Open reduction - Lag-screw fixation
1. General considerations
The majority of these fractures are displaced due to the force of the quadriceps through the patellar tendon and require open reduction.
Fractures with smaller fragments may require repair with tension band fixation.
Goal of the surgery:
- Reattachment of the avulsed fragment with the patellar tendon
- Anatomical reduction in intraarticular fracture types
- Reconstruction of soft-tissue injury
This fracture is usually accompanied with a large soft-tissue injury.
These injuries are occasionally associated with compartment syndrome and frequent clinical assessment is mandatory in the early period following the injury.
There is a risk of anterior growth arrest leading to an apex posterior (extension) deformity, particularly in younger patients.
2. Patient preparation
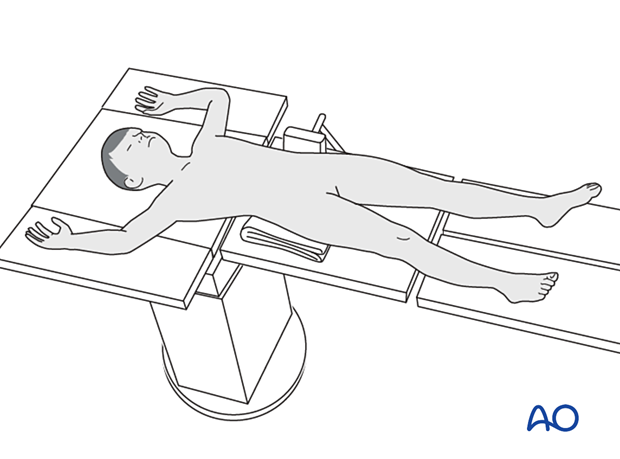
Place the patient in a supine position without traction on a radiolucent table with the knee extended.
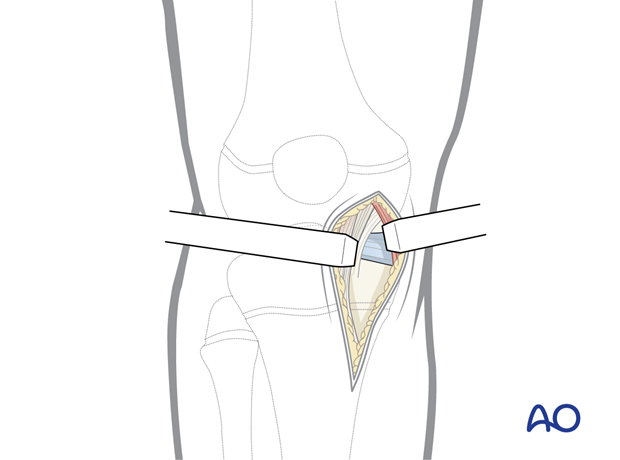
3. Approach
This procedure is commonly performed with a medial parapatellar incision but a lateral parapatellar incision may provide better exposure and depends on the fracture configuration.
4. Reduction
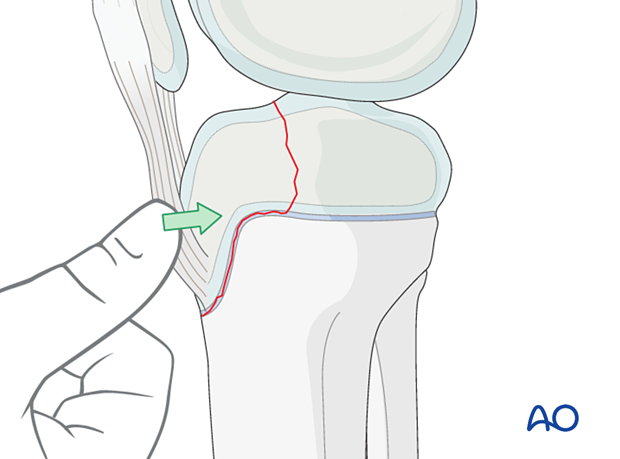
Reduction may be achieved by hyperextending the knee.
