Antegrade nailing
1. Principles
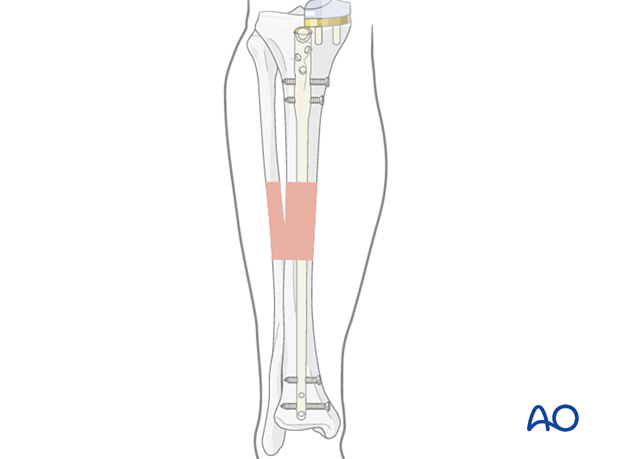
Intramedullary nailing
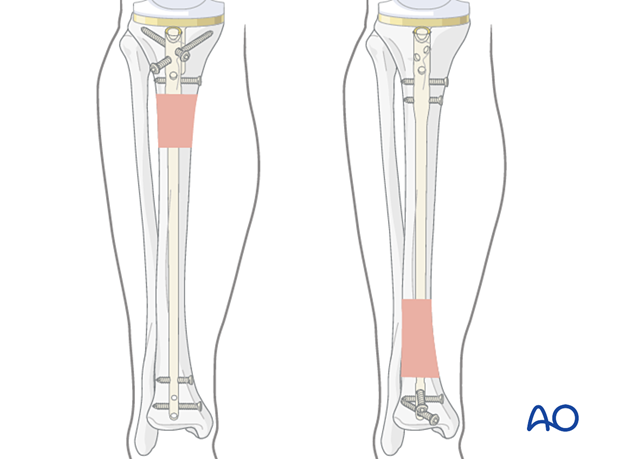
Access to the proximal tibia for intramedullary nail insertion is usually prevented by the tibial prosthesis.
If a patient has anatomy and tibia prosthesis positioning that is amenable to antegrade intramedullary nailing, this can be performed below the total knee replacement.
Intramedullary nailing is a good option in periprosthetic fractures with a unicompartmental knee replacement.
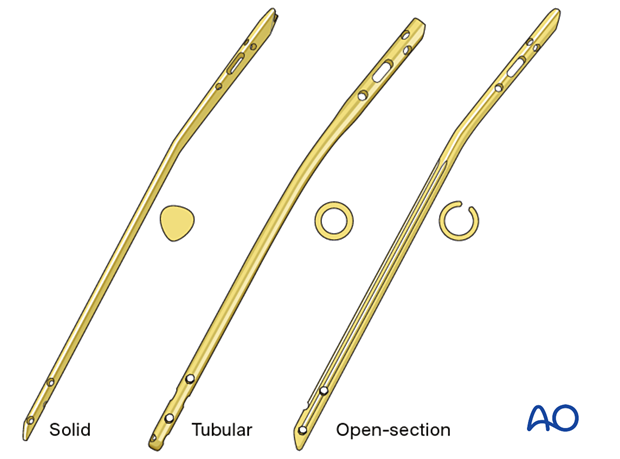
Implant selection
Tibial nails have interlocking screw options in multiple orientations, for better fixation in the proximal segment. It is important to consider the Herzog bend which must accommodate the anatomy and tibia prosthesis positioning.
Preoperative templating is performed to evaluate if an intramedullary nail can be placed safely.
2. Patient preparation and approach
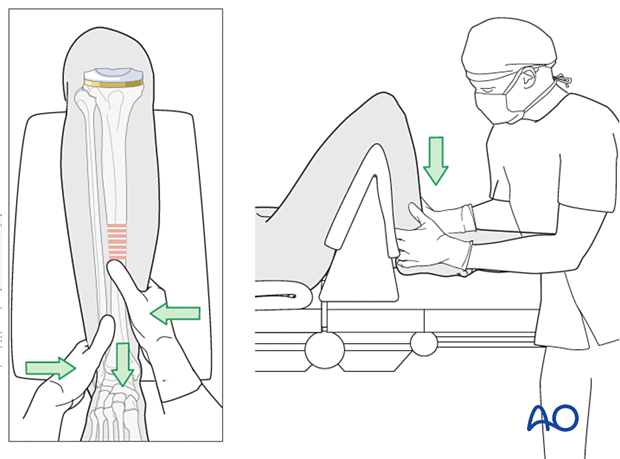
Supine positioning with a bump under the ipsilateral greater trochanter helps face the patella forward.
