Anterior column screw fixation
1. Principles
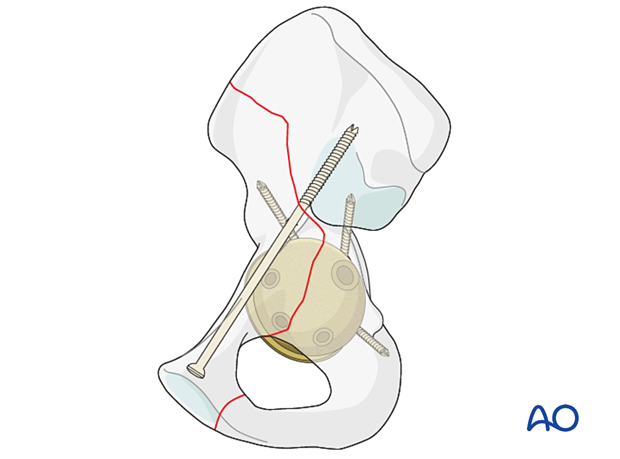
Fracture morphology and surgeon's experience will dictate the choice of fixation method to achieve fracture stability and maintain cup stability.
Intraoperative fractures occurring during component removal or after the arthroplasty surgery, are typically associated with chronic problems related to total hip replacement. In the setting of infection, loosening, or osteolysis the cup may need to be removed.
For further information about standard techniques for ORIF in native acetabular fractures, please refer to the acetabulum section of the AO Surgery Reference.
2. Implant selection
Column screw fixation is typically performed with non-cannulated screws when the fracture is reduced openly as the starting point is easily visualized.
Percutaneous methods are often aided using cannulated screw fixation. Ideally, screws with an outer diameter over 6.5 mm will provide the most rigid guide pin and prevent guide pin complication.
The column corridors must allow for screws of this caliber.
3. Reduction
Anterior column fractures can be more challenging to address and typically do not need to be surgically addressed if there is an intact posterior column. However, in the setting of an unstable cup, with fracture or to prevent late instability, the anterior aspects of the joint should be reduced and stabilized.
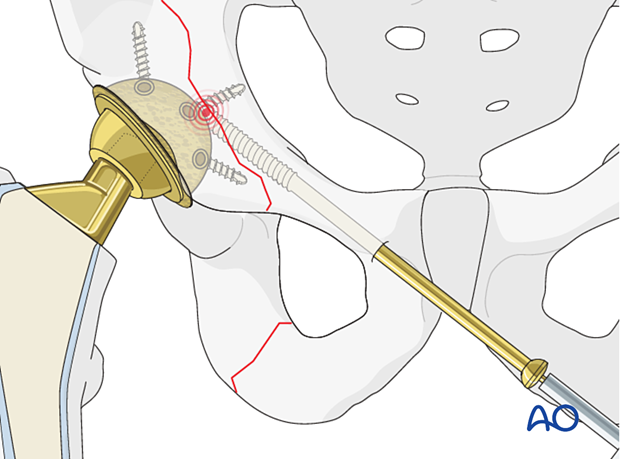
4. Screw application in antegrade fashion
The anterior column can be addressed through an open exposure or through a percutaneous approach.
