Deltopectoral interval approach to the proximal humerus
1. Indication
The (anterior) deltopectoral approach can be used for most proximal humeral fractures as it allows access to all relevant structures.
Usually there is no need for the adult extensile approach and the approach is limited to management of interposed soft-tissue and fracture reduction.
2. Anatomy
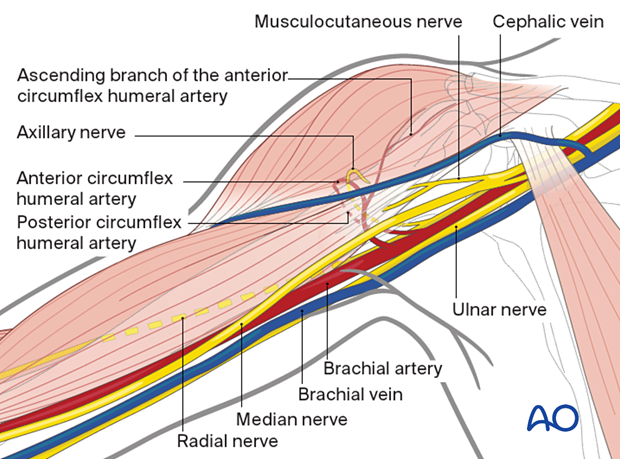
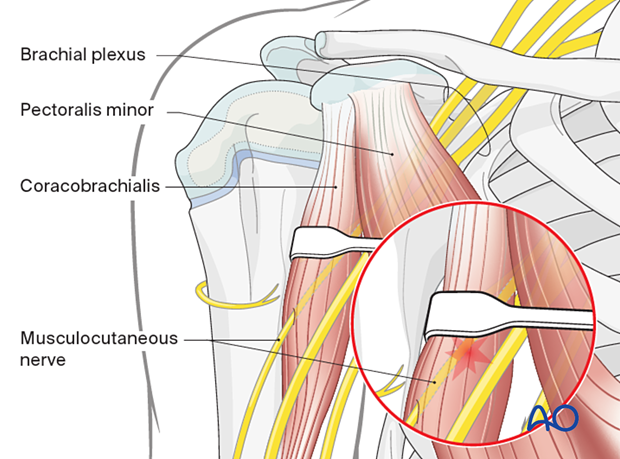
The course of the following neurovascular structures should be appreciated:
- Cephalic vein
- Anterior circumflex humeral artery
- Ascending branch of the anterior circumflex humeral artery
- Posterior circumflex humeral artery
- Musculocutaneous nerve
- Axillary nerve
Additional neurovascular structures, eg, the brachial plexus, are only at risk if there is excessive traction.
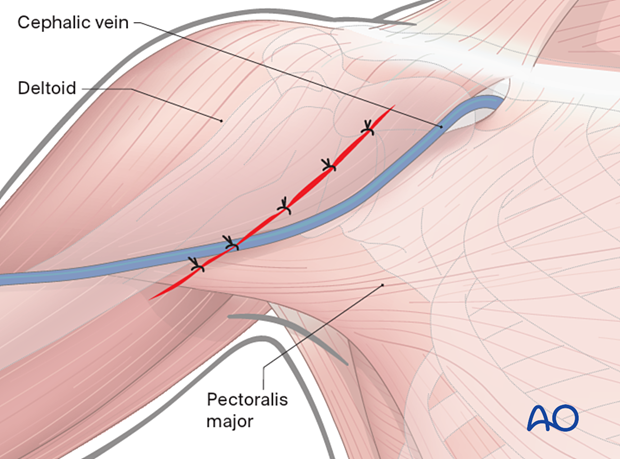
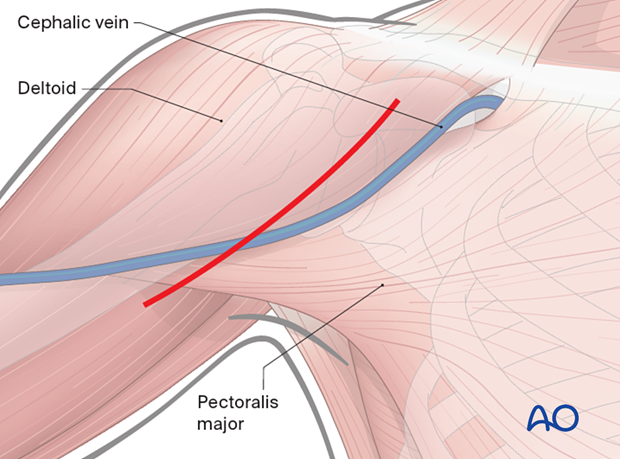
3. Skin incision
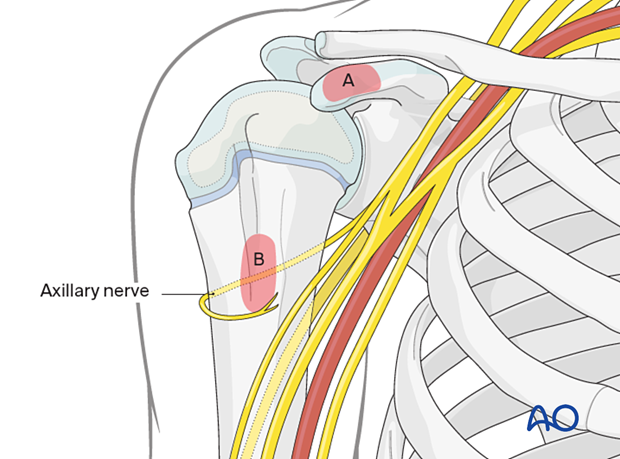
Anatomical landmarks for the anterior deltopectoral approach are:
- Coracoid process (A)
- Proximal humeral shaft (B; at the level of the axilla)
Both landmarks can easily be palpated.
