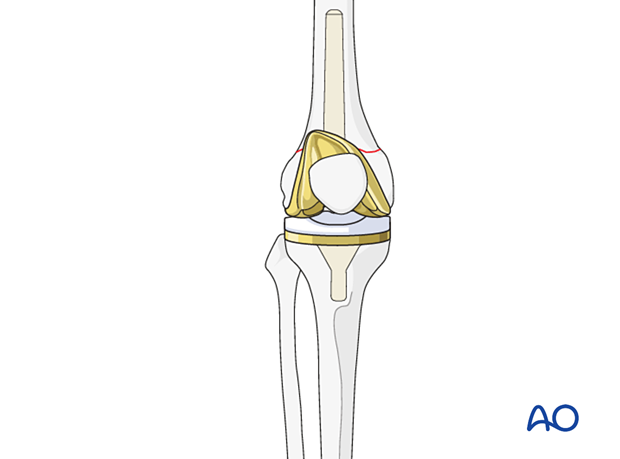
Complete femoral revision with varus/valgus CCK system
1. Introduction
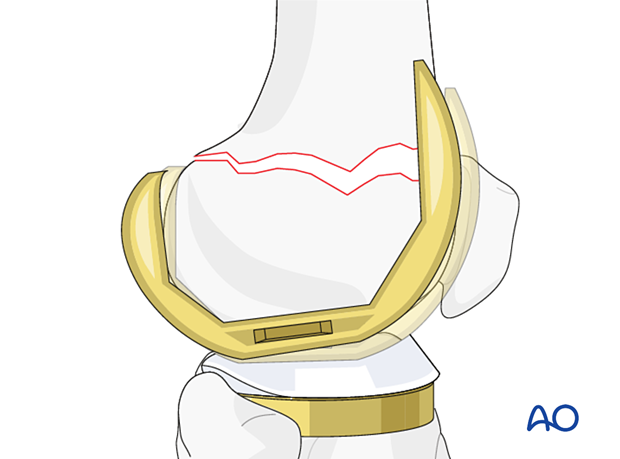
Isolated femoral revision without tibial revision is performed when the femoral component is unstable, or the fracture is not reconstructible. The tibial component is stable and properly aligned. It is important to select an appropriate femoral revision system that is compatible with the retained tibial component.
Femoral revision requires sufficient bone stock and functional collateral ligament integrity. If the collateral ligaments are absent, or incompetent, a hinged prosthesis is required. The hinged knee prosthesis is associated with a higher rate of failure, in particular in the younger and more active patients. Retention of the collateral ligaments origin allows for isolated femoral revision with a stemmed component.
This section focuses on the principles of revision total knee arthroplasty using a medial-lateral constrained implant system or a constrained condylar knee (CCK) system.
The tibial component should be examined for fixation stability and proper alignment during surgery and addressed if necessary.
In selected cases, a less constrained articulation and femoral component can be used for the femoral revision.
2. Preoperative planning
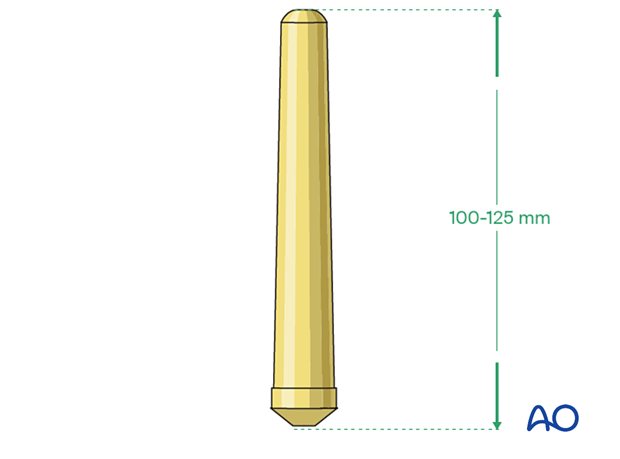
Femoral stem
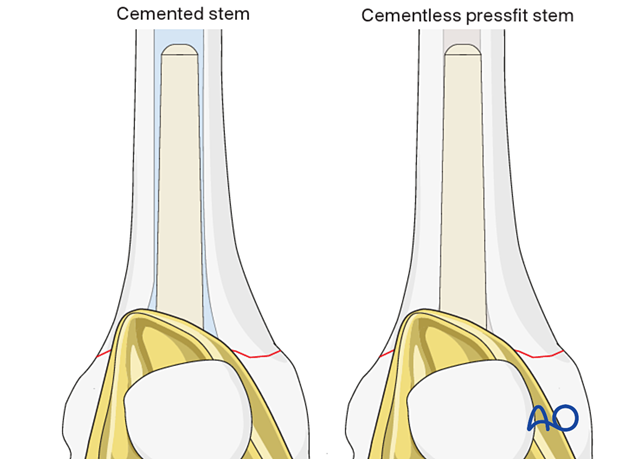
A stem for the femoral component is often required. The stem length is generally 100 - 125 mm. Both a cemented and cementless stem can be used.