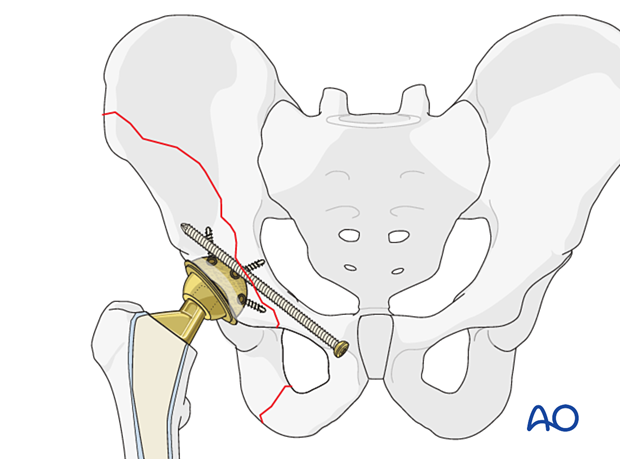
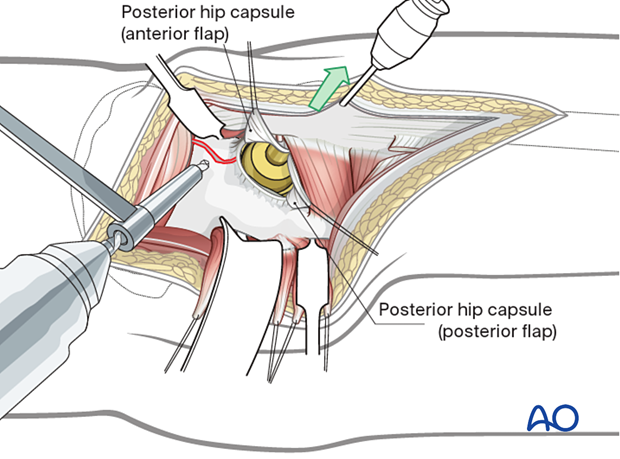
Exposure through open posterior approach
The posterior approach to the hip, with the patient in a lateral position, can easily be extended to expose the screw entry point on the proximal ileum. The screw can be inserted across the fracture site into the low anterior column.
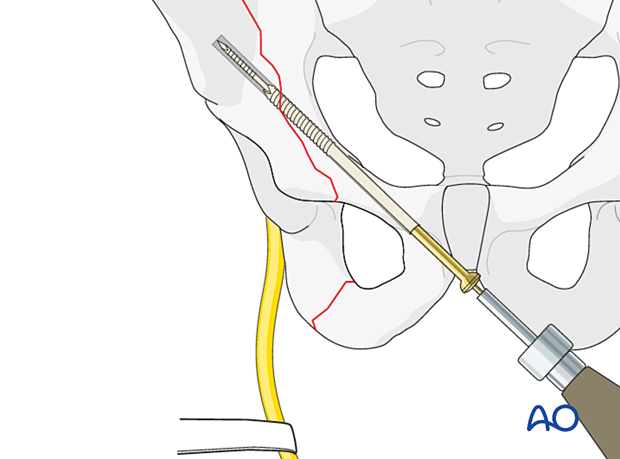
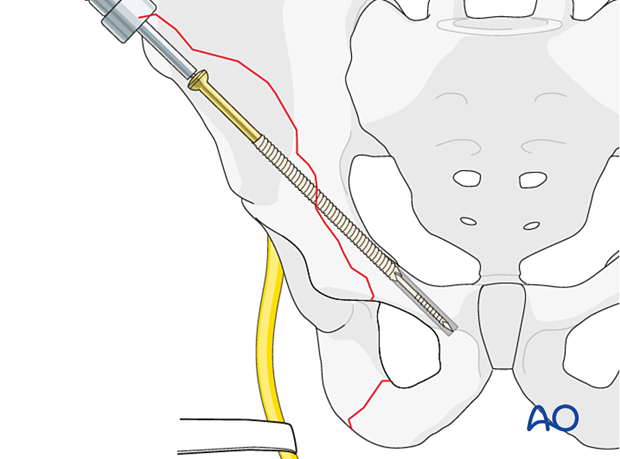
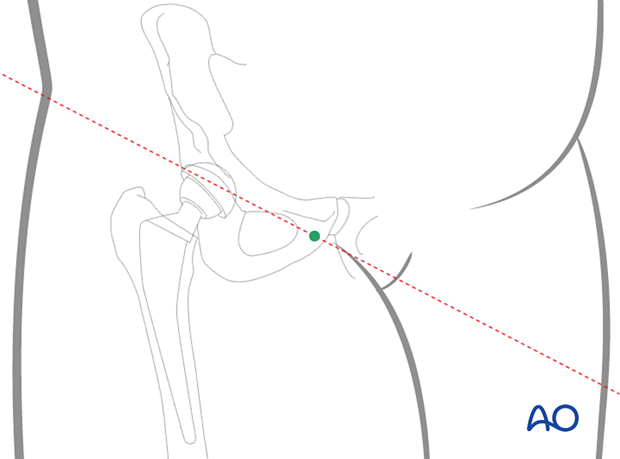
Percutaneous approach
The antegrade percutaneous approach is performed through a stab incision along with the outer table with the patient in a supine or lateral position.
