Open reduction - Plate fixation
1. General considerations
Introduction
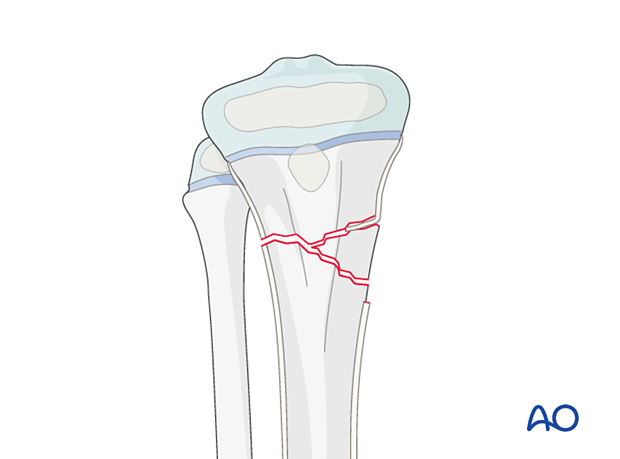
Unstable metaphyseal fractures can be managed with open reduction and plate fixation.
The plate position is dictated by the configuration of the fracture.
It may be necessary to span the physis in fractures with insufficient proximal metaphyseal length.
The use of locking head screws avoids compression of the perichondral ring.
The epiphyseal screws must be removed as soon as bone healing allows to prevent growth arrest and deformity.
Size and type of implant
2.0–4.5 mm plates are typically used in pediatric practice.
The age and weight of the patient, the anatomical site, and the load to which they will be subjected dictate the size of the implant.
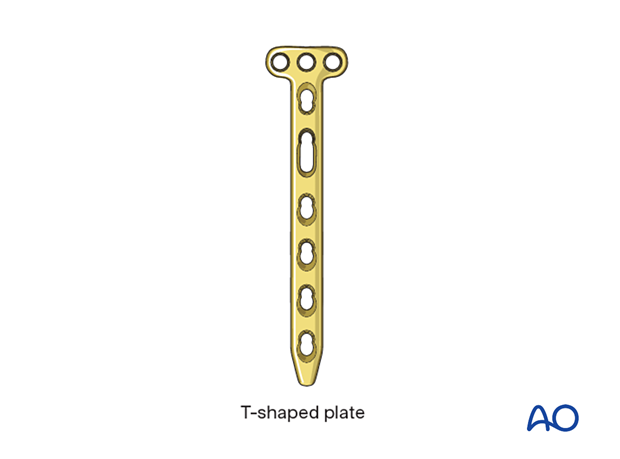
A T-shaped plate can be used.
Adult anatomic plates for the proximal tibia can be used in older children.
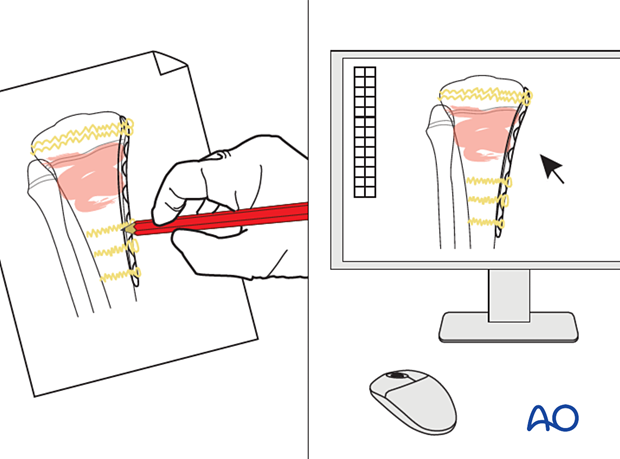
2. Preoperative planning
Preoperative planning is an essential part of the treatment of all proximal tibial fractures because of the variability of the fracture pattern and patient characteristics.
