Open reduction - K-wire fixation
1. General considerations
This technique is used after open reduction of proximal tibial Salter-Harris I–IV fractures, and proximal metaphyseal fractures in patients with an open tibial physis.
These fracture patterns require temporary fixation across the physis to produce adequate stability.
To minimize secondary damage to the physis, manipulation must be gentle.
Multiple passes across the physis with a K-wire should be avoided.
Smooth, narrow K-wires reduce the risk of physeal damage.
Threaded K-wires may increase fracture stability.
It is mandatory to achieve anatomical reduction of the articular surface to preserve joint function. Open reduction is therefore often necessary.
The main goals of treatment of these fractures are to:
- Restore joint congruity
- Minimize injury to the physis
- Prevent secondary displacement
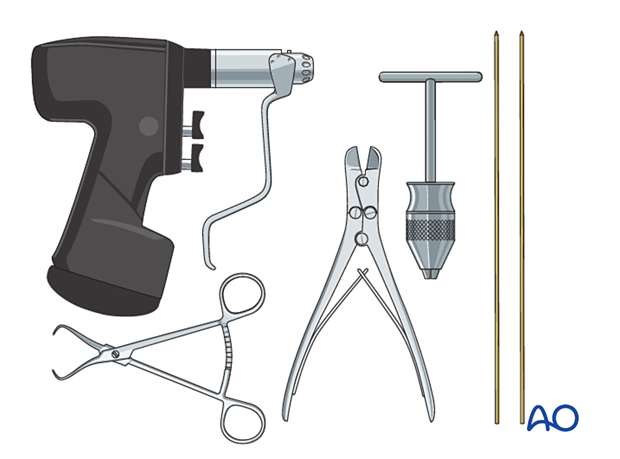
2. Instruments and implants
The following equipment is needed:
- K-wires of appropriate sizes
- Drill or a T-handle for manual insertion
- Wire cutting instruments
- Standard orthopedic instrument set
3. Patient preparation
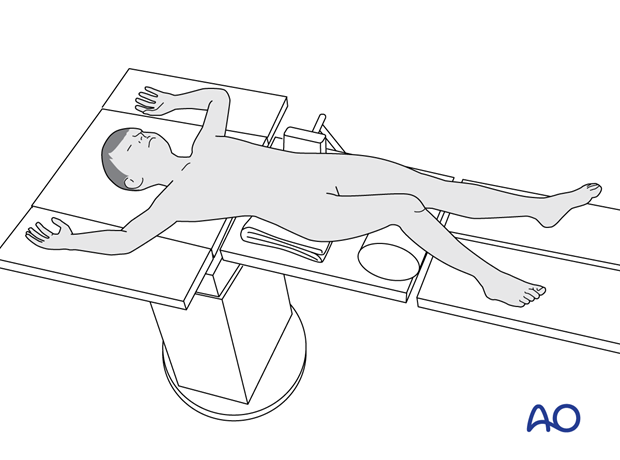
Place the patient in a supine position on a radiolucent table, with a bolster under the ipsilateral flank.
Breaking the table to allow knee flexion may facilitate traction and reduction.
4. Approaches
A medial, anteromedial, or anterolateral approach may be used, depending on fracture pattern. Wires may be inserted percutaneously.
Assessment of the articular surface may be performed either with an arthrotomy or arthroscopy.
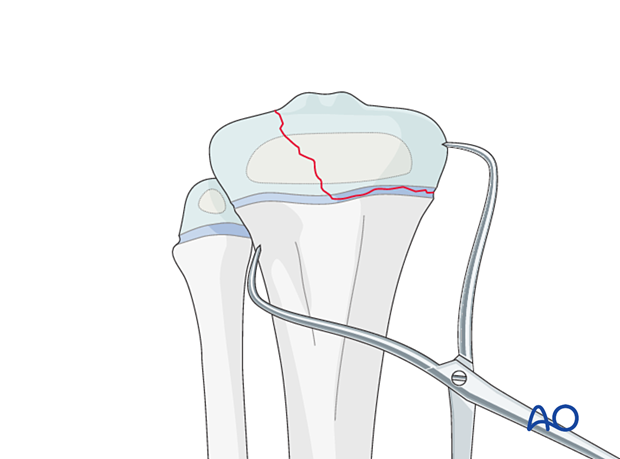
5. Reduction
Direct reduction should be possible after removal of entrapped soft tissue or bone fragments and maintained with reduction forceps.
Confirm anatomical reduction with an image intensifier.
If there is any doubt about the accuracy of reduction of the articular surface, an arthrotomy or arthroscopy may be needed.