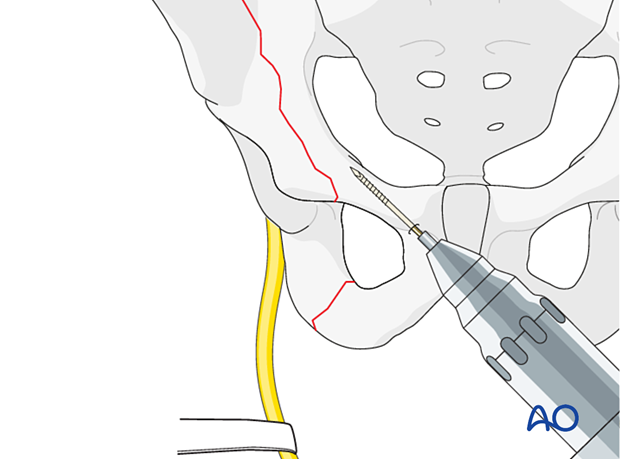
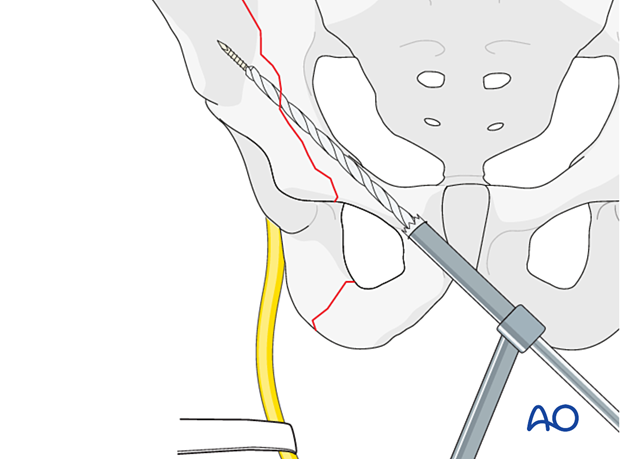
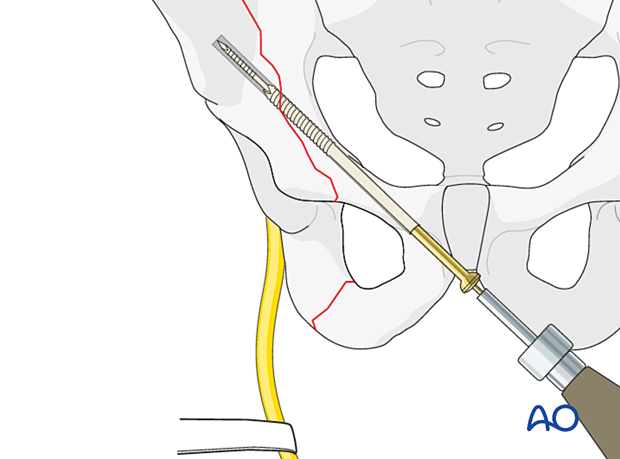
Anterior column fixation
A long guidewire is inserted, and its placement confirmed utilizing fluoroscopy or intraoperative CT.
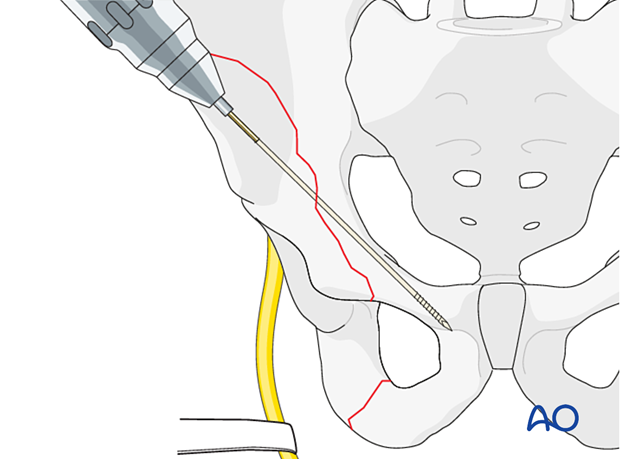
Consider drilling the entry point of the anterior column.