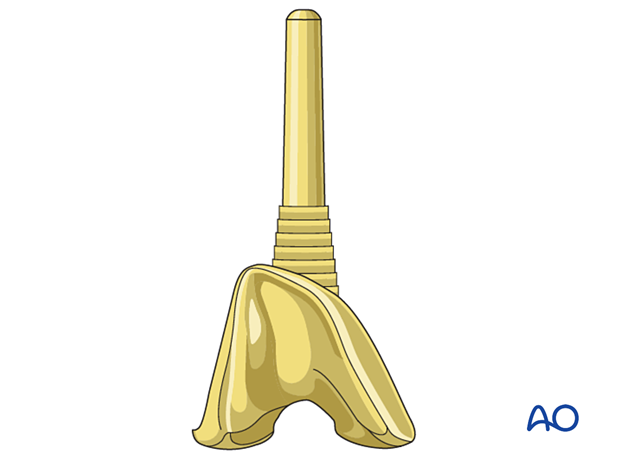
Supplemental metaphyseal fixation
The surgeon may consider using supplemental metaphyseal fixation with cone or sleeve.
Different surgical techniques are involved with the use of a sleeve or a cone.
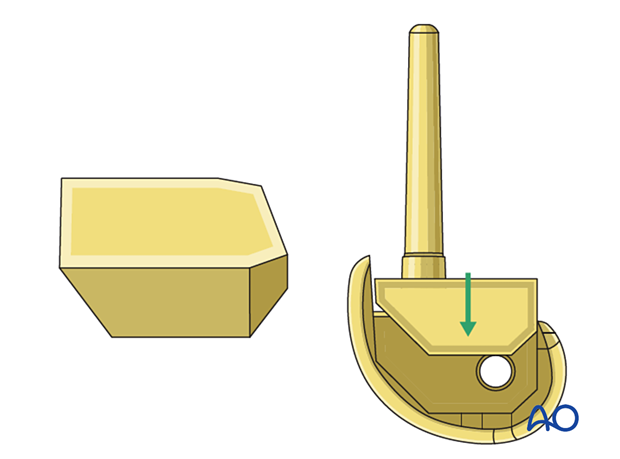
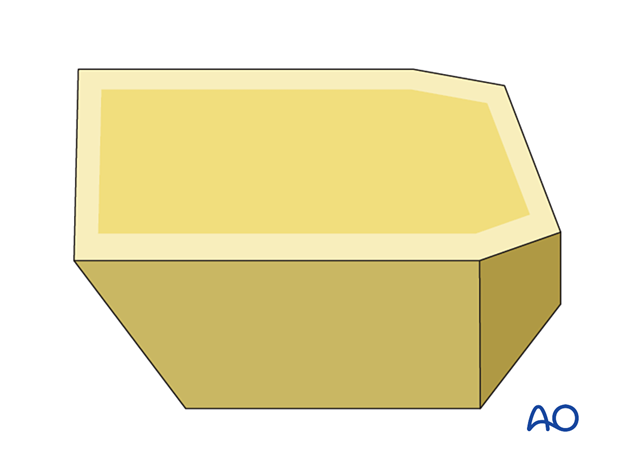
Compensation for bone loss
The surgeon should have metallic augments and wedges available to compensate for any significant bone loss in the distal femur.