6. Fixation
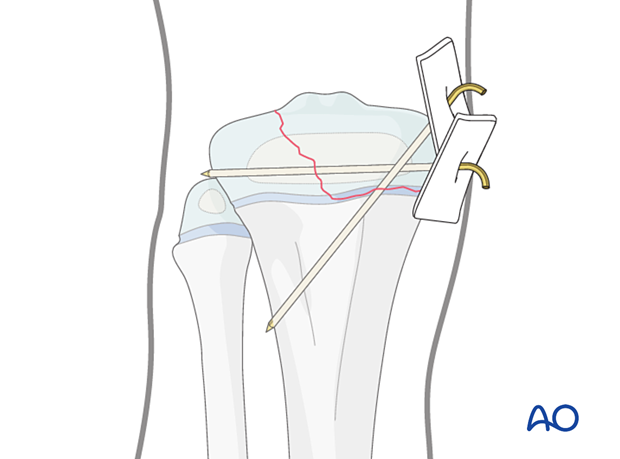
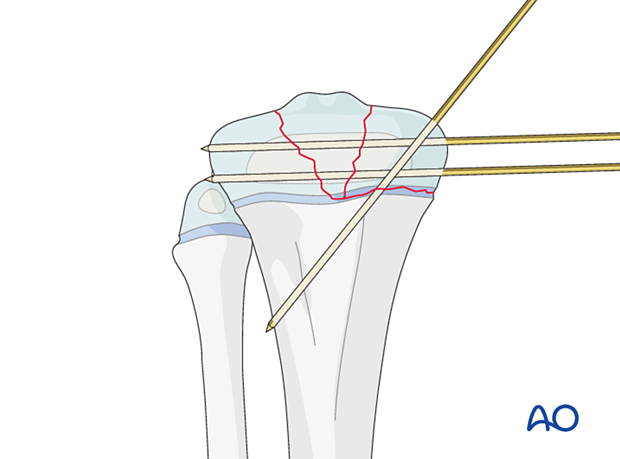
Insertion of K-wires
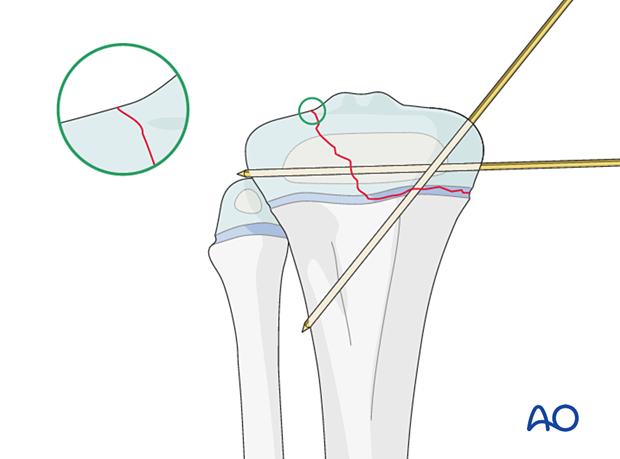
Insert the first K-wire in the epiphysis, parallel to the physis to maintain anatomical reduction of the articular surface.
This wire is usually inserted from the medial side.
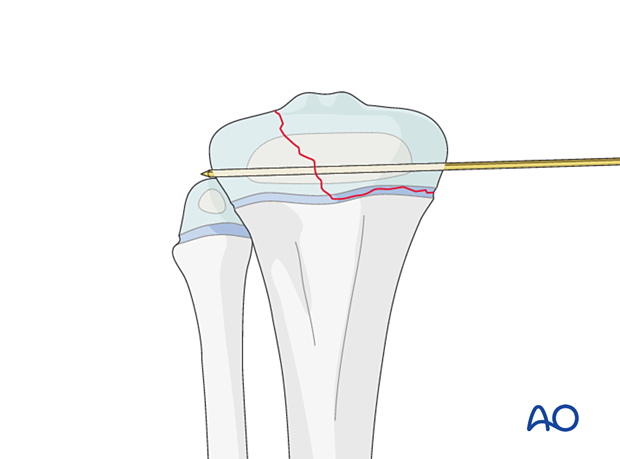
Insert a second K-wire across the physis after confirming a trajectory that will engage the metaphysis of the proximal tibia with AP and lateral image intensifier views.
Engage the K-wire in the cortical bone of the tibia.