This involves:
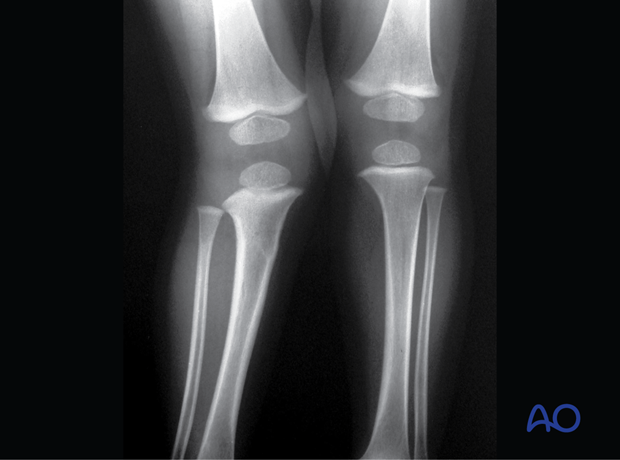
- Careful study of the x-rays
- Definition of the fracture fragments and the desired result. This may be achieved with appropriate software
- Choice of implants
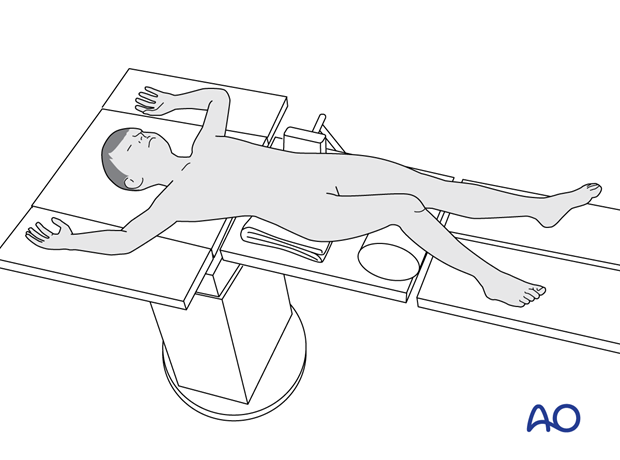
3. Patient preparation
Place the patient in a supine position on a radiolucent table, with a bolster under the ipsilateral flank.
Breaking the table to allow knee flexion may facilitate traction and reduction.
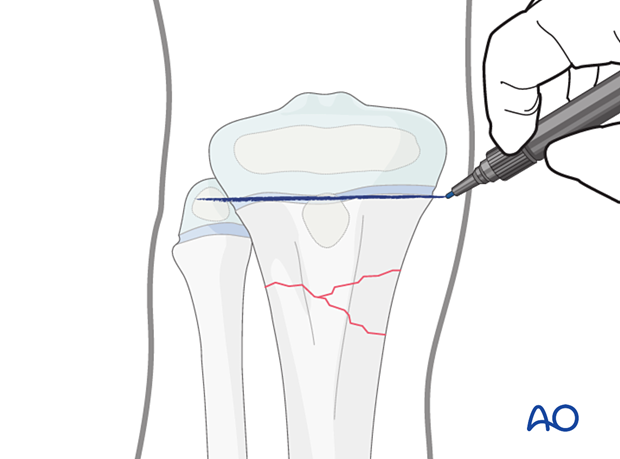
4. Approaches
Confirm the location of the physis with an image intensifier and protect the perichondral ring and adjacent periosteum.
The approach is dictated by the fracture pattern.
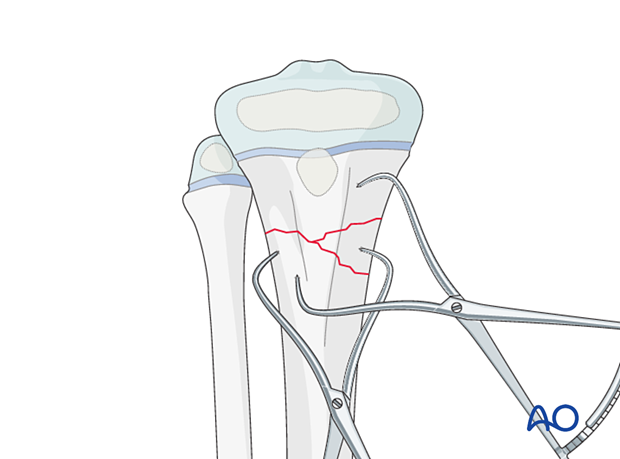
5. Reduction
Removal of impediments
It may be necessary to remove interposed soft tissue and periosteum without devitalizing the fracture fragments.
This is performed under direct vision, prior to fracture reduction.
Reduction maneuvers
Reduction can be performed with:
- Pointed reduction forceps
- A Hohmann retractor, used as a lever to correct translation
- K-wires, used as a joystick to control the distal fragment
If needed, temporarily stabilize the fracture with K-wire(s).