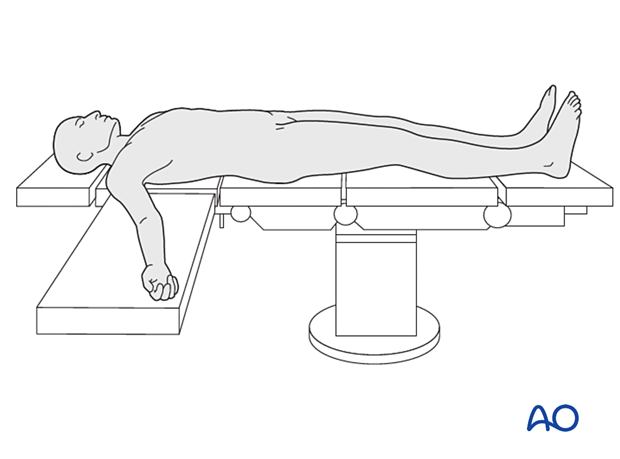
3. Patient preparation
The patient is placed in the supine position. A radiolucent table may facilitate intraoperative fluoroscopy if required.
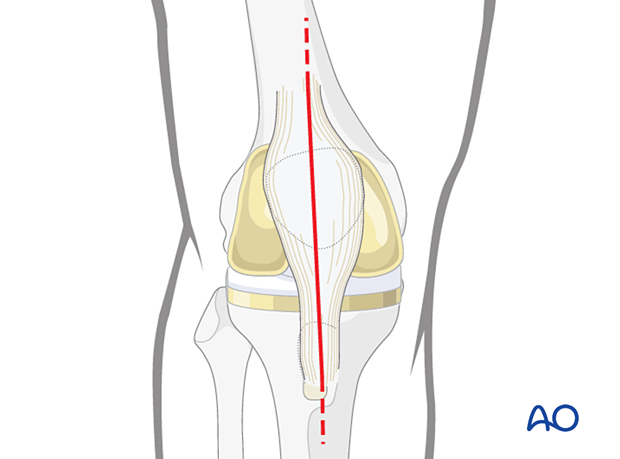
4. Surgical approach
This procedure requires an adequate visualization of the knee joint. The most commonly used is a midline skin incision followed by a medial parapatellar arthrotomy. A proximal and distal extension may be necessary to achieve sufficient visualization and soft tissue releases.
5. Femur
Removal of the femoral component
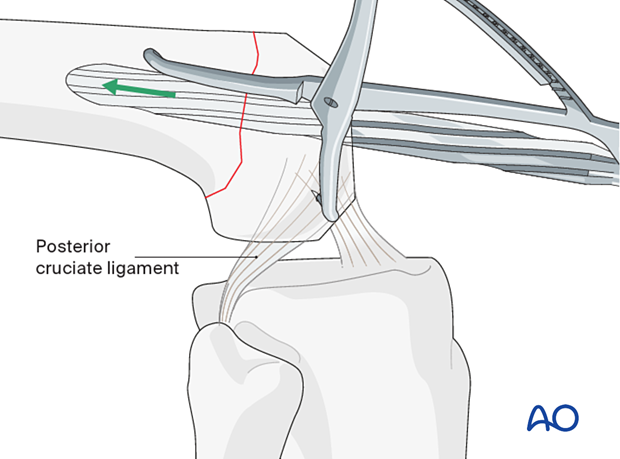
The femoral component is removed, using small oscillating saw and cement osteotomes.