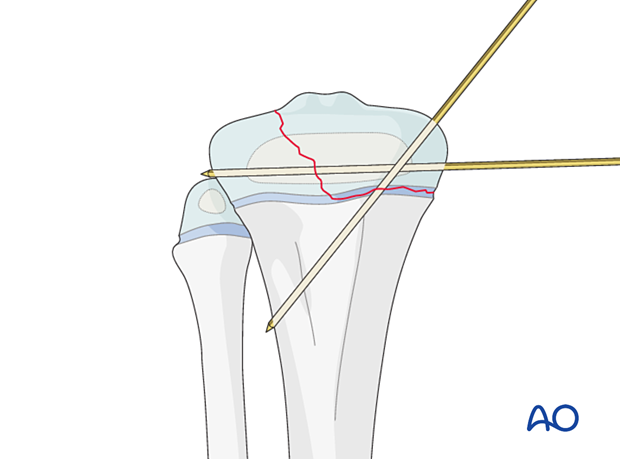
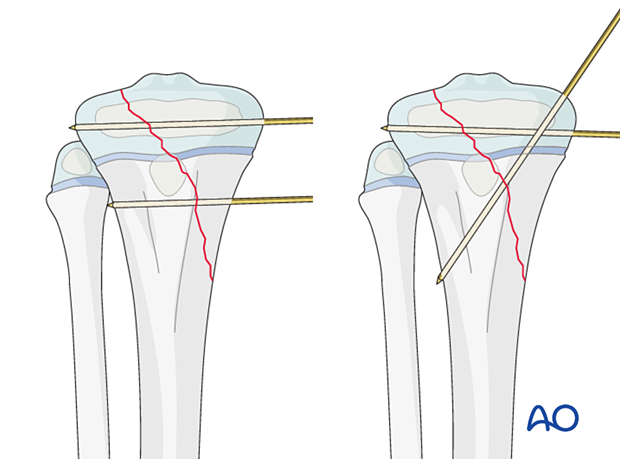
If the epiphyseal component is small, a second, parallel K-wire may be used.
In either case, maximize the spread of the K-wires at the fracture site to increase stability.
Confirm stability of fracture fixation with an image intensifier.
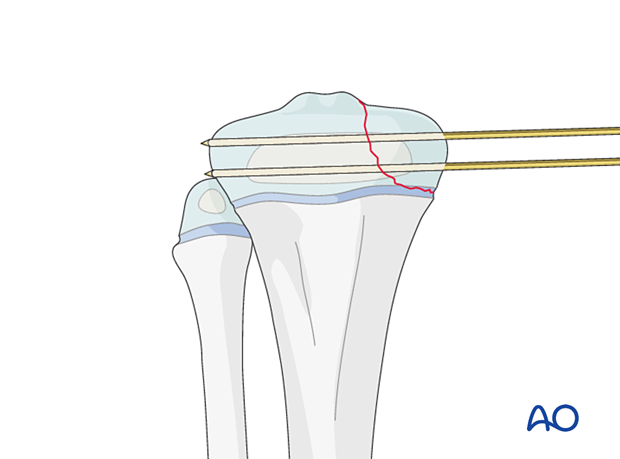
If the epiphyseal fragment is comminuted, K-wire fixation of the articular surface should engage all fragments.
Repair the joint capsule with absorbable sutures. Close the skin and subcutaneous tissues according to surgeon preference.
In Salter-Harris IV fractures, the trajectory of a second K-wire depends on the metaphyseal fracture pattern and may be parallel to the physis or directed from proximal to distal crossing the physis.
Advance the K-wire across the physis after confirming a trajectory that will engage the metaphysis of the proximal tibia on AP and lateral views.
Engage the K-wire in the cortical bone of the tibia.
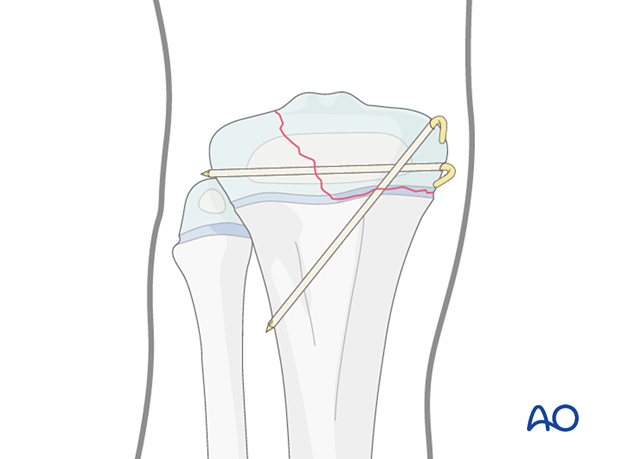
K-wire cutting and dressing
Bend the K-wires approximately 2 cm from the skin to accommodate for swelling as illustrated.
