Open reduction - K-wire fixation
1. General considerations
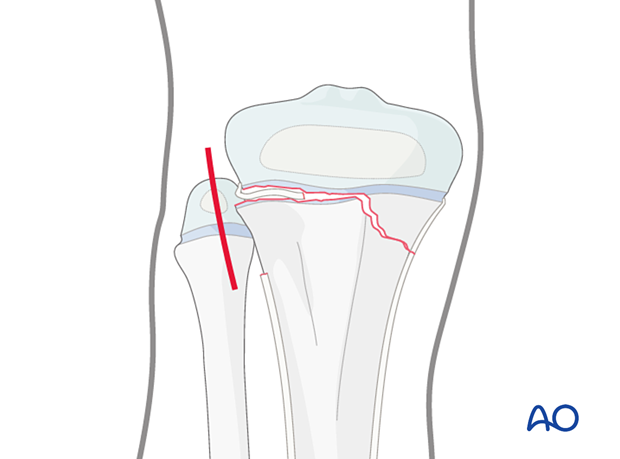
This technique is used after open reduction of proximal tibial fractures including Salter-Harris I–IV, and proximal metaphyseal fractures in patients with open tibial physis.
These fracture patterns require temporary fixation across the physis to produce adequate stability.
To minimize secondary damage to the physis, manipulation must be gentle.
Multiple passes across the physis with a K-wire should be avoided.
Smooth, narrow K-wires reduce the risk of physeal damage.
Threaded K-wires may increase fracture stability.
Closed vs open reduction
If initial closed reduction is unsuccessful, this is usually due to periosteum entrapped on the side that has failed in tension.
Salter-Harris II fractures with metaphyseal comminution may be reduced closed but conversion to an open procedure may be necessary.
2. Instruments and implants
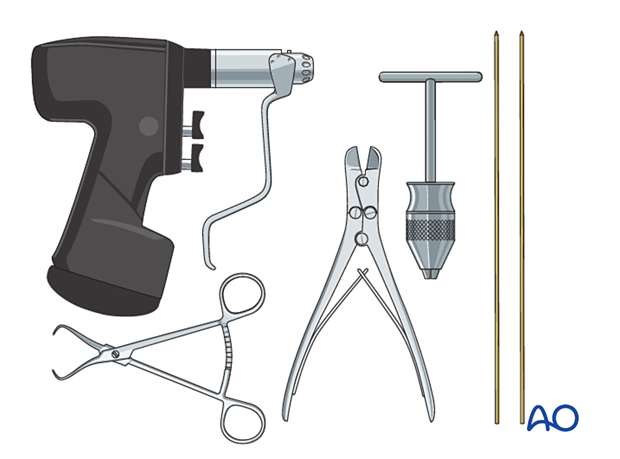
The following equipment is needed:
- K-wires of appropriate sizes
- Drill or a T-handle for manual insertion
- Wire cutting instruments
- Standard orthopedic instrument set
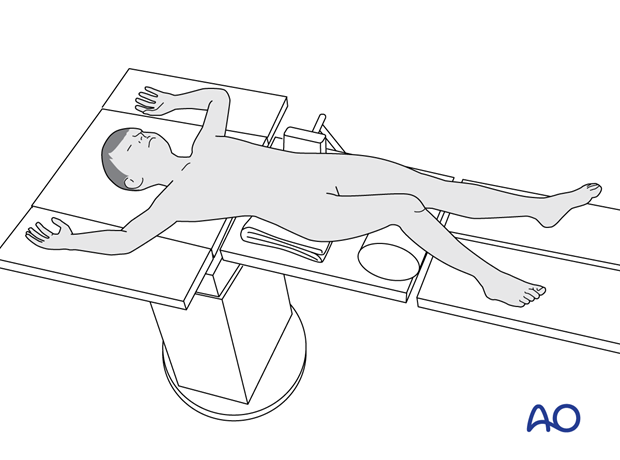
3. Patient preparation
Place the patient in a supine position on a radiolucent table, with a bolster under the ipsilateral flank.
Breaking the table to allow knee flexion may facilitate traction and reduction.
4. Approaches
For open reduction of a Salter-Harris II fracture, the approach should be on the side of the metaphyseal fragment. Wires may be inserted percutaneously.