The knee is flexed over a radiolucent triangle or a ramp for nail insertion.
The midline approach to the knee that was used for the knee arthroplasty is used for nail insertion.
3. Indirect reduction
Manual traction
Depending on the patient’s positioning and type of OR table, one or two people may be required to perform manual traction.
The illustration shows a triangular radiolucent supporting frame, with padding over top, placed proximal to the popliteal fossa. It provides “countertraction” when the fracture is lengthened with distal traction.
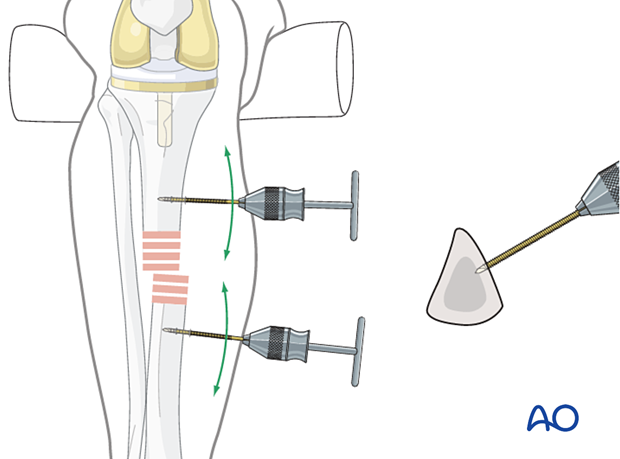
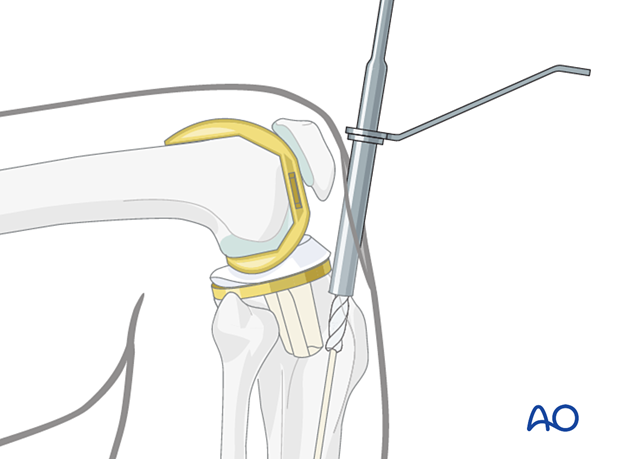
Joysticks
To aid reduction, a “joystick” (in this case a Schanz screw on a T-handled chuck) can be placed into either or both main tibial fragments.
Percutaneous reduction forceps
Oblique or spiral fractures can often be reduced with pointed reduction forceps applied percutaneously.
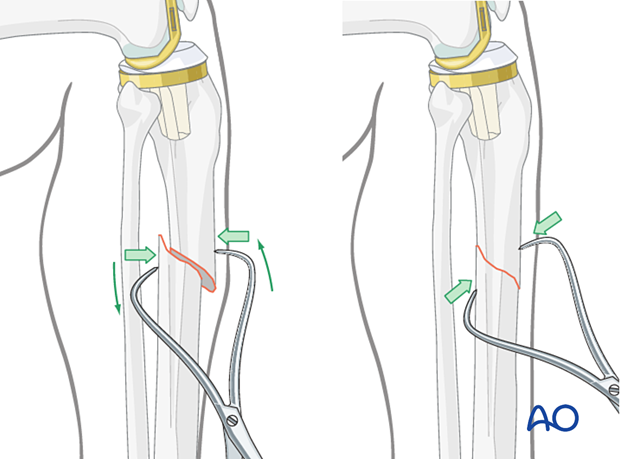
If the fracture is transverse, it may be reduced with manipulation using clamps on the bone ends.
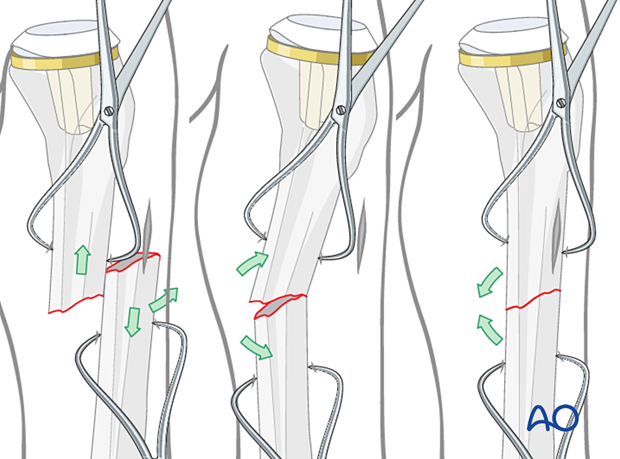
If the indirect reduction is inadequate, limited open reduction is needed. The surgeon must employ an atraumatic soft tissue technique to avoid complications.
