Open reduction - Screw fixation
1. General considerations
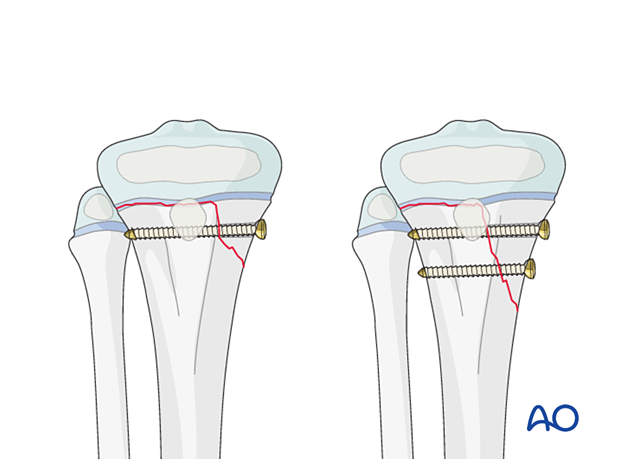
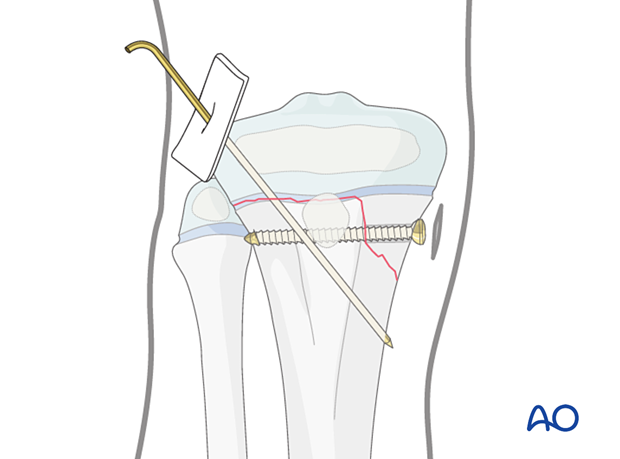
A Salter-Harris type-II fracture may be fixed with a lag screw through the metaphyseal (Thurstan Holland) fragment, parallel to the physis.
If the Thurstan Holland fragment is large enough, two screws may be used.
Closed vs open reduction
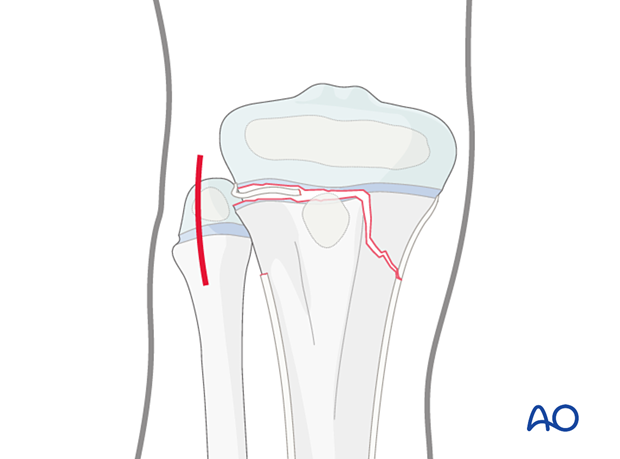
If initial closed reduction is unsuccessful, this is usually due to periosteum entrapped on the side that has failed in tension.
Salter-Harris II fractures with metaphyseal comminution may be reduced closed but conversion to an open procedure may be necessary.
2. Instruments and implants
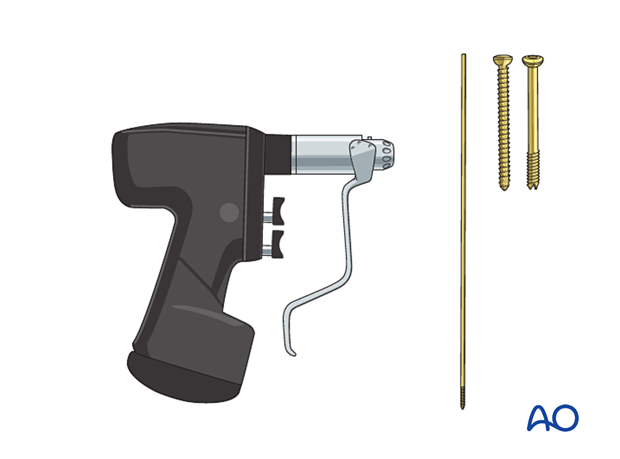
Appropriately sized cannulated or noncannulated lag screws (2.7–5.0 mm) can be used.