5. Reduction
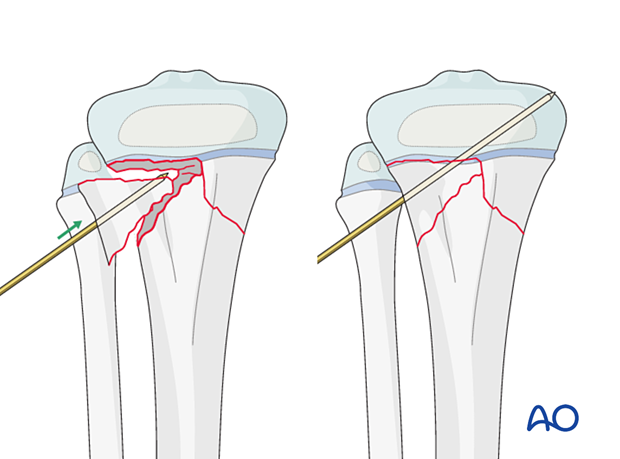
If acceptable closed reduction cannot be obtained, proceed with an open reduction on the opposite side to the Thurston Holland fragment.
Direct reduction should be possible after removal of entrapped soft tissue or bone fragments with a ball spike pusher or a partially inserted K-wire.
The reduction may also be performed and maintained with reduction forceps.
A displaced metaphyseal fragment of a multifragmentary fracture may be reduced with a percutaneous K-wire as a joystick.
If the direction of the K-wire allows, this can be used for definitive fixation.
6. Fixation
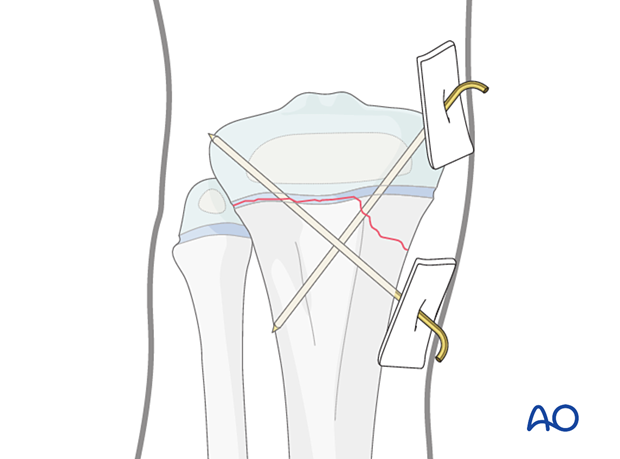
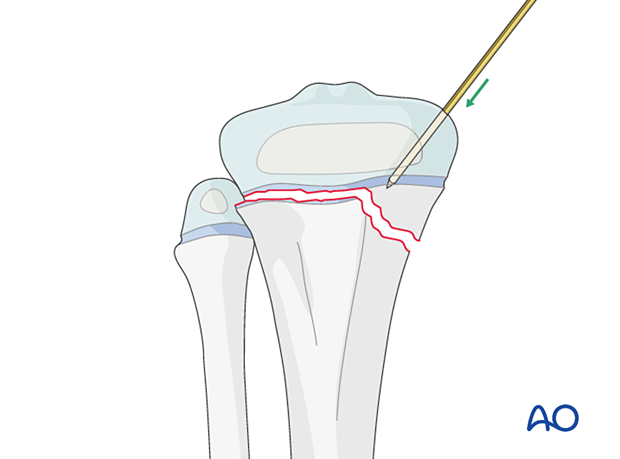
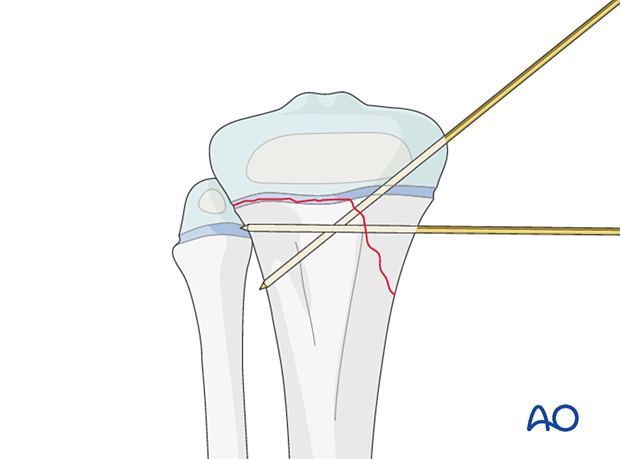
Insertion of K-wires
Insert the first K-wire from proximal to distal starting medially.
Advance the K-wire across the physis after confirming a trajectory that will engage the metaphysis of the proximal tibia on AP and lateral views.
Engage the K-wire in the cortical bone of the tibia.