Limited open reduction
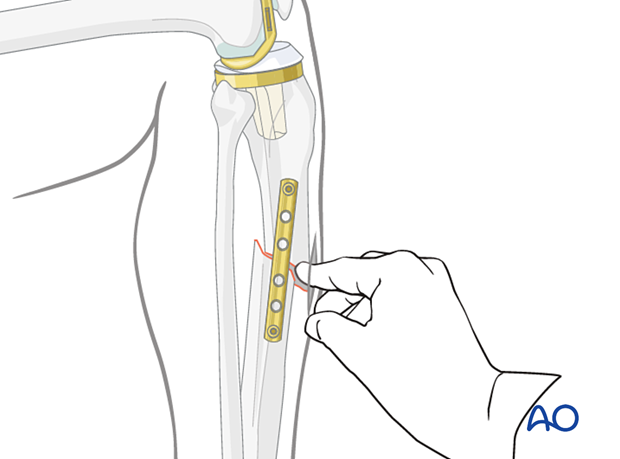
Temporary plate fixationAttaining an adequate reduction prior to instrumentation of the intramedullary canal is critical. A limited incision open reduction can safely be performed in conjunction with provisional reduction aids. Typically, a 1/3 tubular plate with unicortical screws will stabilize the fracture preliminarily.
A Hohmann retractor can be used for reduction by placing it between the fracture fragments and prying them apart.
4. Creation of the nail entry site
The incision must be made more distal than a typical infrapatellar tibial nailing. The dissection is carried down to the proximal tibia, clearly visualizing the tibial tray and carefully protecting the tibial tubercle.
The usual start point for a tibial nail is at the level of the tibial plateau in line with the intramedullary canal.
When a unicompartmental knee replacement is present the entry point might need to be moved slightly medial or lateral.
When a total knee is present, the start point moves 10 mm anterior and distal, between the tibial tray and the tibial tubercle.
The start point should be in line with the tibial crest, which can be palpated.
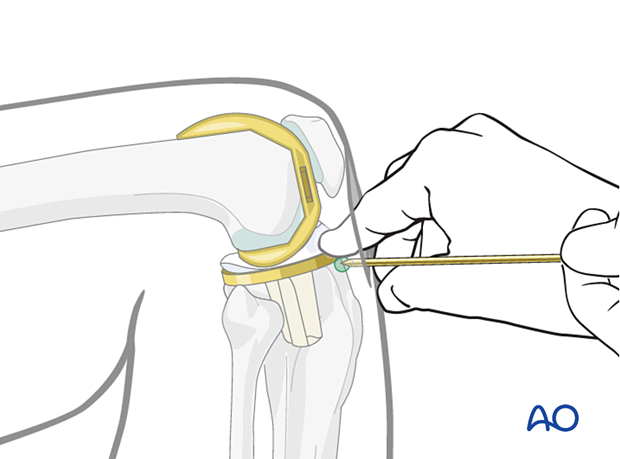
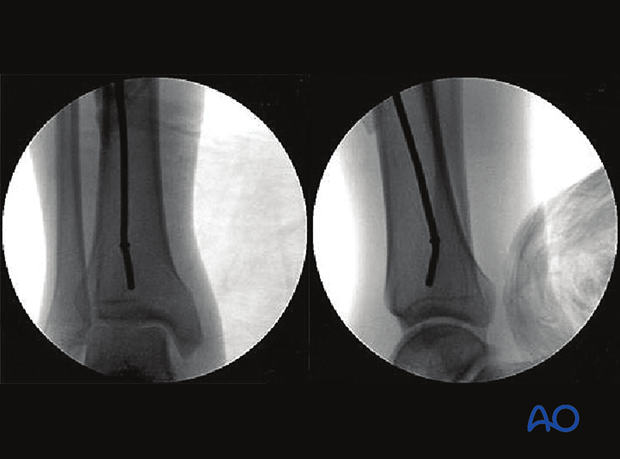
Insertion of the guide pin
Insert the guide wire aiming down the tibial crest, and thus the center of the medullary canal.
Opening the cortex
A cannulated awl or opening reamer is inserted over the previously placed guide pin. This should be performed under fluoroscopic control in the lateral projection, to avoid distal migration of the start point.