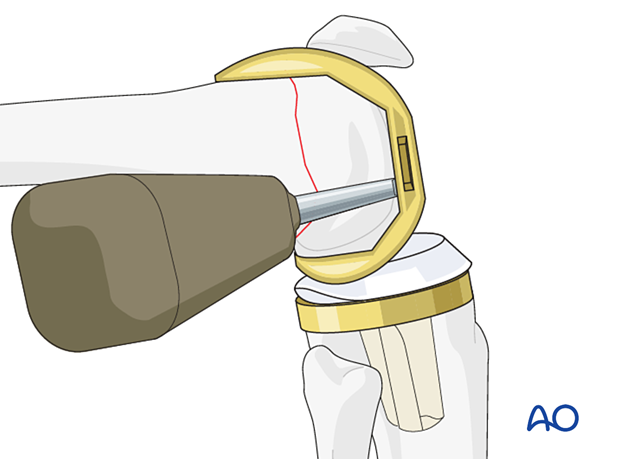
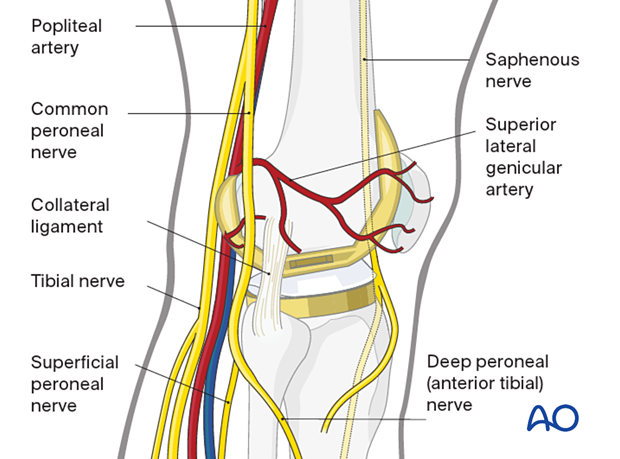
It is important to maintain the attachment of the collateral ligaments and the bony fragments of the femoral condyles.
Care must be undertaken to avoid injury to the neurovascular structures, and to the extensor mechanism of the knee.
Femoral preparation
Provisional stabilization of the fracture fragments will facilitate the femoral preparation.
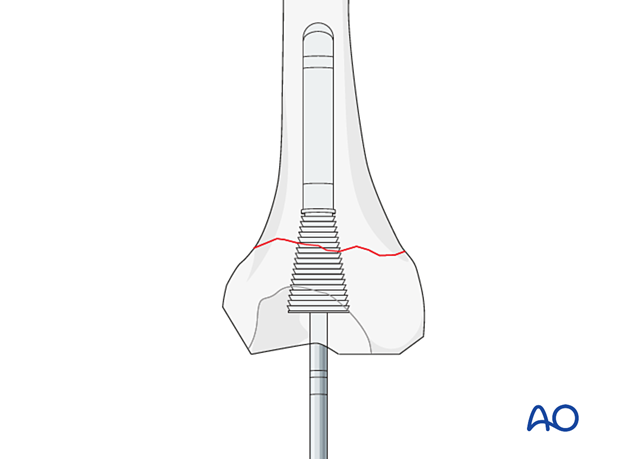
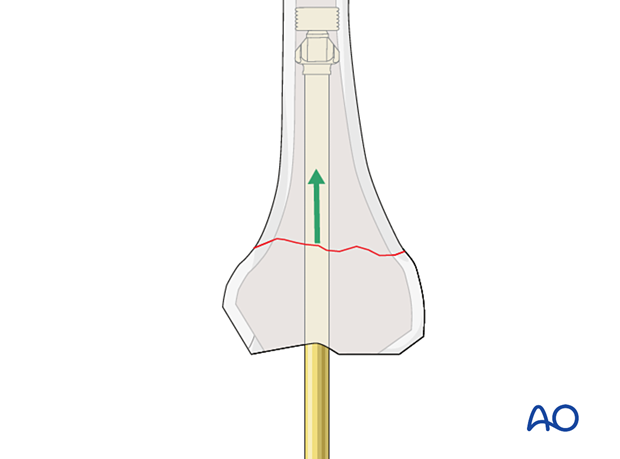
The femoral canal is prepared with reamers of increasing size. The depth of the reaming is determined by the length of the selected stem.
If additional bone cuts are needed, then an intramedullary femoral cutting jig is used to make the appropriate bone cuts for the constrained femoral prosthesis.
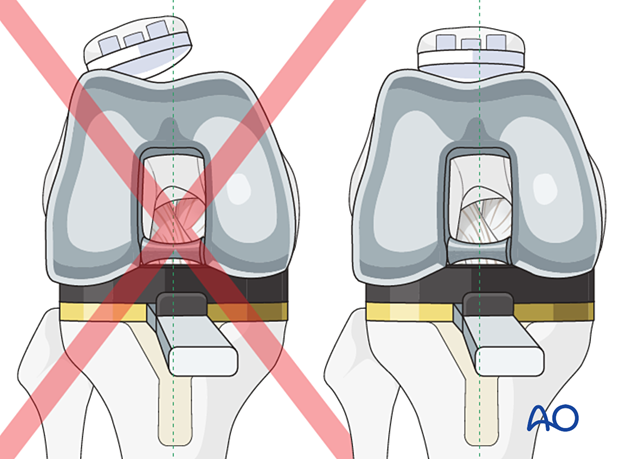
Take care to rotate the cutting block in line with the transepicondylar axis and parallel to the tibial tray in order to achieve a symmetrical flexion gap.