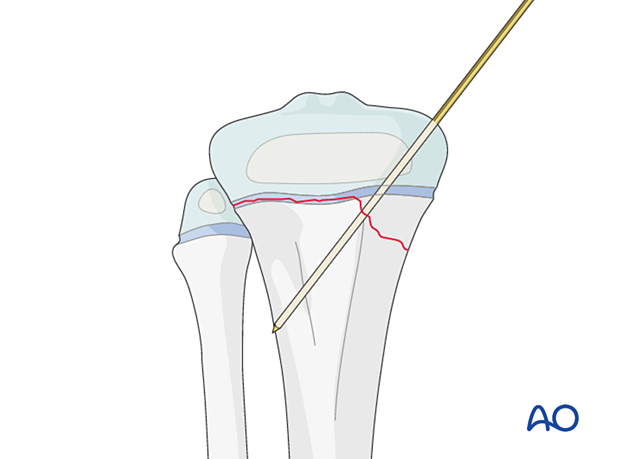
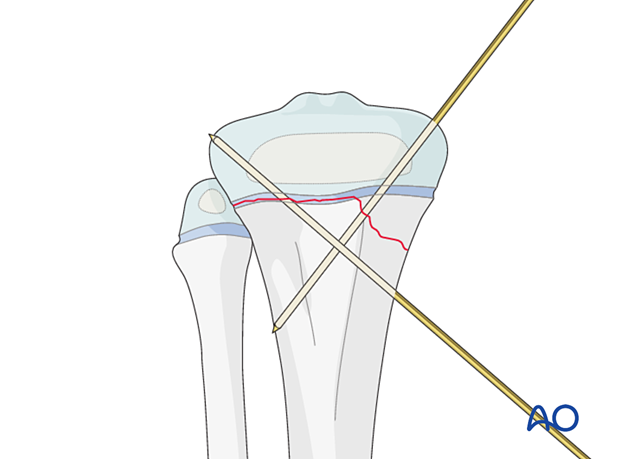
The second K-wire may be inserted from distal to proximal from the medial side to avoid injury to the common peroneal nerve.
Take care not to penetrate the articular surface with the tip of the K-wire.
If the metaphyseal fragment is large enough, the second K-wire may be inserted in the metaphyseal region parallel to the physis. Take care not to injure the peroneal nerve.
In either case, maximize the spread of the K-wires at the fracture site to increase stability.
Confirm stability of fracture fixation with an image intensifier.
In multifragmentary fractures, a third K-wire may be required if there is persistent instability.
Repair the joint capsule with absorbable sutures. Close the skin and subcutaneous tissues according to surgeon preference.
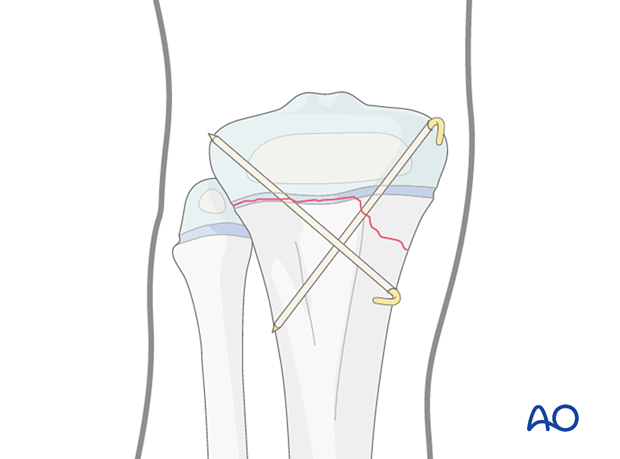
K-wire cutting and dressing
Bend the K-wires approximately 2 cm from the skin to accommodate for swelling as illustrated.
Cut the K-wires and apply a dressing or sponge to stabilize the K-wires against the skin.
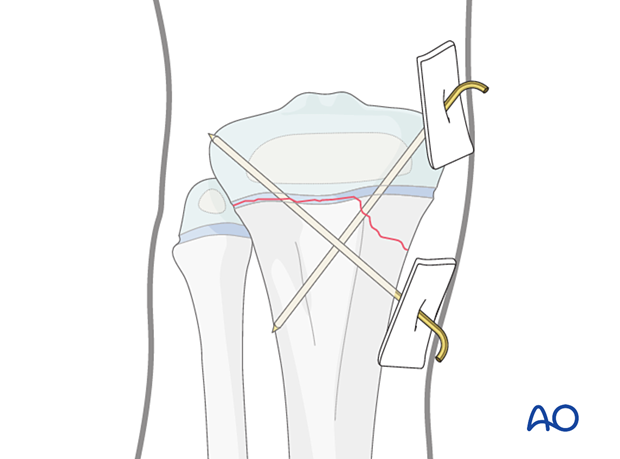
K-wires may be buried under the skin, but this requires further surgery for wire removal.