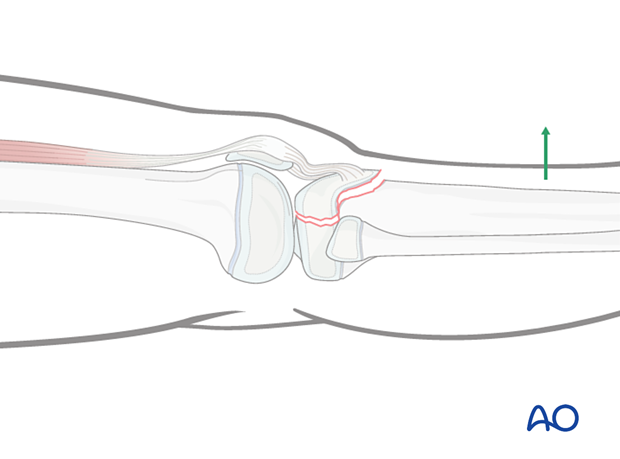
Reduce the fracture by direct pressure to manipulate the fragment into the correct position.
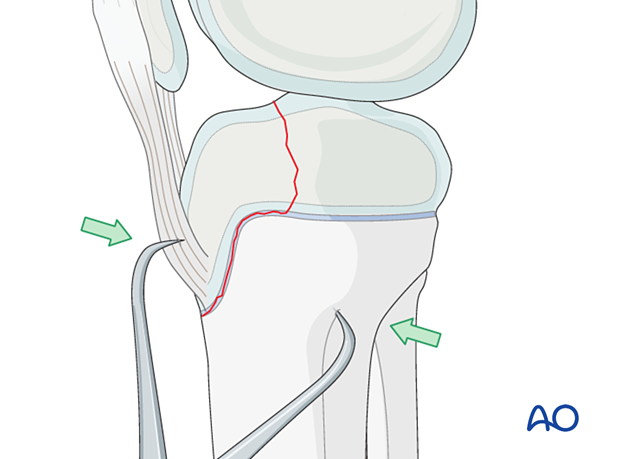
If this is not successful, a small reduction forceps placed on the anterior tibial cortex and the bone fragment …
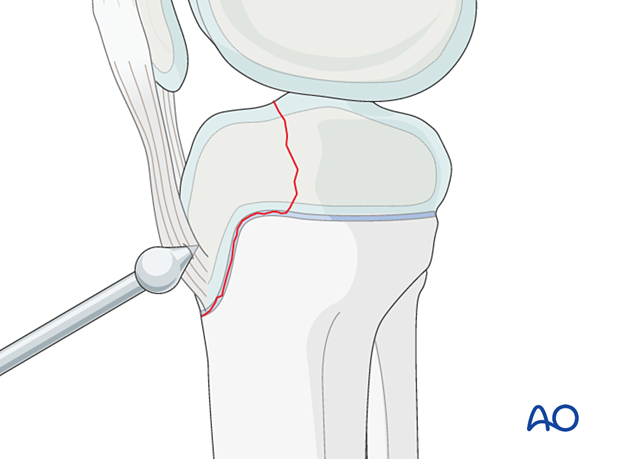
… or a ball-spike pusher may be used.
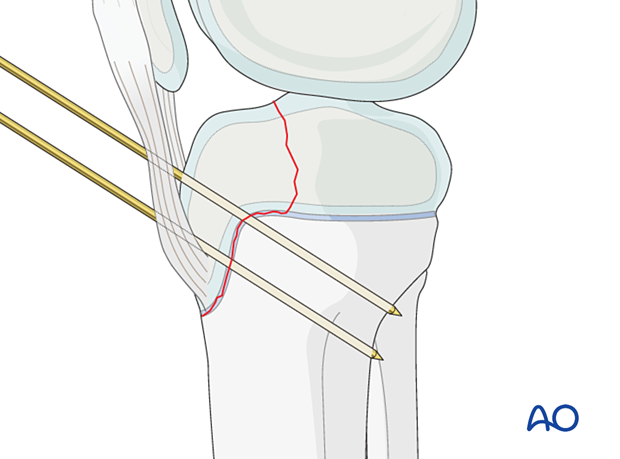
The reduction may also be secured with temporary K-wires.
Reduction of the articular surface
An arthroscopic approach may be useful. This is limited to inserting a camera to visualize the articular surface and assist with its reduction.
Alternatively, a limited arthrotomy may be considered to specifically visualize the articular surface.
