Proximal tibia replacement
1. Introduction
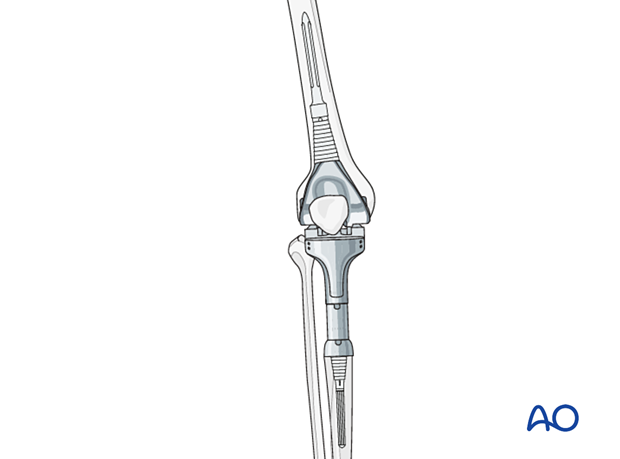
Proximal tibia replacement prosthesis is indicated when the tibial bone stock is insufficient or non-reconstructable.
The standard femoral component for primary total knee arthroplasty is not compatible with the proximal tibial replacement prosthesis. Therefore, the revision of the femoral component is required.
2. Preoperative planning
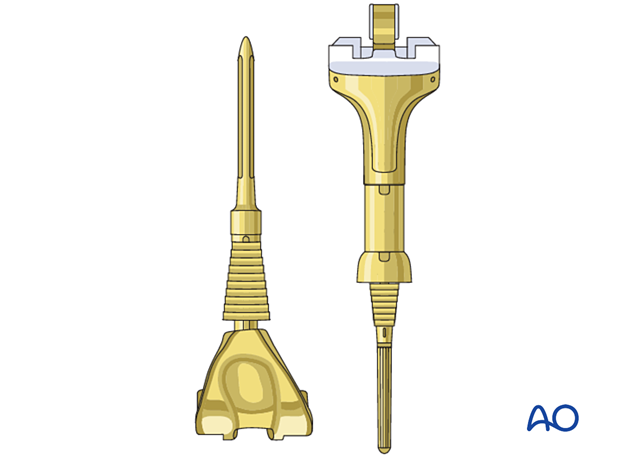