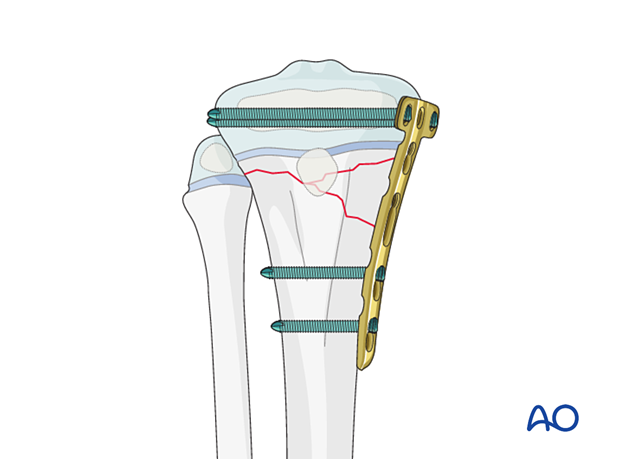
6. Plate fixation
Apply the plate in a standard manner.
Multifragmentary fractures often require bridge plating.
Plate application
Contour the plate to match the anatomy of the proximal tibia.
Take care to position the plate so that it does not interfere with the distal insertion of the hamstring muscles.
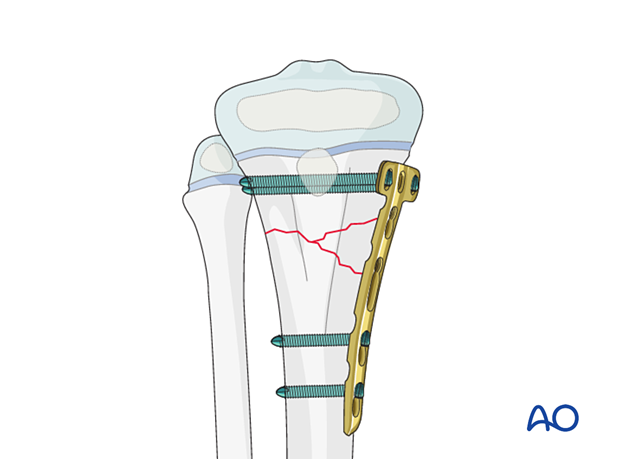
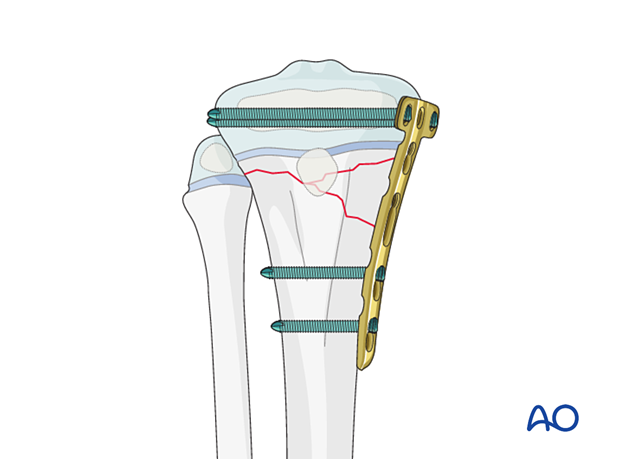
Place the plate so that the proximal screws can be inserted into the epiphysis, parallel to the physis.
Hold the plate to the bone with K-wires or reduction forceps.
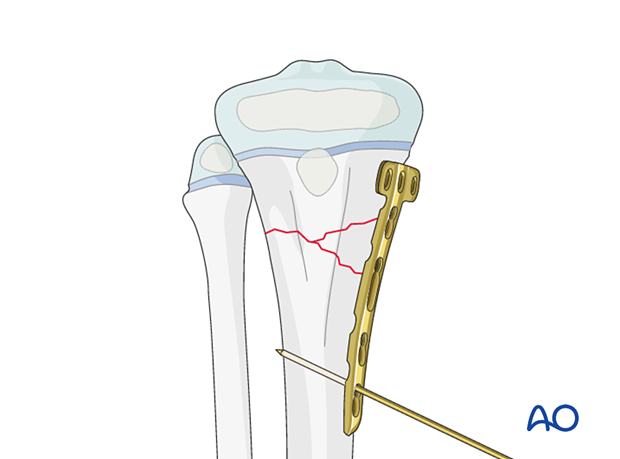
Screw insertion
The periosteum and perichondral ring should not be disturbed.