The following equipment is used:
- Screw set or cannulated screw set
- Drill
- Image intensifier
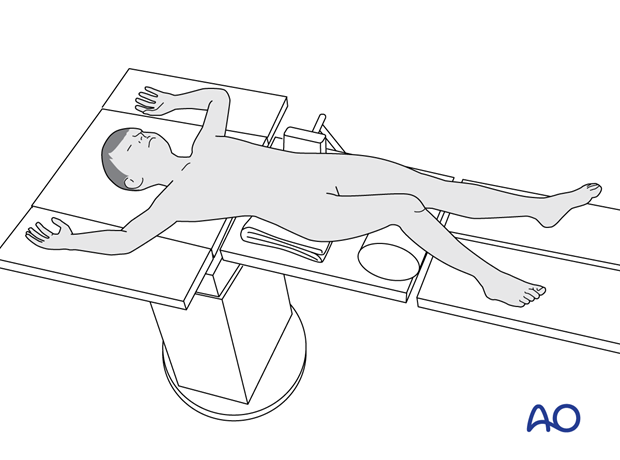
3. Patient preparation
Place the patient in a supine position on a radiolucent table, with a bolster under the ipsilateral flank.
Breaking the table to allow knee flexion may facilitate traction and reduction.
4. Approaches
The approach is dictated by the fracture pattern and location of the block to reduction (eg, periosteum). Screws may be inserted percutaneously.
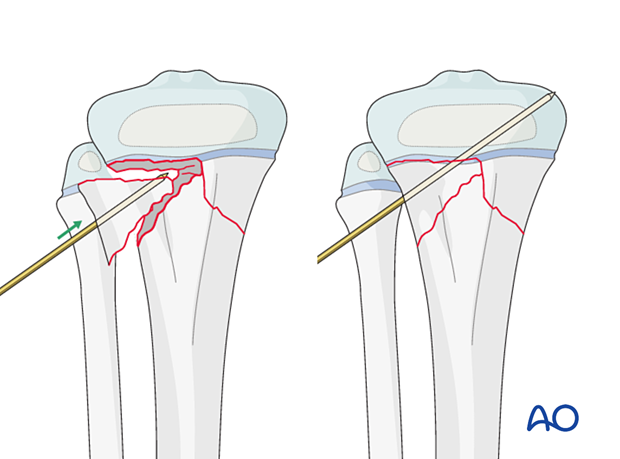
5. Reduction
If acceptable closed reduction cannot be obtained, proceed with an open reduction on the opposite side to the Thurston Holland fragment.
Direct reduction should be possible after removal of entrapped soft tissue or bone fragments with a ball spike pusher or a partially inserted K-wire.
The reduction may also be performed and maintained with reduction forceps.
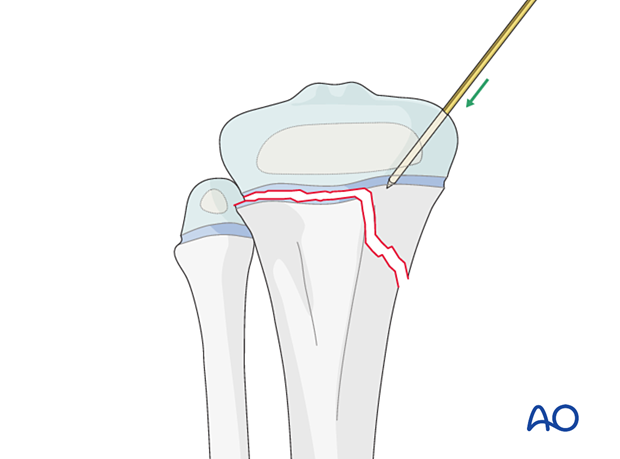
A displaced metaphyseal fragment of a multifragmentary fracture may be reduced with a percutaneous K-wire as a joystick and temporarily stabilized.
6. Fixation
Incision
Perform a stab incision at the level of the planned screw insertion.
Spread the underlying soft tissues with blunt dissection and place a soft-tissue protector down to the bone.
Insert the guide wire.