7. Final assessment
Confirm fracture reduction and implant position with an image intensifier.
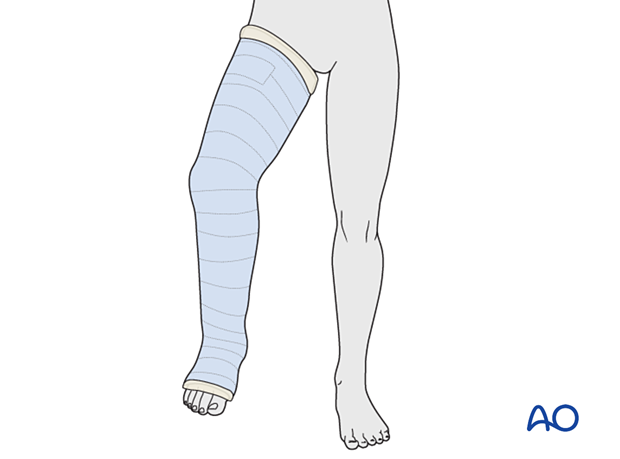
8. Immobilization
A cast is mandatory because K-wires in isolation are inadequate to neutralize muscle forces.
Apply a long leg cast with the knee flexed to 30°–45° for 3–6 weeks, depending on the age of the patient.
9. Aftercare
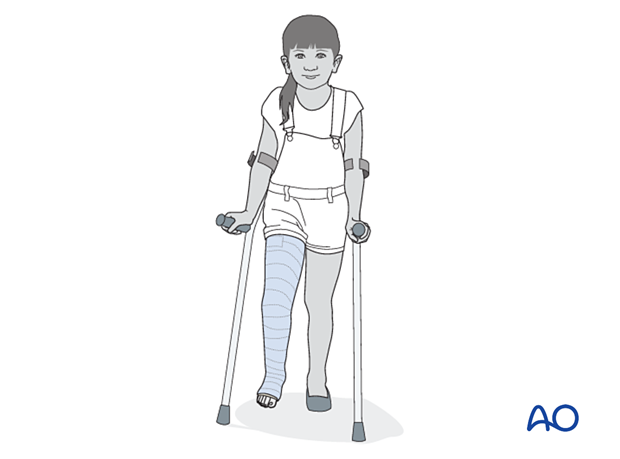
Immediate postoperative care
The patient is kept touch-weight bearing.
Older children may be able to use crutches or a walker.
Younger children may require a period of mobilization in a wheelchair.
Neurovascular examination
The patient should be examined frequently in the initial period following the injury, to exclude neurovascular compromise or evolving compartment syndrome.
High-energy fractures are associated with vascular injuries and require careful clinical assessment.
Follow-up, cast and K-wire removal
These fractures heal quickly, and cast and K-wires are typically removed, following an x-ray, 3–6 weeks after injury.
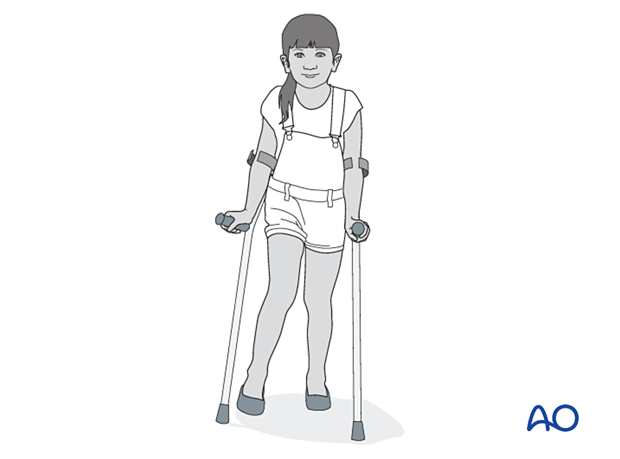
Mobilization
Once K-wires and cast are removed, partial weight-bearing and knee range-of-motion exercises are started with gradual return to normal activity.
Follow-up for growth disturbance
All patients with fractures of the proximal tibia should have clinical and radiological examination 8–12 weeks postoperatively to confirm healing and alignment.
Clinical examination should be repeated at intervals for at least one year to detect early signs of growth disturbance.
If there is a clinically relevant leg length discrepancy or malalignment, radiological assessment is required.