Cut the K-wires and apply a dressing or sponge to stabilize the K-wires against the skin.
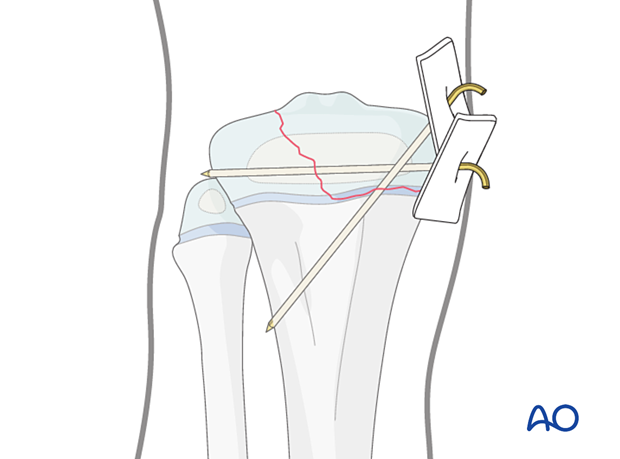
K-wires may be buried under the skin, but this requires further surgery for wire removal.
7. Final assessment
Confirm fracture reduction and implant position with an image intensifier.
8. Immobilization
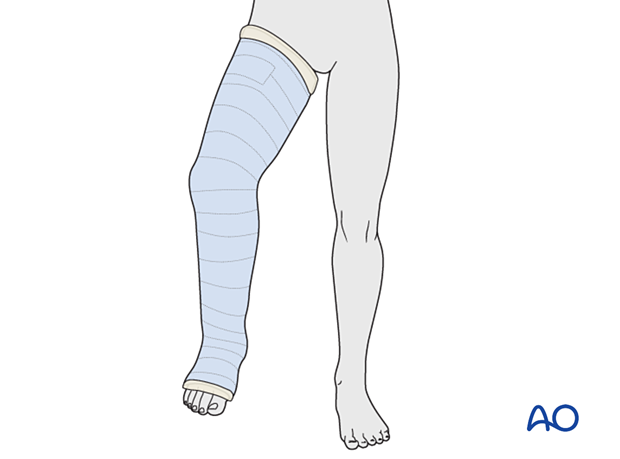
A cast is mandatory because K-wires in isolation are inadequate to neutralize muscle forces.
Apply a long leg cast with the knee flexed to 30°–45° for 3–6 weeks, depending on the age of the patient.
9. Aftercare
Immediate postoperative care
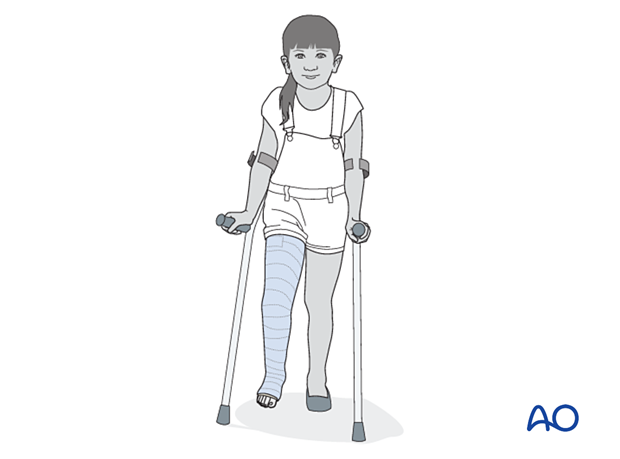
The patient is kept touch-weight bearing.
Older children may be able to use crutches or a walker.
Younger children may require a period of mobilization in a wheelchair.
Neurovascular examination
The patient should be examined frequently in the initial period following the injury, to exclude neurovascular compromise or evolving compartment syndrome.
High-energy fractures are associated with vascular injuries and require careful clinical assessment.
Follow-up, cast and K-wire removal
These fractures heal quickly, and cast and K-wires are typically removed, following an x-ray, 3–6 weeks after injury.
Mobilization
Once K-wires and cast are removed, partial weight-bearing and knee range-of-motion exercises are started with gradual return to normal activity.
Follow-up for growth disturbance
All patients with fractures of the proximal tibia should have clinical and radiological examination 8–12 weeks postoperatively to confirm healing and alignment.
Clinical examination should be repeated at intervals for at least one year to detect early signs of growth disturbance.
If there is a clinically relevant leg length discrepancy or malalignment, radiological assessment is required.