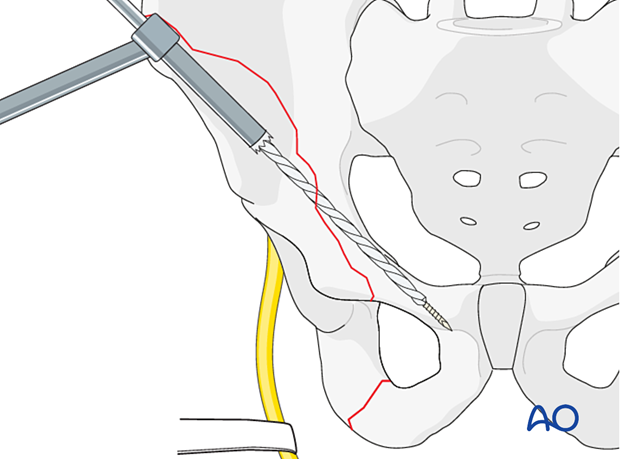
The screw is inserted over the guidewire.
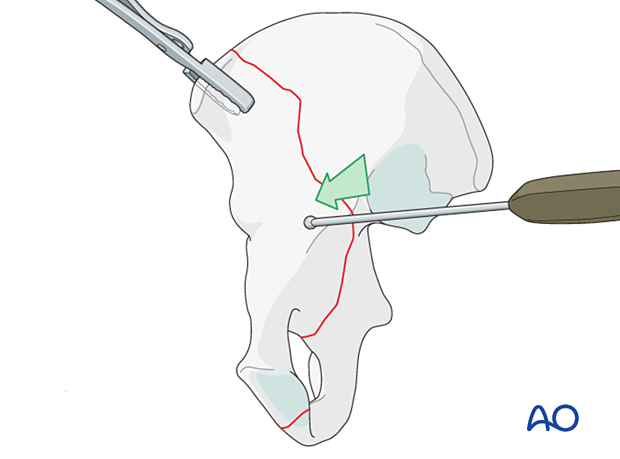
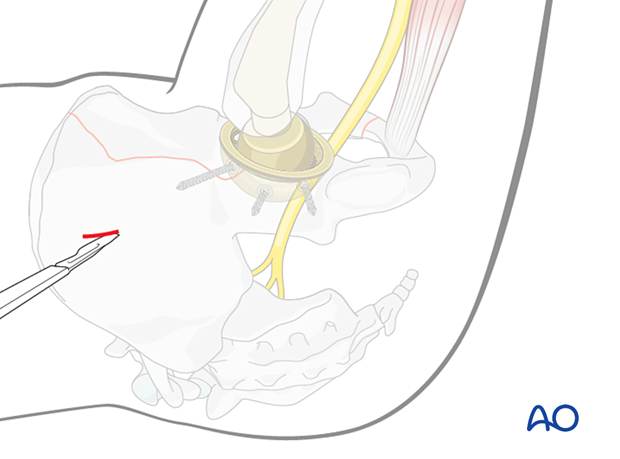
5. Screw application in retrograde fashion
When a fracture has been identified intraoperatively, effort should be made to utilize the surgical exposure that is already available.
Percutaneous approach
For this technique, the patient should be placed supine. The retrograde approach is performed through a stab incision past the midline to allow for entry at the pubic tubercle of the affected side.
