Suture repair
1. Introduction
Often periprosthetic patellar fractures might be isolated superior pole or inferior pole avulsion fractures. These typically have stable patellar buttons but lack an intact extensor mechanism.
It is critical to reconstruct the extensor mechanism and the modified Krakow suture technique with bone tunnels through the remnant patella can be effective.
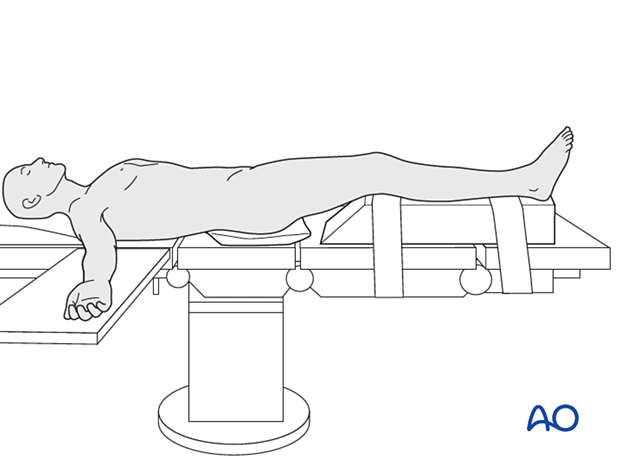
2. Patient preparation and approach
The patient should be positioned supine with the affected lower extremity on a ramp that will allow for full knee extension and ease of biplanar fluoroscopy.
The prior surgical incision should be utilized over the mid patella. The deep dissection should be carried out with an arthrotomy that will allow for exposure of the undersurface of the patella. Utilization of a proximal thigh tourniquet can be helpful during reconstruction. The surgeon may also choose to have appropriate polyethylene implants available for revision, particularly in knee replacements that have been in place for many years.
3. Reduction and fixation
The avulsed bony fragment attached to the quadriceps or patellar tendon can be used to facilitate reduction. However, more commonly the suture will first be placed within the tendon to facilitate reduction.
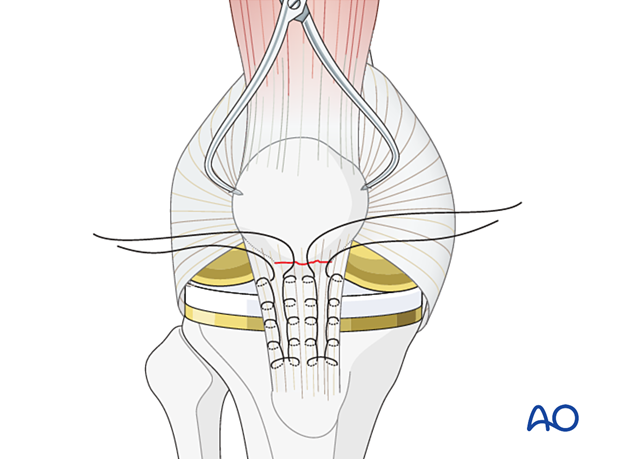
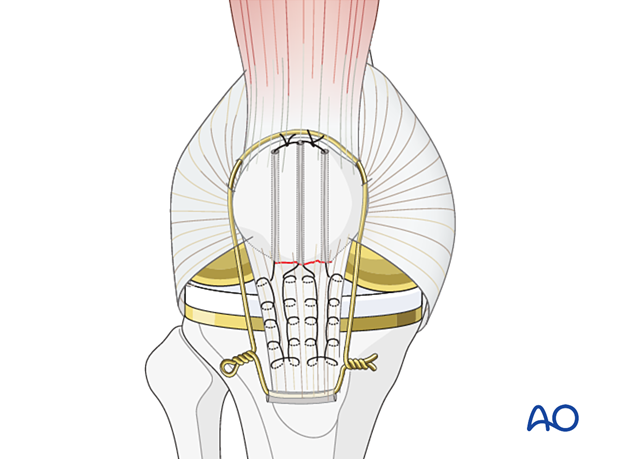
Krackow whip stitch
The Krackow whip stitch uses 2 or more locking loops inserted into each side of the patellar (or quadriceps) tendon. The Krackow whip stitch is stronger than the Kessler, or Bunnell, stitches that are used for repairing smaller tendons.
The suturing configuration can vary depending on the surgeon's preference.
Open the patellar tendon retinaculum longitudinally. Insert two locked Krackow stitches of #5 non-absorbable suture into the patellar tendon, as illustrated.