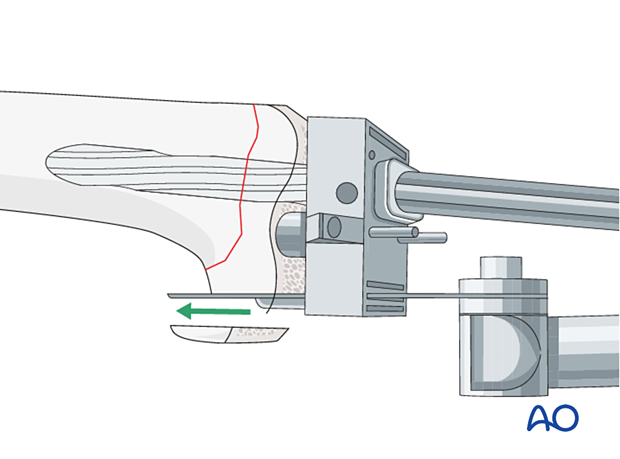
The diameter of the stem is determined by the reamer diameter which achieves cortical contact with the diaphyseal bone. One should allow for at least 2 mm of cement mantle around the stem if cement fixation is used.
If cementless stem fixation is selected, line to line fit of the reamer to the final stem diameter is used.
If there is bone deficiency due to fracture fragmentation, additional bone cuts may be required to remove the fragments and to accommodate the use of augments behind the new femoral component to achieve the balanced extension and flexion gaps.
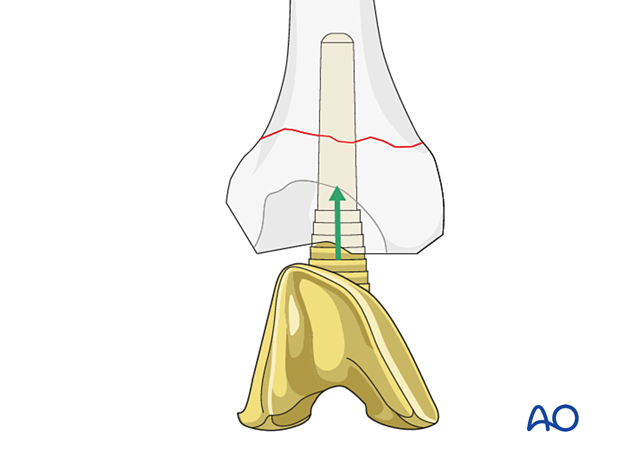
If a femoral sleeve or a cone is selected, appropriate instruments are used to prepare the distal femur.
6. Trial
The trial component is assembled, and a trial reduction is performed.
Gap balancing and knee stability assessment is performed using the appropriate thickness of the trial polyethylene insert. The goal is to achieve symmetrical flexion and extension gaps. This is performed using tension spreaders or gap sizing blocks.
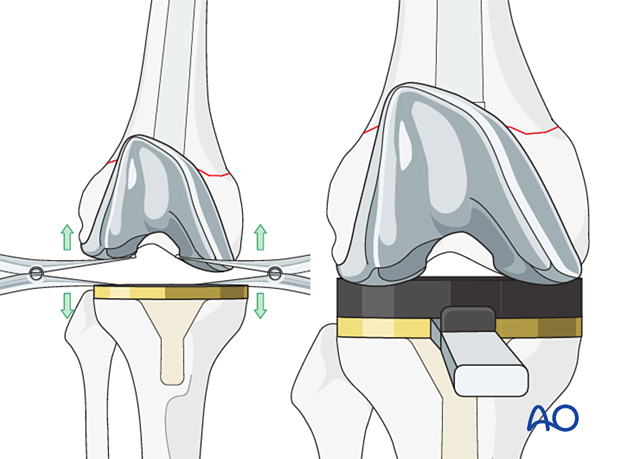
Patella tracking is carefully assessed to ensure no instability or impingement throughout the entire range of knee motion.
