bone stock
This is mainly indicated for a large, single fragment with good bone quality. Cannulated or standard screws can be used, with or without washers.
Sutures are more secure for patients with osteoporosis or comminution because they can be placed through tendon insertion sites, which may be stronger than the bone itself. The sutures can be placed in patterns that are optimal for stabilizing comminuted fragments.
Anchorage of sutures can be through an anterior to posterior drill hole through the lateral cortex of the humerus just distal to the fracture site, or through the subscapularis tendon anteriorly. Combinations of these techniques are possible.
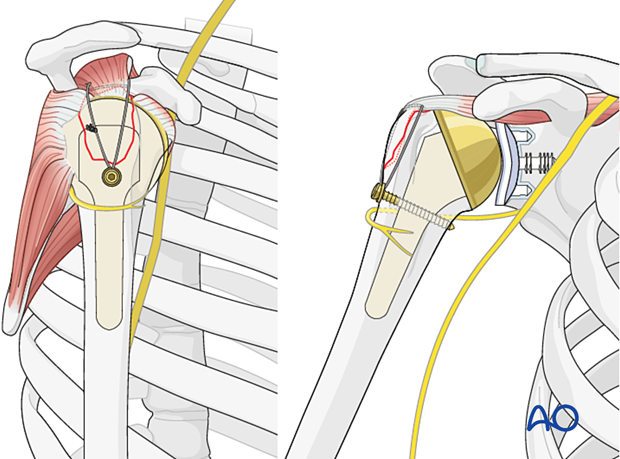
5. Screw fixation
Achieve preliminary fixation as shown above. Then insert at least two appropriately-sized screws to ensure rotational stability. Screws should engage the medial cortex, distal to the articular surface. Cannulated or standard screws may be used.
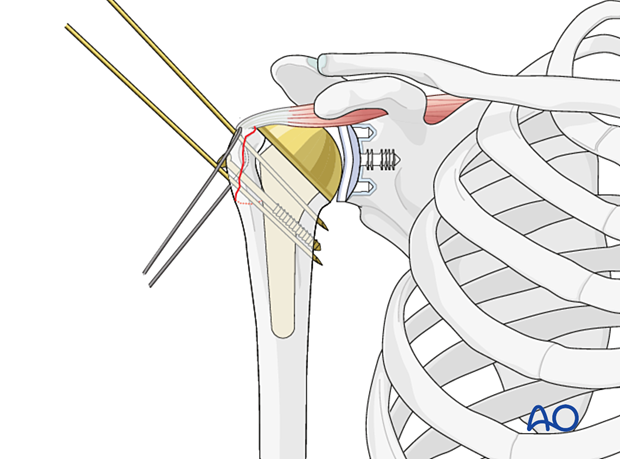
Check the fixation under image intensifier control.
Once the lag screw(s) are inserted, the K-wire(s) used for temporary fixation, and any stay sutures, should be removed.
6. Suture fixation
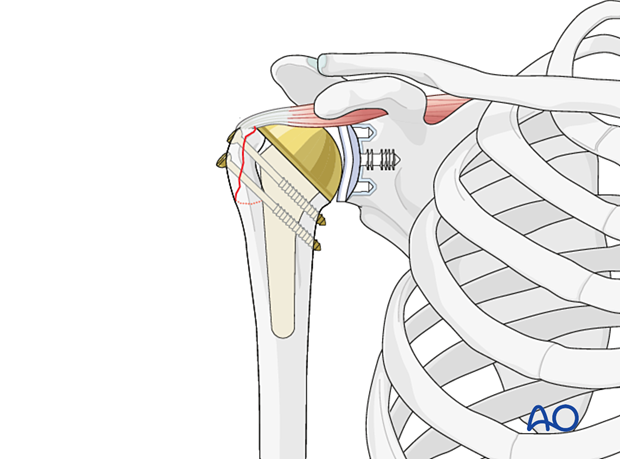
The most secure anchorage for a neutralizing suture is in the rotator cuff tendon, just before it inserts into the bone. Pass the needle parallel to the bone, picking up a good bite of the tendon. In osteoporotic patients, these sutures are more robust than when placed through the bone.
This form of fixation was referred to as a “Tension band suture fixation”. We now prefer the term “Neutralizing suture” because the tension band mechanism cannot be applied consistently to each component of the fracture fixation. An explanation of the limits of the Tension band mechanism/principle can be found here.
If there is sufficient bone stock around the stem, a screw can be used for distal anchorage.
Pass the suture through a washer and the washer over a cortex screw. The screw is then placed into the neck region.
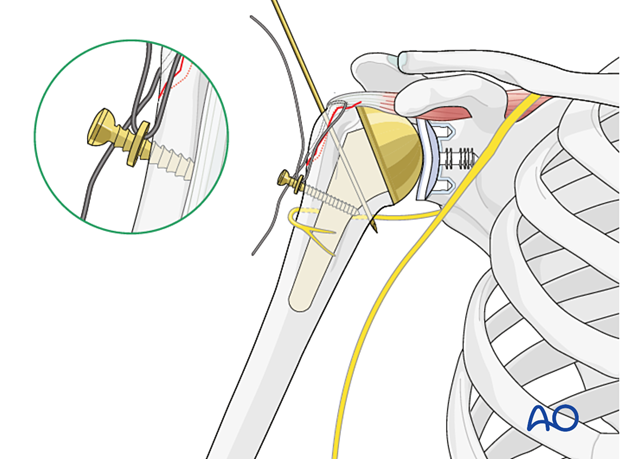
The suture is then tightened and tied.
Using a screw rather than a drill hole for anchoring has the advantage of requiring less exposure.
Alternative fixation options include:
- Transosseous cerclage or neutralization suture
- Transosseous self-centering suture
- Suture anchor
Combination of screw fixation and suture fixation
Screw osteosynthesis can be augmented using the beneficial effect of suture neutralization or cerclage suture techniques.
7. Final check of osteosynthesis
The C-arm must be directed to allow orthogonal views. Position the arm as necessary to confirm that reduction is satisfactory, fixation is stable, and the screws are of appropriate length.
8. Aftercare
Postoperative phases
The aftercare can be divided into four phases of healing:
- Inflammatory phase (week 1–3)
- Early repair phase (week 4–6)
- Late repair and early tissue remodeling phase (week 7–12)
- Remodeling and reintegration phase (week 13 onwards)
Full details on each phase can be found here.