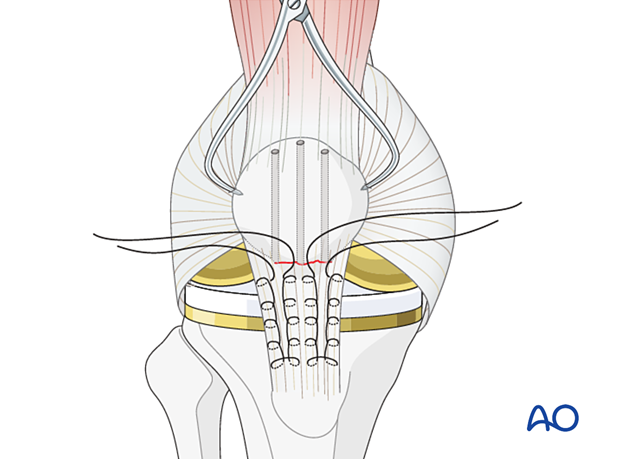
Make holes in the main fragment
Make 3 longitudinal drill holes with a 2.5 mm drill in the proximal patellar fragment. Be careful to ensure that there is adequate space between the holes to ensure a stable base for the sutures.
The inferior or superior pole of the patella should be prepared with a curette to a bleeding bony base to maximize healing potential.
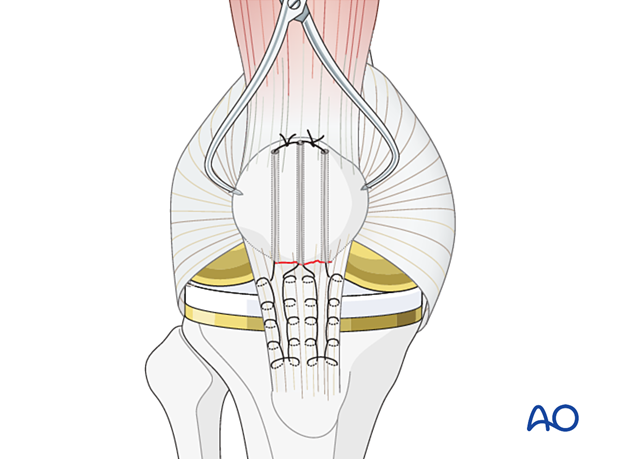
Ligament fixation
Using a suture passer from proximal to distal, pull the free ends of the sutures through the proximal segment.
The sutures are then tightened and tied deep to the opposing tendon, with the knee in full extension. It can be helpful to place a pointed bone tenaculum on the intact patella and utilize it to draw the patella towards the ruptured tendon. This will decrease the risk of suture failure.
Be sure that there is good contact between the tendon and the bone.
Augmentation of patella tendon repair
To protect this suture repair during the healing process, a protective cerclage wire or suture can be passed around the upper pole of the patella and through a transverse drill hole distal to the tibial tubercle.
This wire frequently breaks later, and it is best to remove it once healing is assured at 3-4 months.
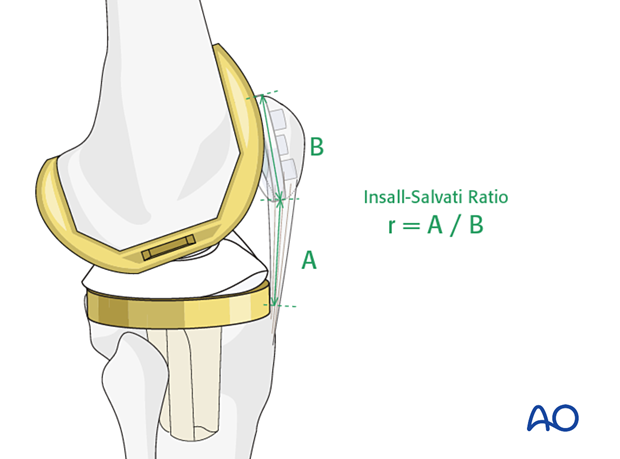
If the cerclage wire is tightened too tightly it will not be possible to flex the knee and a patella baja will occur.
This complication must be avoided and can cause severe limitation of knee flexion. If there is a need for a cerclage wire to protect the patellar tendon, a patella baja can be produced by misjudging the exact length of the patellar tendon. The opposite knee will indicate the correct position of the patella as described under x-ray evaluation.
The Insall-Salvati Ratio can be used as a surrogate measurement for patella baja. The ratio of the length of the patellar tendon measured on the lateral projection to the length of the patella should be 0.8 - 1.2.
4. Aftercare
Tendon healing often progresses slower than fracture healing. Rehabilitation should progress accordingly. Gentle knee flexion can start after wound healing. Active and resisted knee extension should be limited until 10 weeks.