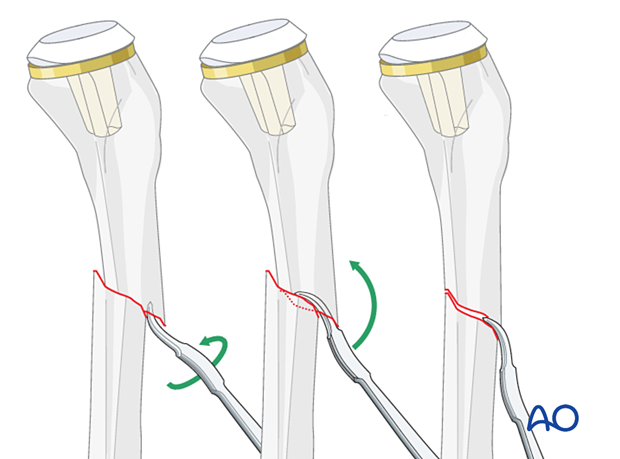
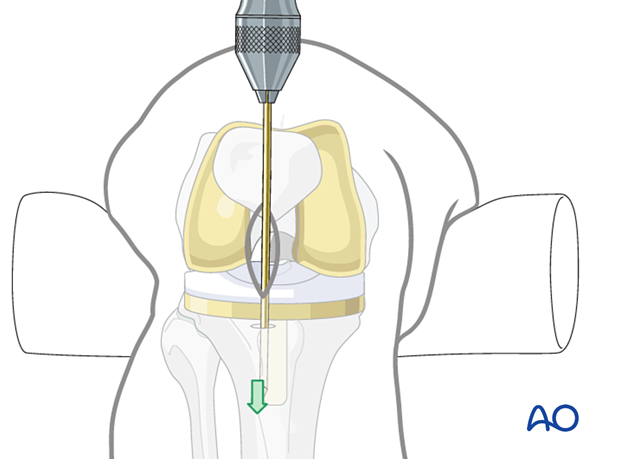
5. Guide wire insertion
Ball-tipped guide wire
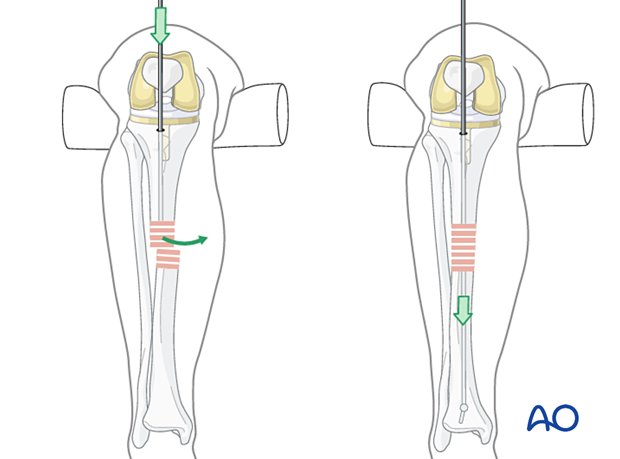
Once the proximal metaphysis is breached, pass a ball-tipped guide wire down the medullary canal into the distal metaphysis. This requires fracture reduction.
Bending the guide wire
Slightly bending the guide wire 10-15 mm above its tip is helpful for two reasons:
- Passing through the fracture site into the distal fragment is easier since rotation of the guide wire redirects its tip.
- It also facilitates the proper position of the tip in the distal metaphysis.
Fluoroscopic control
Use fluoroscopy to check that the guidewire is positioned above the center of the ankle joint.
Protect the tibial tray and the polyethylene during reaming. Proceed with caution as sequential reaming tends to cause distal migration of the entry point risking damage to the tibial tubercle.
Proceed according to the usual nailing technique.
6. Locking of the nail
Proximal locking
Aiming guides for proximal locking screws are used.
Proximal locking is dependent on the geometry of the prosthesis. The goal is to put a minimum of two interlocking screws.
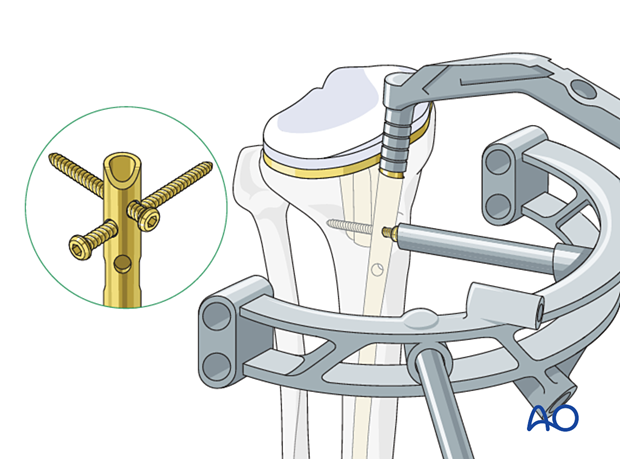
Distal locking
Distal locking is performed according to the standard nailing technique.
7. Aftercare
Intramedullary nailing usually allows early full weight-bearing postoperatively.
Knee bracing is not essential and should be considered optional for patient comfort.