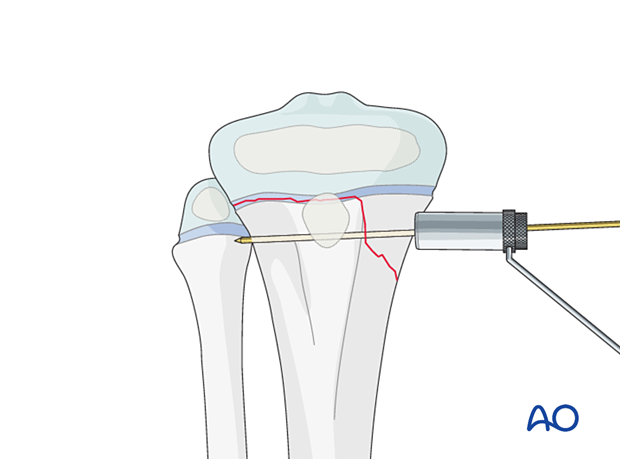
Screw insertion
Insert a lag screw parallel to the physis starting in the center of the metaphyseal fragment, in a standard manner.
If the metaphyseal fragment is sufficiently large, insert two screws.
Confirm reduction, fracture stability, and screw placement with an image intensifier prior to removal of the guide wire.
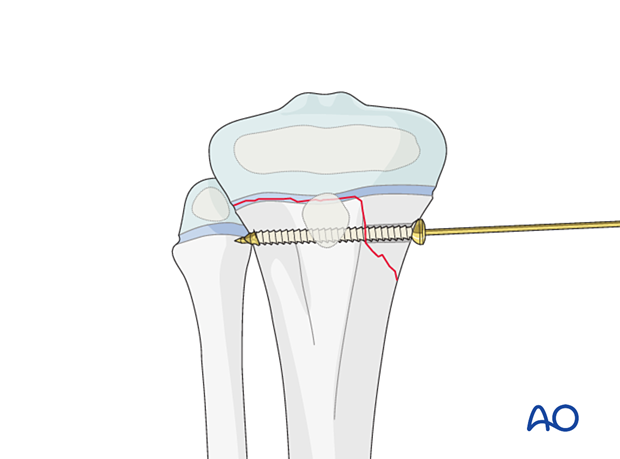
Insertion of a K-wire
If there are concerns about the stability, insert an additional K-wire across the physis to stabilize the physeal component of the fracture.
7. Final assessment
Confirm fracture reduction and implant position with an image intensifier.
8. Application of a cast
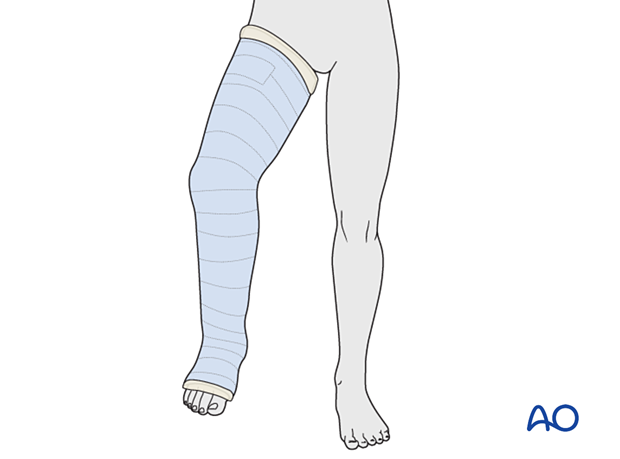
In a patient compliant with weight-bearing restrictions, no additional casting is necessary.
A long leg cast with the knee flexed 30°–45° may be necessary for 3–6 weeks.
9. Aftercare
Immediate postoperative care
The patient is kept touch-weight bearing.
Older children may be able to use crutches or a walker.
Younger children may require a period of mobilization in a wheelchair.
If no cast has been applied, range of motion exercises can be started immediately.
Neurovascular examination
The patient should be examined frequently in the initial period following the injury, to exclude neurovascular compromise or evolving compartment syndrome.
High-energy fractures are associated with vascular injuries and require careful clinical assessment.
Follow-up
The first clinical and radiological follow-up is usually undertaken at 4–6 weeks.
Mobilization
Weight bearing can be started when clinical and radiological signs suggest a stable fracture, typically 3–4 weeks after injury.
Implant removal
A K-wire is typically removed 3–6 weeks after injury.
Screw removal is optional and can be performed at least 3–4 months after injury.
Follow-up for growth disturbance
All patients with fractures of the proximal tibia should have clinical and radiological examination 8–12 weeks postoperatively to confirm healing and alignment.
Clinical examination should be repeated at intervals for at least one year to detect early signs of growth disturbance.
If there is a clinically relevant leg length discrepancy or malalignment, radiological assessment is required.