Before screw insertion, ensure that both plate ends are aligned and have good contact with the bone. Check the tibial alignment with an image intensifier before screw insertion.
The order of screw insertion depends on the fracture configuration.
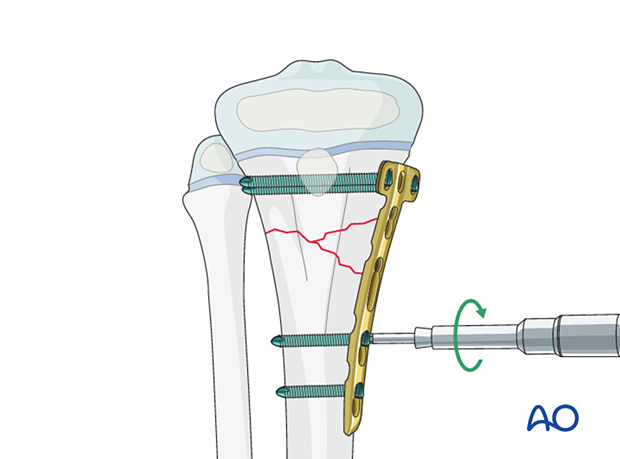
Physeal spanning plate
If the plate spans the physis, the perichondral ring should be protected with a dissector or elevator to offset the plate during locking screw insertion.
Locking screws should be used adjacent to the physis to prevent compression of the perichondral ring.
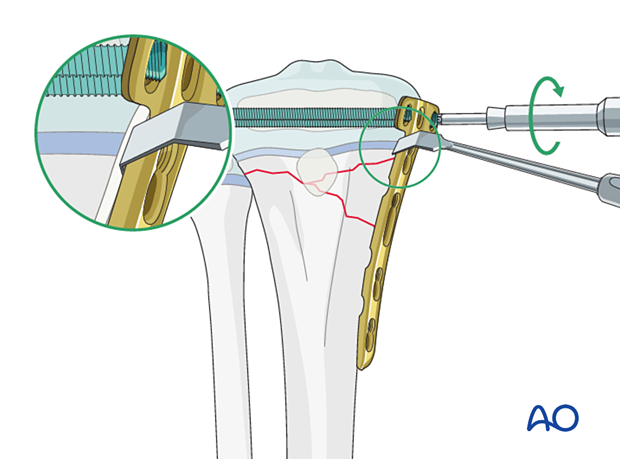
Before screw insertion, ensure that both plate ends are aligned and have good contact with the bone. Check the tibial alignment with an image intensifier before screw insertion.
Remove the dissector or elevator after screw fixation.
7. Final assessment
Confirm fracture reduction and implant position with an image intensifier.
8. Application of a splint
In a patient compliant with weight-bearing restrictions, no additional casting is necessary.
A splint with the knee flexed 30°–45° may be applied for comfort in the early postoperative period.
9. Aftercare
Immediate postoperative care
The patient is kept touch-weight bearing.
Older children may be able to use crutches or a walker.
Younger children may require a period of mobilization in a wheelchair.
If no cast has been applied, range of motion exercises can be started immediately.
Neurovascular examination
The patient should be examined frequently in the initial period following the injury, to exclude neurovascular compromise or evolving compartment syndrome.
High-energy fractures are associated with vascular injuries and require careful clinical assessment.
Follow-up
The first clinical and radiological follow-up is usually undertaken at 4–6 weeks.
Mobilization
Weight bearing can be started when clinical and radiological signs suggest a stable fracture, typically 3–4 weeks after injury.
Implant removal
Early implant removal should be performed after clinical and radiographic confirmation of fracture consolidation to avoid growth arrest.
Alternatively, if there is remaining growth, the epiphyseal screws should be removed after initial fracture healing. The remaining implant may be removed later if necessary.
Follow-up for growth disturbance and deformity
All patients with fractures of the proximal tibia should have clinical and radiological examination 8–12 weeks postoperatively to confirm healing and alignment.
Clinical examination should be repeated at intervals for at least one year to detect early signs of growth disturbance.
If there is a clinically relevant leg length discrepancy or malalignment, radiological assessment is required.
Check for valgus deformity which may develop over several months with greenstick fractures (Cozenʼs phenomenon). This occurs in younger patients and usually improves within 2 years of injury.