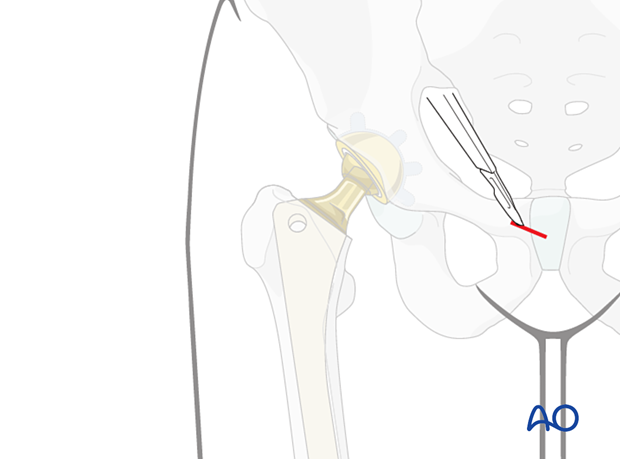
Anterior column fixation
A long guide-pin is inserted, and its placement confirmed utilizing fluoroscopy or intraoperative CT.
Consider drilling the entry point of the anterior column.
The screw is inserted over the guidewire.
6. Aftercare following ORIF
Postoperative management
Postoperative management should include careful monitoring of hematocrit and electrolytes particularly in the elderly patients.
Postoperative IV antibiotics should be administered up to 24 hours.
Consideration should be given to anticoagulation for a minimal course of 35 days. If there are thromboembolic complication this treatment is extended.
Drains can be discontinued when output is less than 30 to 50 cc per 12 hours.
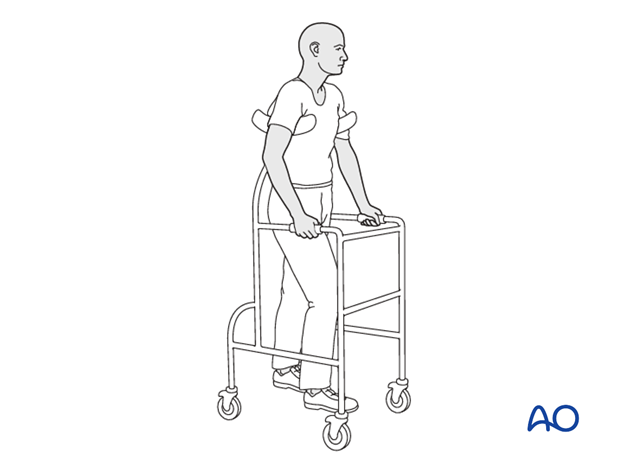
Patient mobilization
Immediate mobilization of the patient should commence. If fracture stability will allow, the patient should be made weight bearing as tolerated as soon as possible. Long periods of limited weight bearing are extremely detrimental to patient recovery.
Precautions against hip dislocation
Hip precautions can be extremely important in patients who have suffered intraoperative acetabular fracture. Much work has been done to minimize the surgical exposure during hip arthroplasty to decrease the risk of dislocation. These advantages are typically removed when acetabular stabilization need to be performed. A dislocation in the postoperative course of such a patient can be disastrous.
Patients are instructed to follow standard hip precautions against dislocation based upon the surgical approaches for hip arthroplasty.
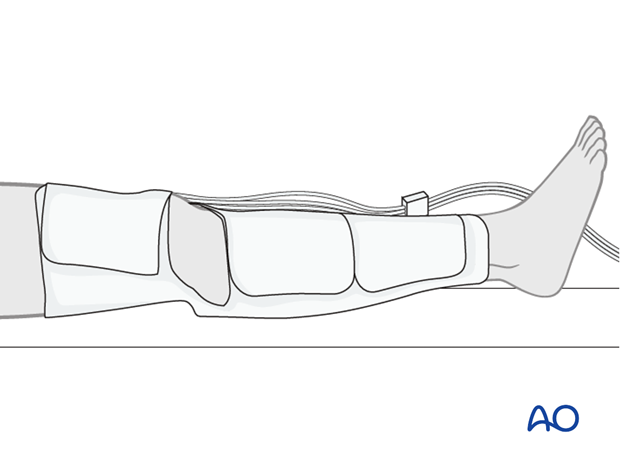
Wound healing
Avoidance of edema postoperatively is critical for both wound healing and patient mobilization. This can be aided by pneumatic compression devices. If negative pressure wound therapy is utilized, it can be discontinued after 5 to 7 days. Staples or sutures are typically removed at 14 to 21 days.