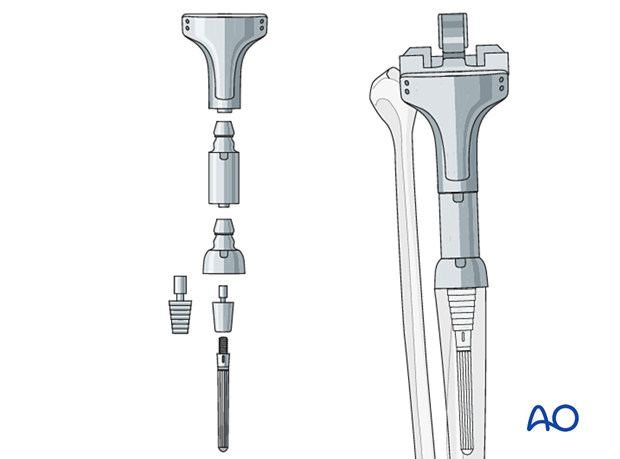
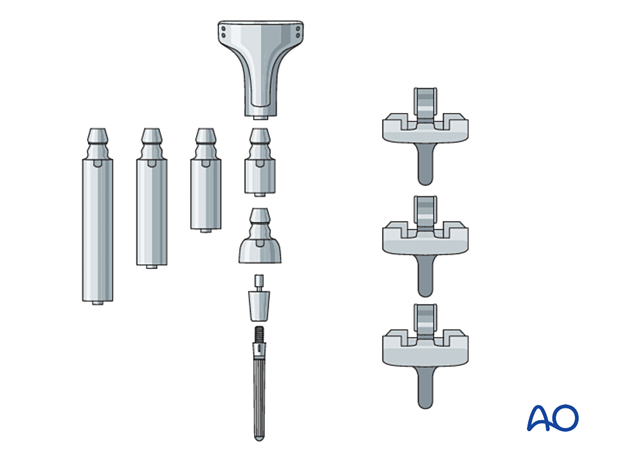
Proximal tibia replacement prosthesis
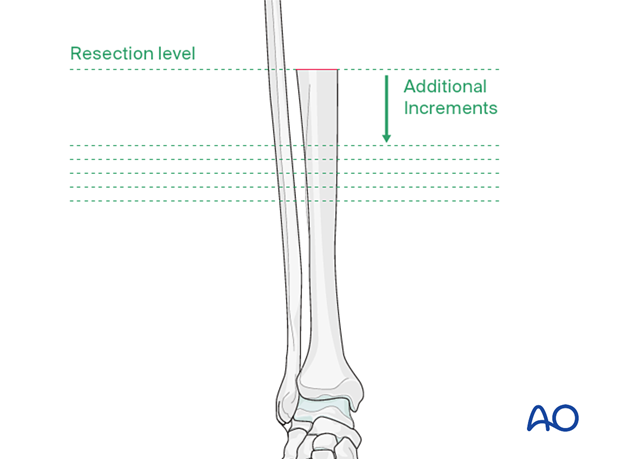
Templating is performed to determine the appropriate length of the proximal tibial bone resection.
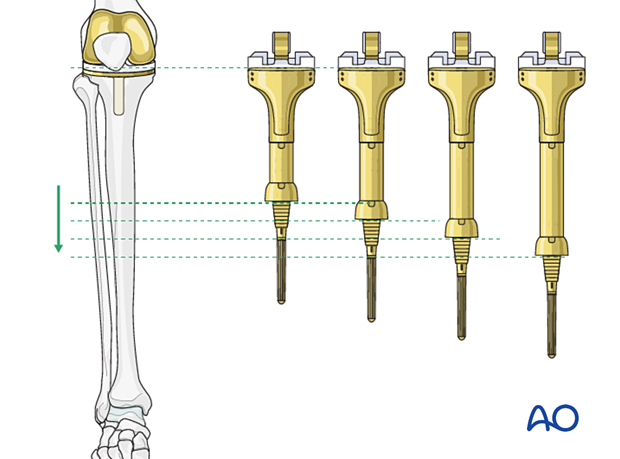
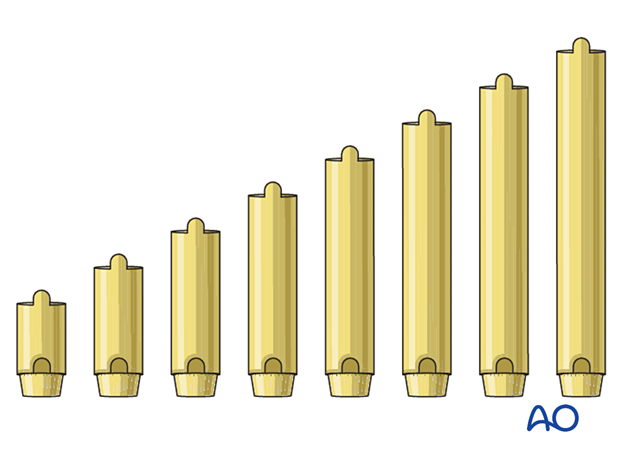
Additional intercalary segments are available to meet the reconstructive requirements.