5. Screw fixation
Knee flexion for drilling
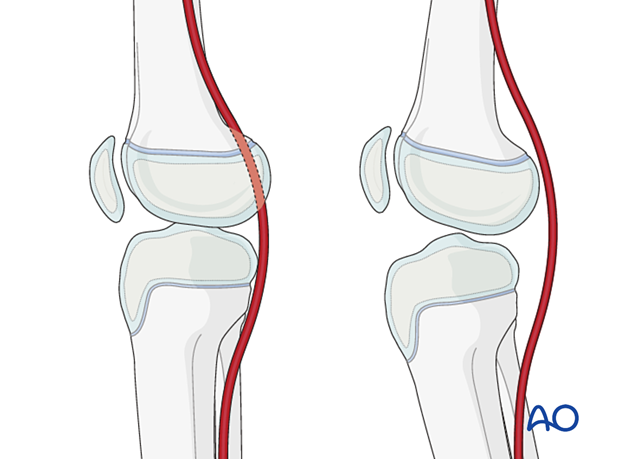
The neurovascular bundle is closely related to the bone in full extension.
Flex the knee 15°–20° to reduce the likelihood of damage to the popliteal neurovascular structures.
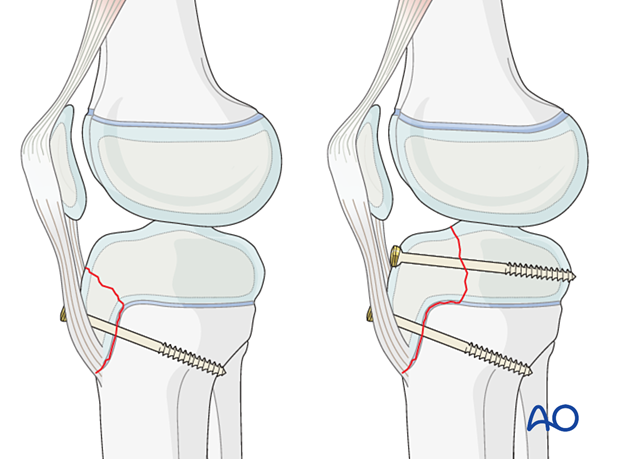
Lag screw insertion
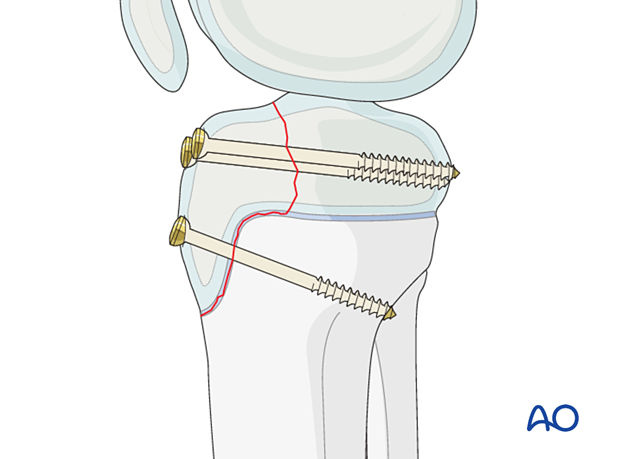
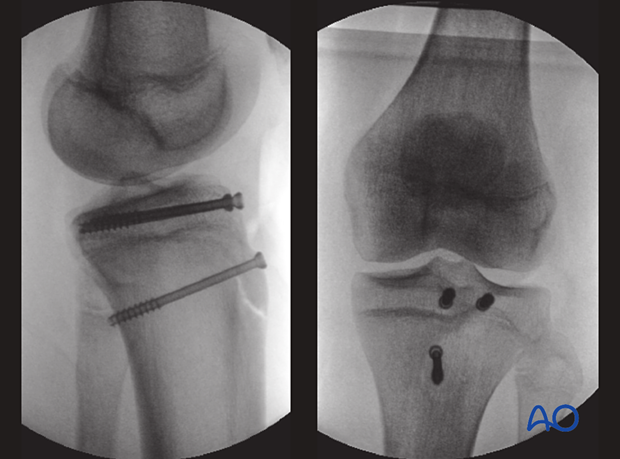
Insert two or three lag screws in an AP direction, depending on the size of the fragment.
Optimal compression can be achieved with bicortical insertion of a screw with sufficient diameter.
Select a screw that is the correct length for bicortical engagement but avoid a longer screw to reduce the risk of injury to the popliteal neurovascular structures.