7. Components insertion
Bone preparation for cementing
The femoral bone surface and the canal are lavaged to remove any debris. The bone surface and the canal are dried before proceeding.
Cement restrictors
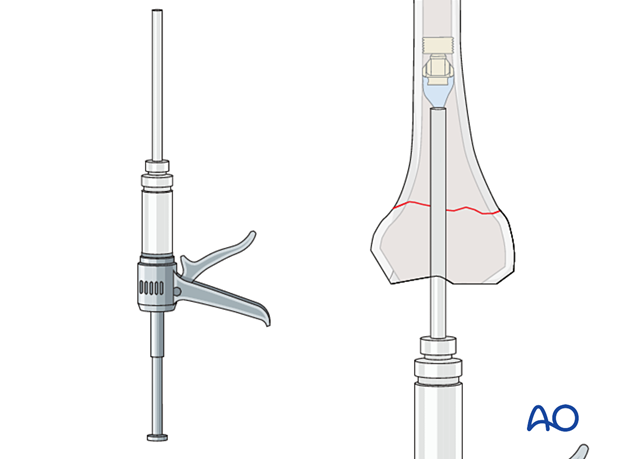
The cement restrictor is inserted into the femoral canal to allow for a 1 cm cement mantle between the stem tip and the restrictor.
If a sleeve is used, the sleeve and the stemmed femoral component are assembled together first, then the monobloc implant is inserted into the femur.
Cementation
Cement is mixed using standard techniques and is injected into the canal with retrograde filling and pressurization, using a cement gun.
Insertion of the femoral component
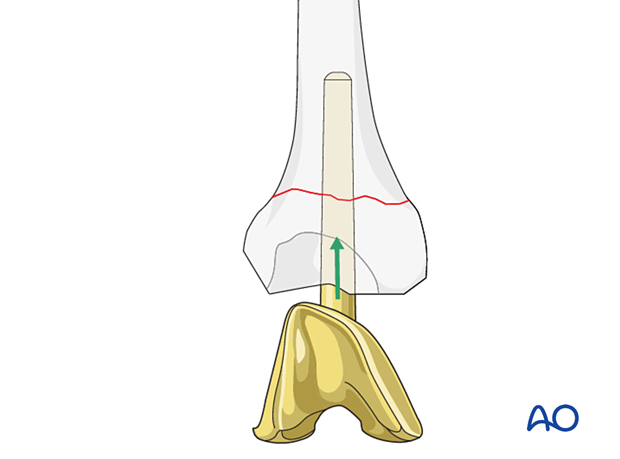
The femoral component (including any augment) is seated with 3-5° of external rotation to the mid coronal axis of the femoral shaft or in line with the trans-epicondylar axis to allow for proper patellar tracking. The femoral rotation is also aligned to the tibial component to achieve a symmetrical flexion gap.
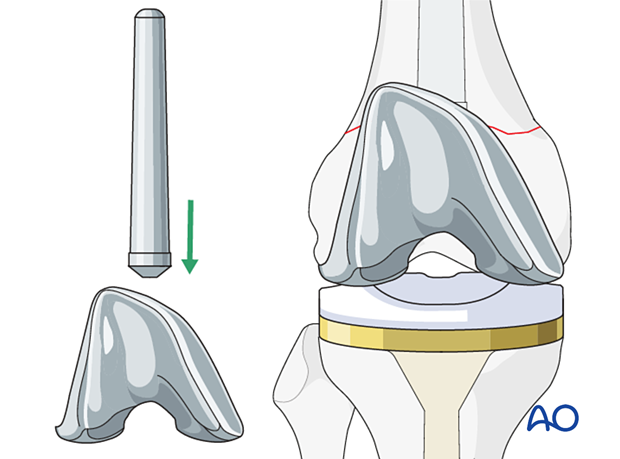
8. Final reduction
The selected polyethylene bearing component is impacted into the retained tibial tray. Additional locking screw or pin for the polyethylene bearing is inserted according to the requirements of each implant design.
If patellar tracking is not ideal, a lateral retinacular release and medial imbrication can be performed.

9. Aftercare
The patient can be mobilized with full weight-bearing and active range of motion immediately after surgery.