Make a skin incision between the coracoid process and the proximal humeral shaft. This can be straight or curved depending on surgeon’s preference.
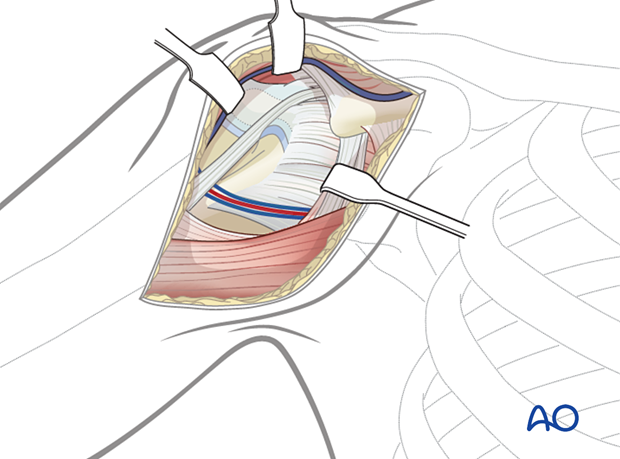
4. Exposure of the superficial fascia
Expose the deltopectoral groove with the cephalic vein. These structures can be identified by:
- The course of the muscle fibers
- The cephalic vein itself
- Fat tissue surrounding the vein
If in doubt, look for the deltopectoral groove at the proximal and/or distal end of the skin incision.
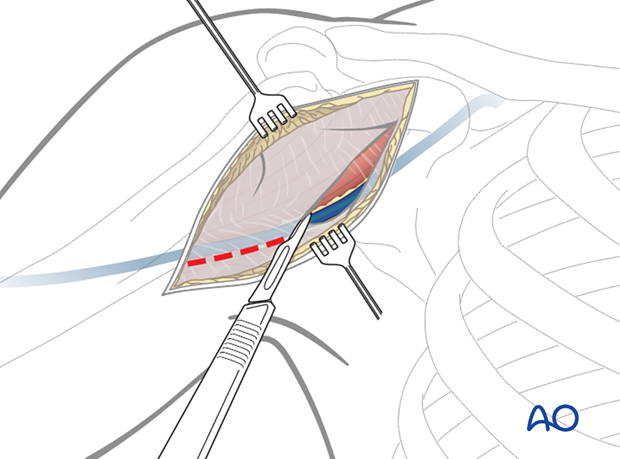
5. Dissection down to the deltopectoral groove
Retract the cephalic vein laterally or medially, and open the fascial layer along the groove. If retracted laterally, the anatomical drainage of blood from the deltoid muscle is respected but it is at risk of damage by retractors during surgery. In any case, the cephalic vein should be preserved to reduce surgical edema of the limb.
Failure to identify the deltopectoral groove can lead to difficulty in dissection of the deltoid and possibly to denervation of the anterior portion of the deltoid.
Use blunt dissection between and under the deltoid and pectoralis muscles to expose the clavipectoral fascia.
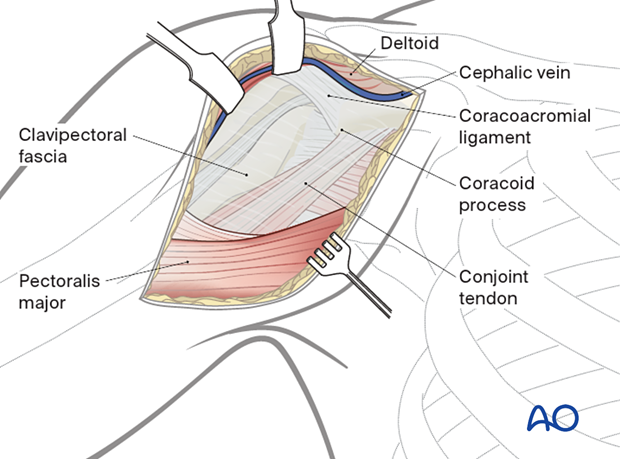
6. Exposure of the deep layers
Identify the coracoid process and the conjoint tendon.
Incise the clavipectoral fascia lateral to the conjoined tendon and inferior the coracoacromial ligament.
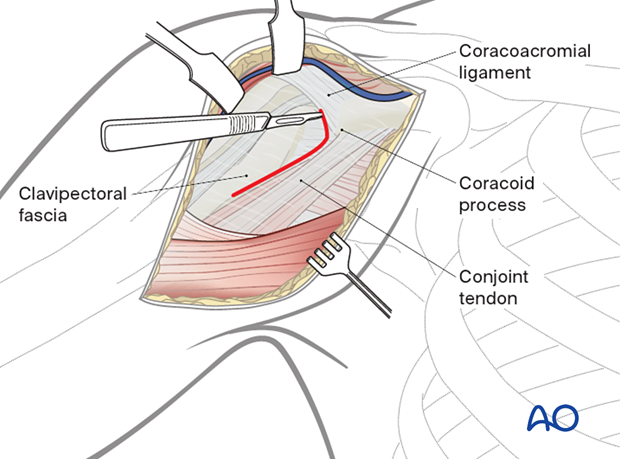
Retract the deltoid muscle laterally using a delta (modified Hohmann) retractor and the conjoined tendon medially using a Langenbeck retractor.
Expose the proximal humerus and confirm the anatomical landmarks (subscapularis tendon, lesser tuberosity, bicipital groove with the biceps tendon and the greater tuberosity). Evaluate the fracture morphology. Hemorrhagic bursa tissue may be resected if necessary.
Distally, expose the pectoralis major.

7. Wound closure
Irrigate the wound.
Close the deltopectoral groove, the subcutaneous tissues and the skin.