The type of fracture is most commonly seen in adolescents approaching skeletal maturity.
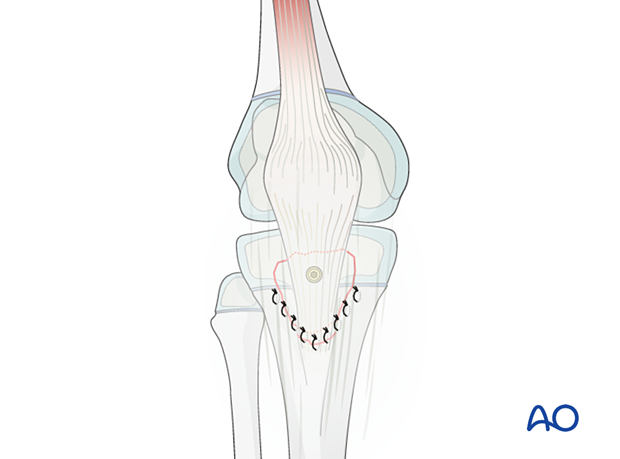
Soft-tissue reconstruction
The soft tissues of the extensor apparatus are commonly avulsed with the apophysis and require reconstruction after stabilization of the fracture.
6. Final assessment
Check reduction of the fragment, the implant position, and tension of the patellar tendon under direct vision and with an image intensifier.
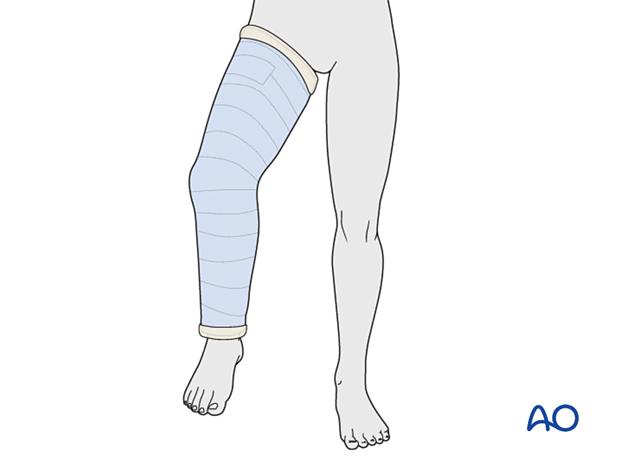
7. Immobilization
Depending on fixation stability, fracture size and soft-tissue damage, a cylinder cast with the knee flexed 20°–30° should be applied for 4 weeks.
The patient is kept touch-weight bearing.
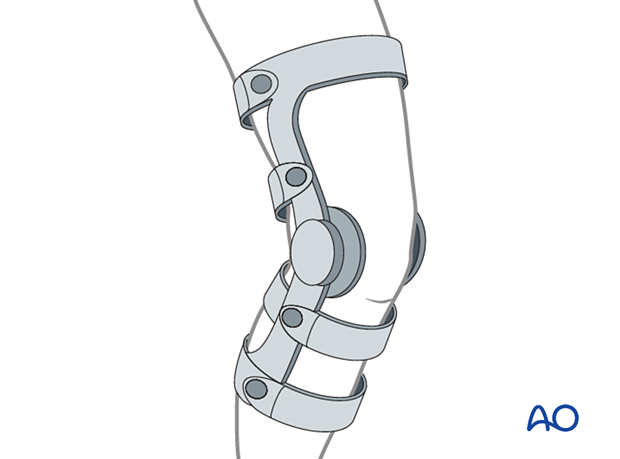
Alternatively, a hinged knee brace may be used with a gradually increasing range of motion over 4 weeks, with the patient instructed to remain touch-weight bearing.
8. Aftercare
Neurovascular examination
The patient should be examined frequently, to exclude neurovascular compromise or evolving compartment syndrome in the period immediately following the injury.
Follow-up
The first clinical and radiological follow-up is usually undertaken after 6 weeks to confirm consolidation of the fracture.
Growth disturbance is not common as the fracture generally occurs in patients close to skeletal maturity. In younger patients, growth disturbance is more likely and requires close clinical follow-up.
Bony overgrowth at the apophysis is possible and may lead to local irritation or pain.
Implant removal
Implants should be removed after 3–6 month if there is continuing growth. They may also be removed if they are causing local irritation.