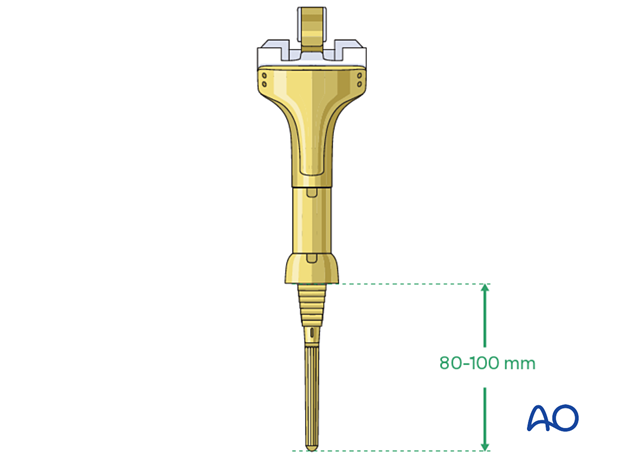
Tibial stem
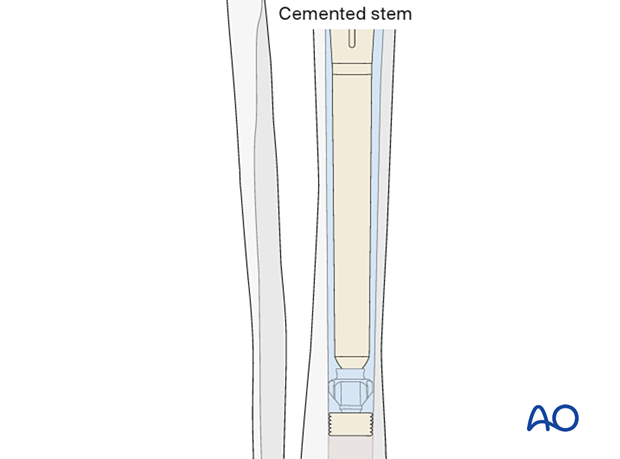
The length of the stem for the proximal tibia replacement prosthesis is typically 80-100 mm.
3. Patient preparation
The patient is placed in the supine position. A radiolucent table may facilitate intraoperative fluoroscopy if required.
4. Surgical approach
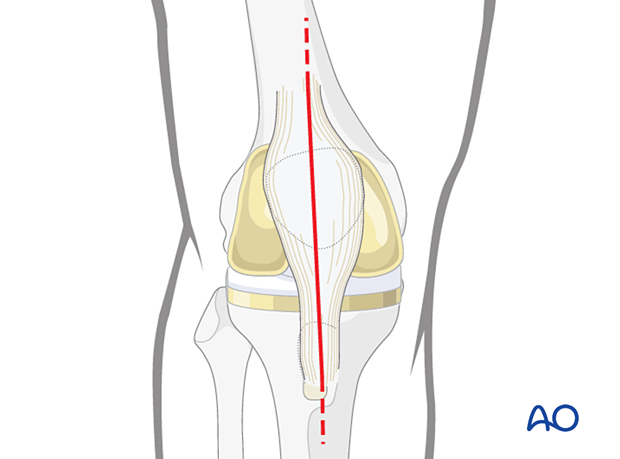
This procedure requires an adequate visualization of the knee joint. The most commonly used is a midline skin incision followed by a medial parapatellar arthrotomy. A proximal and distal extension may be necessary to achieve sufficient visualization and soft tissue releases.
5. Tibia
Tibial component removal
The tibial component is removed together with the fractured bone segments. Soft tissues and ligaments and the tibial tubercle with attached patella tendon are released from the proximal tibia fragment. The tibial tubercle is retained for later reconstruction of the extension mechanism. Care is taken to avoid neurovascular injuries.
Preparation of the tibia
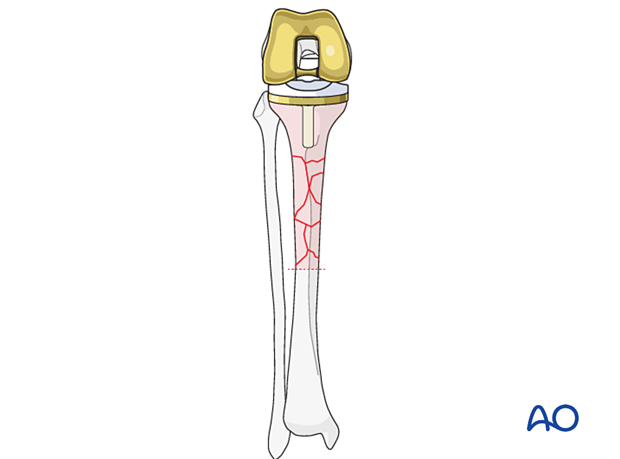
Additional bone resection in the tibia shaft may be necessary to accommodate the length of the proximal tibia replacement system.
The tibia resection level can be evened with a planer to optimize contact with the new prosthesis.
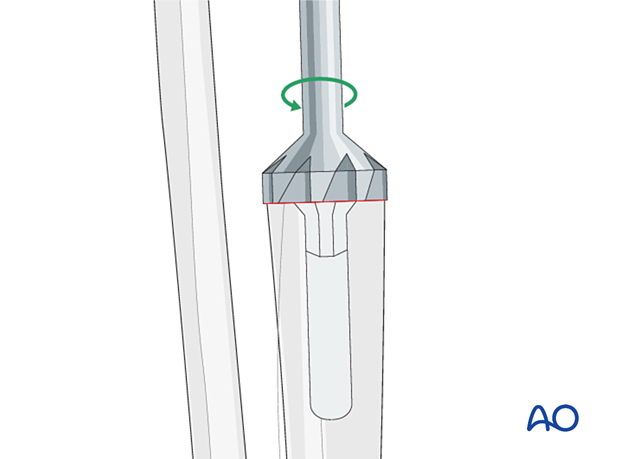
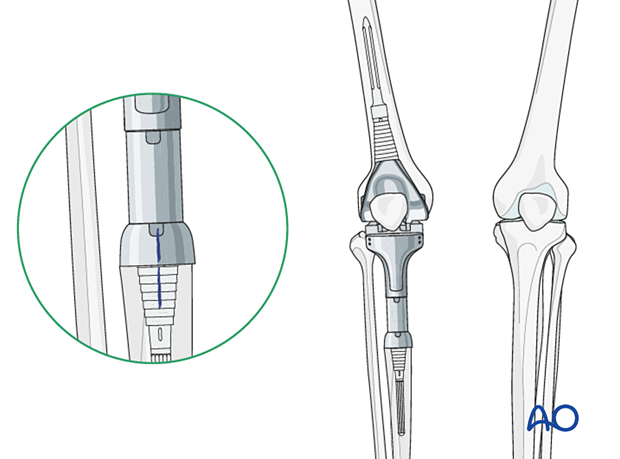
The tibial canal is prepared with reamers of increasing size. The depth of the reaming is determined by the length of the selected stem.
The diameter of the stem is determined by the reamer diameter which achieves cortical contact with the diaphyseal bone. One should allow for at least 2 mm of cement mantle around the stem.
6. Femur
Femur revision techniques are described under the treatment: complete femoral revision with hinged knee.
7. Trial
The trial components are assembled, and a trial reduction is performed.
Leg length
Leg length equalization is achieved by using the appropriate intercalary tibial segment(s) and with the selected thickness of the polyethylene bearing.
Rotational alignment
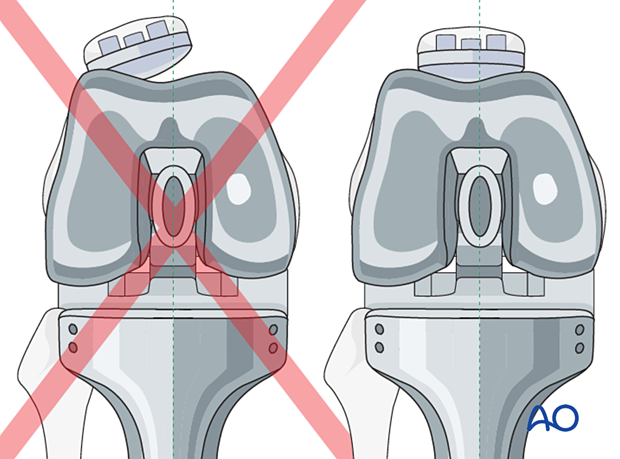
Rotational alignment of the components is critically important.
The tibial component is aligned with the femoral component and is checked using anatomical landmarks including the tibial crest and the intermalleolar axis.
Proper rotational alignment of the femoral component is referenced to:
- Linea aspera
- Fluoroscopic rotational assessment using the lesser trochanter
- Patellar tracking during trial reduction
Marking of the proper rotational alignment is performed for later reference during component insertion.
Patella tracking
Patella tracking is carefully assessed to ensure no instability or impingement throughout the entire range of knee motion.
8. Components insertion
Bone preparation for cementing
The tibial canal is lavaged and dried.
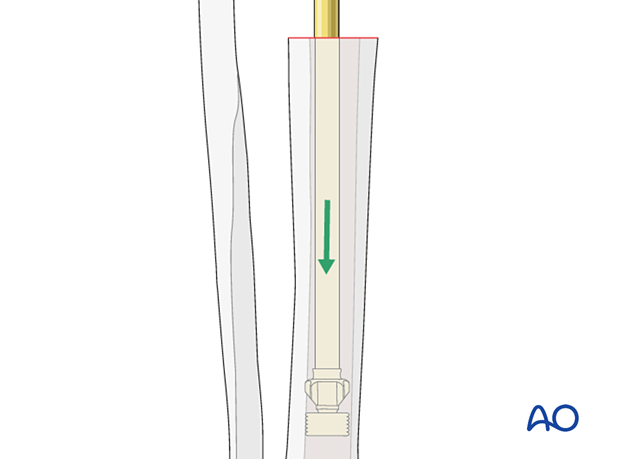
Cement restrictor
The cement restrictor is inserted into the tibial canal to allow for a 1 cm cement mantle between the stem tip and the restrictor.
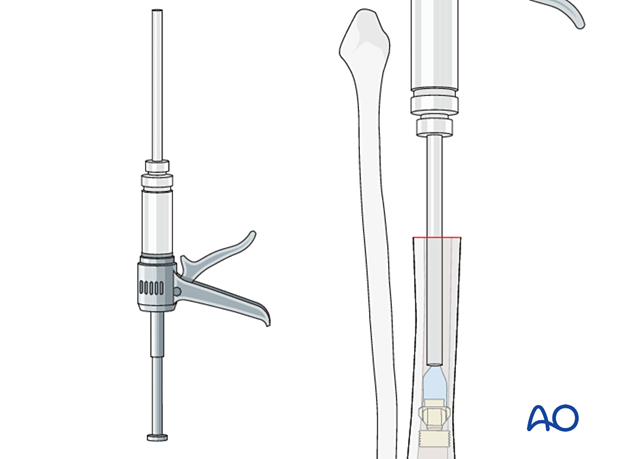
Cementing
Cement is mixed using standard techniques and is injected into the canal with retrograde filling and pressurization, using a cement gun.
Tibial component
The tibial component is seated with rotational alignment to previously made marking during the trial reduction.
Coupling
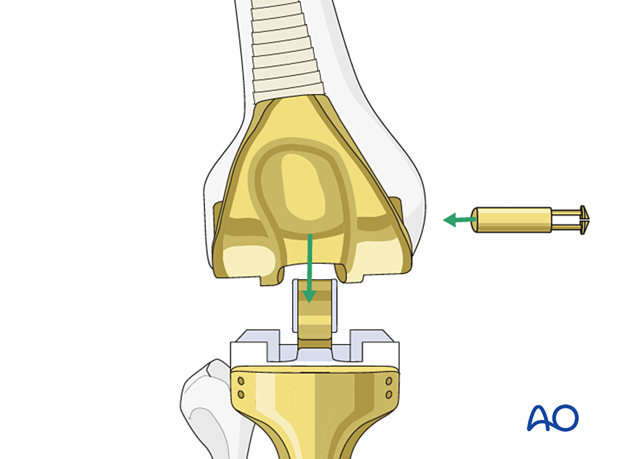
The selected polyethylene bearing along with the bushings for hinged articulation are assembled and coupled together.
If patellar tracking is not ideal, a lateral retinacular release and medial imbrication can be performed.

9. Extensor mechanism reconstruction
Most of the proximal tibial replacement prostheses allow for suture reattachment of the remaining patellar tendon with its attached bone fragment. Some may also offer clips or pins to add additional fixation.
10. Aftercare
The patient is allowed to bear full weight.
The patient should be protected in extension with a knee brace for 6 to 8 weeks to allow for sufficient healing of the extensor mechanism.
A gentle range of motion can then be started.
The anterior compartment muscles are often compromised from the surgical dissection, the use of an ankle foot orthosis (AFO) to support the foot and ankle during gait is recommended













